805
Views & Citations10
Likes & Shares
The present article discusses the creation of an
elderly care model. Population aging caused by demographic and epidemiological
changes in Brazil, a relatively recent phenomenon, requires an efficient
response. Based on a critical analysis of healthcare models for the elderly,
the text presents a proposal for the healthcare of this age group, with
emphasis on low intensity levels of care, focusing on health promotion and
prevention, in order to avoid overload in the system. Integrated care models
aim to solve the problem of fragmented and poorly coordinated care in current
health systems. The more health professionals know about the history of their
patients, the better the results. This is how the contemporary and resolutive
models of care recommended by most major national and international health
agencies should function. A higher quality, more resolutive and cost-effective
care model is the focus of the present study.
INTRODUCTION
The recent phenomenon of population aging in
Brazil, caused by demographic and epidemiological changes, requires an
effective response. Based on a critical analysis of healthcare models for the
elderly, we propose the creation of a model entitled Caring Senior, emphasizing
low-intensity levels of care, focusing on health promotion and prevention, in
order to avoid burdening the system. Integrated care models aim to solve the
problem of the fragmented and poorly coordinated care that currently prevails
in health systems. We advocate an approach that prioritizes low-intensity
interventions and constant monitoring, through different care settings, as
recommended by most major national and international health agencies, which
include: integrated medical treatment, with a flowing process of educational
actions, health promotion, prevention of preventable diseases, delayed onset of
illness, early care intervention and rehabilitation from sickness.
POPULATION AGING IN
BRAZIL AND IN THE WORLD
One of humankind’s greatest achievements has
been the increase in life expectancy, accompanied by a substantial improvement
in the health parameters of populations, although these achievements are
unequally distributed across countries and socioeconomic contexts. Reaching old
age, which was once the privilege of the few, has today become the norm, even
in the poorest countries. The accomplishment, however, has resulted in a major
challenge: how to add quality to the additional years of life.
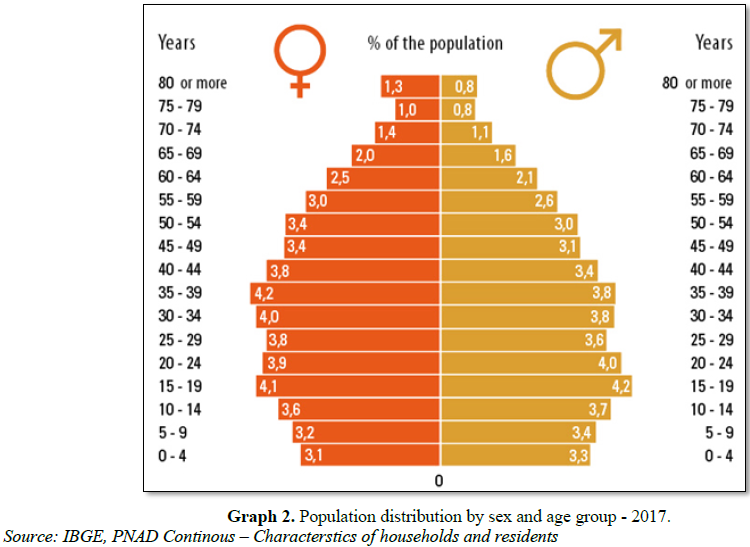
The elderly have a
number of well-established health characteristics – more chronic diseases and
frailties, greater health costs and lower social and financial resources. Even
without chronic diseases, aging involves functional loss. Due to the many adverse
situations they face, care for the elderly must be structured differently from
that of adults, in order to provide special assistance. Current health services
are based around fragmentary care, with multiple specialist consultations,
little sharing of information, and numerous drugs, tests and other procedures.
This burdens the system, with a major financial impact at all levels, and does
not generate significant benefits in quality of life [3,4].
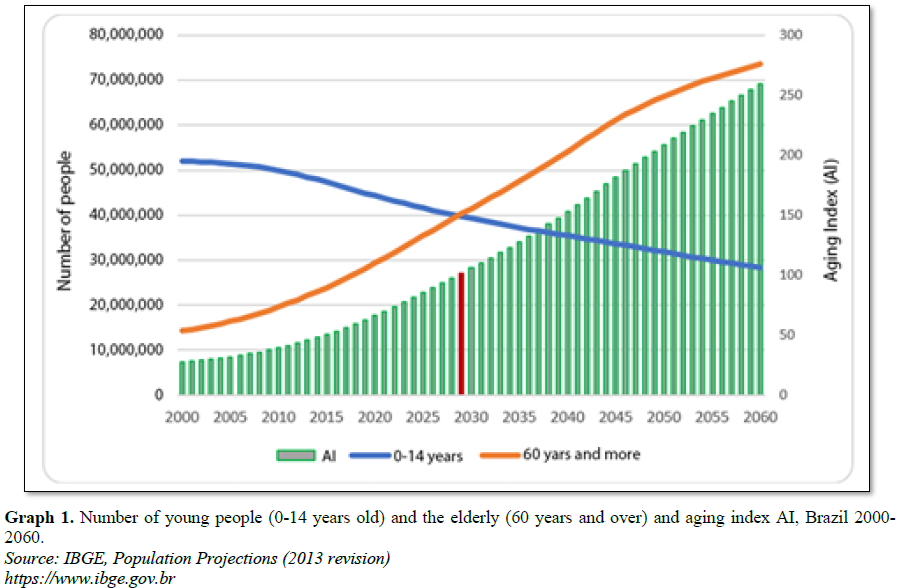
The demographic
projection for the next few years predicts further population aging. The
current scenario, therefore, is likely to worsen if the model remains
unchanged. Increased longevity leads to greater use of health services,
generating higher costs and demands on resources and threatening the
sustainability of the system. The chronic and multiple diseases that this group
suffers require constant monitoring, permanent care, continuous medication and
periodic examinations [5,6]. Our care models date from a time when Brazil was a
country of young people and acute diseases. Today, however, we are a young
country with grey hair. Actions based on health promotion and education, the
prevention and delay of the onset of diseases and frailties, and the
maintenance of independence and autonomy must be expanded [7,8].
HEALTHCARE SYSTEMS AND THE ELDERLY
In health systems
outside Brazil, general practitioners or family doctors are entirely
responsible for the treatment of 85% to 90% of their patients, without the need
for referral to specialists. Health professionals with specific training (in
Nutrition, Physical Therapy or Psychology) are also involved in care. In this
way, the elderly will have a much wider range of qualified professionals,
recommended to them by their own doctor [9].
In Brazil, however,
there is an excess of specialist consultations, with the current model
prioritizing the fragmentation of care. This can be clearly seen in comparisons
with the UK model, the National Health Service (NHS). Here, the central figure
is the general practitioner (GP), who has a high resolutive capacity and can
establish a strong bond with patients. The NHS is available to every citizen,
regardless of income or social status, in a similar manner to the SUS in
Brazil. To be eligible for free public health care, a citizen must register
with a General Practitioner (GP). The main health service units are local
clinics made up of general practitioners and nurses. Any medical care required,
provided it is not an emergency or caused by an accident, will be performed by
the health center doctor.
In contrast, the
American model is based around referral to numerous medical specialists,
resulting in a model of care that is the opposite to that of the UK. These two
rich countries, with great medical traditions, therefore employ different models
and achieve quite different results [10].
A contemporary
elderly healthcare model should employ a flow of actions based on education,
health promotion, the prevention of disease where possible, delayed onset of
illness, early care and rehabilitation from diseases. A care pathway for the
elderly based on efficacy and efficiency must presuppose an articulated,
referenced network with an information system based on this approach [11].
Health systems
currently operate with a small number of non-integrated points of care.
Patients generally enter this disjointed network at an advanced stage, with the
hospital emergency room often the entry point. Such a model, as well as being
inadequate and anachronistic, offers a very poor cost-benefit ratio, being
hospital-centered and involving intensive use of expensive technologies. Its
failure, however, should not be attributed to users, but to the care model
itself, with an overburdening at more complex levels of care due to a lack of
resolutive treatment at earlier levels.
One of the problems
faced by most current care models is an exclusive focus on disease. Even when a
program based on anticipating illness is offered, the proposals are primarily
geared towards the reduction of a certain disease. This overlooks the fact that
when a chronic disease is established the objective should not be a cure, but
stabilizing the clinical picture and constant monitoring to prevent or
ameliorate functional decline [12].
Studies have shown
that care must be organized in an integrated manner and should be coordinated
throughout its duration in a logic-based network, from entry into the system to
end of life care. New models of healthcare for the elderly should therefore
present a proposal for a care pathway that focuses on actions of education,
health promotion, the prevention of diseases where possible, delaying the onset
of disease, early care and rehabilitation.
Financial pressure
Demographic
transitions and the improvement in Brazil's social and economic indicators,
when compared with previous decades, have led not only to the growth of the
elderly population, but also to greater financial pressure on public and
private health systems. As the number of elderly people increases, so,
naturally, does the prevalence of chronic diseases and spending [8].
In recent decades
it has been seen that most of the public health problems that affect the
population – both communicable and non-communicable diseases – can be
prevented. This is demonstrated by a significant decrease in mortality from coronary
and cerebrovascular diseases and a reduction in the incidence of and mortality
from cervical cancer, as well as a decline in the prevalence of smoking and the
occurrence of lung cancer in men. A major social and economic burden can
therefore be avoided through the reduction of disease [13].
Many still see
preventative action as a burden of additional procedures and costs. In fact it
is the inverse of such thinking and, in the medium and long term, can reduce
hospitalizations and other, much more expensive procedures. All the evidence
indicates that biomedical health systems are likely to suffer problems of
sustainability in the future.
We live in the
information age. In the Collective Health field, epidemiological information
can be translated into a capacity to predict events, enabling early diagnosis,
especially in relation to chronic diseases. It can delay the onset of such
illnesses, improving quality of life and the effectiveness of the therapeutic
approach [10].
The model we
propose is based on the early identification of the risks of frailty among
users. Once risk is identified, the priority is early rehabilitation in order
to reduce the impact of chronic conditions on functionality, seeking to
intervene before harmful effects can occur. The idea is to monitor health, not
disease, with the intention of delaying the onset of illness so that the
elderly can enjoy the time they have left. Thus, the best strategy for the
proper care of the elderly is based on the permanent monitoring of health and
keeping such individuals under continuous observation, varying only the level,
intensity and context of the intervention [14].
The role of the
health professional in these cases is not to avoid the disease (as it is
already settled) or seek a cure, but to stabilize and reduce harm, aimed at
maintaining quality of life and preventing or mitigating functional decline
[15]. In general terms, these are the foundations of the healthcare proposed by
the Caring Senior program.
AN INNOVATIVE HEALTHCARE MODEL
Elderly care should
be structured in a unique manner. The current provision of health services
fragments care for this age group, with multiple specialist consultations, a
failure to share information, the widespread use of drugs, clinical and imaging
exams, and other procedures that overwhelm the system, have a major financial
impact at all levels and do not generate significant benefits for health or
quality of life [5]. As stated above, one of the problems stems from the
exclusive focus on disease.
The hierarchy of
the network provides at least two fundamental benefits for the care of the
elderly: reduced iatrogeny and more organized flow of care. Clinical guidelines
and protocols are also essential for the construction of the treatment plan.
They should direct good practices, be based on the best evidence available and
be appropriate for each clinical situation. The treatment plan guides the care
pathway according to the needs of the patient [14].
Programs aimed at
this group should be based on integrated care, with the key health professional
and his or her team managing not the disease, but the health profile of the
patient. Often, a health problem can only be treated with the reduction or
suspension of other actions [16]. Prevention is essential. The earlier an
intervention is carried out, the better the chances of a more positive
prognosis [9]. A health unit with a wider range of characteristics allows the
anticipation of problems through the early identification of possible symptoms,
changes in mood or possible functional loss. In this way, the elderly
individual can be referred promptly to their attending doctor [15].
A phrase which has
been repeated for decades in medicine is that the more a healthcare
professional knows about the history of their patient, the more positive the
results will be. This belief is supported by the World Health Organization and
all managers and professionals in the field of health. As logical as it is old,
it continues to represent a modern idea of a health care model [13]. It is
surprising, then, that we do not see it practiced on a daily basis. There
should be an emphasis on the integrated care of the elderly, adding
conventional medical care to the development of supervised educational and
leisure activities. The purpose is to maintain a good quality of life for as
long as possible.
The hospital is
often seen as the ideal location for healing. This, however, is a conceptual
error. Instead, the model should include several care settings prior to the
hospital, and hospitalization should occur only at the acute moment of chronic
illness or in cases of emergency, and should be as brief as possible. The entry
point to the system should be somewhere that allows the client and their family
to feel protected and supported. It is in this setting of first contact that
the user is informed of all the care possibilities and pathways available to
them. The reception phase is fundamental for those entering the system, and is
a stimulus for developing trust and fidelity.
The proposal of care
for the elderly should be understood as a strategy for establishing care
pathways, organizing the movement of individuals through the system according
to their degree of frailty. The identification of risk and the integrality of
care at the different points of the network are key to this model.
Hierarchization does not presuppose an evolutionary path between the care
levels of the model, although expected patterns can be anticipated. The stages
cannot be absolutely fixed, however, as there is always the possibility of
reverting disability and returning to less complex levels of care, depending on
each individual situation.
Better care results
and economic-financial outcomes are needed. To achieve this, everyone involved
in the model should understand the need for change and allow themselves to
innovate – in the care they provide, in the remuneration of the model, and in
the evaluation of the quality of the sector. Innovation often means recovering
the simplest forms of care and values that have been lost within our health
system.
The main risk
factor of most of the chronic diseases that affect the elderly individual is
age itself. Aging without chronic illnesses is the exception rather than the
rule. Thus, the focus of any contemporary policy should be to promote healthy
aging, by maintaining and improving – where possible – the functional capacity
of the elderly, the prevention of diseases, the recovery of the health of those
who have become sick (or the stabilization of illnesses) and the rehabilitation
of those who have had their functional capacity restricted. Actions such as
these, however, are still rare. The greatest investment continues to be in
traditional care, with emphasis on the hospital structure [4].
To say that
monitoring health and anticipating predictable illnesses is a "different
and innovative" way of caring questions the efficiency of healthcare
managers. Ideally, health care services should focus on providing qualified
care and well-being for the elderly, ensuring their clients have a referral
doctor, and that all doctors have a portfolio of clients for whom they provide
care. The care unit space should have the characteristics of a social center,
with a variety of activities including medical consultations and actions aimed
at integration and participation, encouraging the establishing of trust and
client loyalty within the model. This “innovation” is at least 70 years old, as
it has operated in the UK since 1948. It is nonsensical to consider it new. The
model proposed here, which we will call Caring
Senior, embraces the successful British experience and offers permanent
monitoring of health.
Our proposal: The caring senior model
To put these
theories into practice, the model of care for the elderly in Brazil must be
urgently redesigned [17]. The Caring Senior model was designed with these basic
assumptions in mind, and is characterized by a focus on low-intensity instances
of care, through the constant monitoring of the elderly and the provision of
light, but intensive care, as it is known that when properly monitored, more
than 85% of such clients do not require more complex care.
Other healthcare
actions will be the responsibility of a separate structure, which is
responsible for dealing with segments such as the emergency unit, the hospital,
clinical and imaging exams and medical specialists. Caring Senior will involve
specialist doctors and will also accompany its clients in high-intensity
instances of care – but as a support mechanism, not as a central element of
care, as we will see below.
Four aspects
underlie the entry point (or level 1) of Caring Senior: reception, fidelity,
integrality and assessment of the risk of frailty/ disability. Within this
model, levels 1 to 3 are low-intensity settings, or in other words involve
lower costs and are largely composed of care provided by well-trained health
professionals. Efforts should be made to maintain patients at such
low-intensity levels of care to preserve their quality of life and social
engagement [18]. The other settings, which involve more serious cases, are
expensive and include hospitals and other long stay facilities. Within these
settings, the preference is to rehabilitate the patient and transfer them to
low intensity settings, although this will not always be possible. Efforts
should be made to maintain the elderly within the first three levels of care,
to preserve quality of life and reduce costs. The goal is to concentrate more
than 90% of the elderly in these settings [19].
Care models for
this age group should be people-centered, based on the specific needs of
individuals. Care should be managed from the moment of entering the system to
the end of life, with constant monitoring. We know that the elderly face
specific challenges due to chronic diseases and the bodily and social frailties
they suffer [8]. Entering the model through Level 1 (reception) guarantees
conscious access to the system, a start based on transparency of the rules of
the healthcare plan, grace periods, rights and obligations, the care offered,
and bonuses and rewards. It is, therefore, the entry point, a crucial moment
for establishing empathy and trust, fundamental elements of user fidelity.
Another important
differential is the proposal to register the care pathways of patients through
a comprehensive information system, which will record not only the clinical
evolution of the elderly persons, but also their participation in individual or
collective preventative actions, as well as interaction with the care support
manager and phone calls made to or by the “GerontoLine” (the name we have given
to a qualified and resolutive call-center) or use of computer or smart phone
apps. This allows the sharing of information, enabling a more complete
evaluation of the individual and including the medical records of the hospital
unit, governed by specific norms.
Caring Senior is
based on certain principles. The first is the role of the doctor, who is
responsible for a portfolio of clients. A nurse will also be available, and
will perform an effective role in providing care to the clientele and ensuring
better quality of care. The clinical unit will have several such pairs of
general practitioners and nurses, and a 40-hour work week will allow for
portfolios that can provide care to between 800 and 1,000 clients. This will
guarantee that healthcare professionals have the time to attend each client
properly, ensuring appointments at least four times a year, and accompanying
them in other instances of care, if necessary.
A full Caring
Senior unit, for example, will have five pairs of doctors and nurses who are
responsible for around 4,000 to 5,000 patients. Health professionals must be
trained to provide care within the philosophy of the program, prioritizing
health promotion and disease prevention. These will include psychologists,
nutritionists, physiotherapists and physical educators, who will attend cases
as selected by doctors. These professionals will lead group activities and
lectures and provide guidance on relevant topics. In addition, each region
(depending of course on demand) will have two or three minimum capacity units,
featuring only a doctor/nurse pair, with support services provided in the full
unit.
To allay fears
about the possible high costs of maintaining such a structure, it is worth
noting that health professionals cost much less than a day's stay in an
Intensive Care Unit or hospital. To provide good care and avoid the exaggerated
use of specialist doctors and unnecessary hospitalizations, it is essential to
maintain a high quality reception structure.
This relationship
between the healthcare system and the user must change. It should be
transparent, establishing a pact based on truth. The actions performed must be
recorded in the information system, which must begin at reception and continue
until the end of the patient's life [20].
The hierarchy of
the care model provides knowledge of its users, their profile and their needs,
in order to better organize the delivery of services. One thing is certain:
without better organization of the care of the elderly and the elaboration of a
care plan, population aging and the greater prevalence of diseases will cease
to be opportunities, and will instead become obstacles for the sustainability
of the Brazilian supplementary health system.
It is important to
emphasize that the proposal presented herein is not only intended to discuss
mechanisms for the reduction of health costs, which, while important, is not
the only concern. Like the other issues, it drives us towards a greater goal,
namely the integral care of the elderly. The model presented has a commitment
and goal of improving the quality and coordination of the care provided from
the entry point to the system and throughout the continuum of care, avoiding
redundant examinations and prescriptions, interruptions in the health
trajectory of the user and iatrogeny generated by the disarticulation of health
interventions.
The hospital and
the emergency room will always be important settings for the provision of
health care, but it is necessary to redefine and recreate the roles they play
in today’s health care network. These units of care should be reserved
primarily for moments of acute chronic illness [21].
An adult client
aged over 49, with one or more chronic diseases will not be cured. The duty of
the physician is to stabilize, monitor, and ease the pain caused by the
disease, which is likely to remain with the patient for the rest of their
lives. The role of the Caring Senior general practitioner will be to maintain
the functional capacity of clients so that they can enjoy a full and healthy
life. The benefit of Caring Senior will be the reduction of the numbers of
specialist doctors and subsequently fewer exams and drugs, as loyalty will
prevent the client from resorting to emergency units and so greatly reduce
hospitalization periods.
It should be
remembered that Caring Senior involves low-intensity instances of care, and is
largely composed of care provided by well-trained health professionals
concerned with preserving the quality of life and social participation of their
elderly clients. Instances considered high-intensity are expensive and involve
the hospital and other long stay units. All effort must be taken to
rehabilitate the elderly and return them to low-intensity instances of care.
Central points of the model
Three aspects must
be considered, namely:
1.
The doctor and
nurse are responsible for a portfolio of clients.
2.
The user will
receive a financial stimulus (reward) for adherence to the care model, which is
based on monitoring and fidelity to the health team.
3.
The
remuneration of the physician and the health team will be established through
the success of the care. Better performance results in better rewards. It is
acknowledged that health professionals are poorly paid.
The quality of care
offered by the attending physician, his or her client portfolio and his or her
variable remuneration are of similar importance. Emphasis is also placed on the
client portfolio, functional assessments, the tracking of risks, the work of
the care support manager, and an efficient information system that records all
client events. The importance of the various care settings, such as the
outpatient clinic, the hospital, home care, rehabilitation, the
multidisciplinary team, the cohabitation center and palliative care, should
also be highlighted. All are part of the network of care and are integrated
through the information system and the attending physician, who remains the
clinical reference throughout the course of the model. It is clear that the
hospital is only one setting. It is equal to the others, but less important
than preventive actions, which are the center of the model. The logic is based
on low-intensity settings and integral care, the multidisciplinary team and the
doctor responsible for the patient.
For the model to
succeed, therefore, it is essential that clients are encouraged to participate
in the proposed programs and actions, instead of the current logic of using a
health plan only when undergoing tests or going to hospital with a disease
already in an advanced stage. The model includes all possible care settings,
excludes nothing in relation to the care required – in fact, it includes new
units not usually offered to the clients of many healthcare providers – and
prioritizes the provision of care in “lower intensity" settings. These
offer the best possible care, with trained and qualified professionals, based
on modern scientific conceptions of treatment. In short, our proposal is to
invest in health to reduce spending on disease.
A high quality,
easy to use technology information system will provide fundamental support for
the doctor/nurse pairing and facilitate client loyalty. Technology is an
essential part of the Caring Senior project, and so participants must be able
to use the system to its maximum potential.
For example, the
faces of clients could be recognized when they come through the door of the
clinic, allowing their medical records to be open on the receptionist’s desk by
the time they get there. The receptionists can then address the clients by
name, ask about their families, and check the list of medications they are
taking. These simple actions add enormous trust to the relationship, making the
client feel protected and welcomed from the first instance.
Registering the
care pathways of the patient is a unique feature of this model. A high-quality
information system of broad scope can document not only the clinical evolution
of the elderly person, but also their participation in individual or collective
prevention actions, as well as the support provided by the nurse and telephone
calls made, all of which must be resolutive and performed by trained and qualified
personnel.
Information from
telephone, computer or cell phone contact between patients and professionals
should be shared among the team, to enable a comprehensive assessment of the
individual. The information system, which begins with the registration of the
client, is one of the pillars of the program. It allows the entire care pathway
to be monitored at each level, verifying the effectiveness of the actions and
contributing to decision-making and follow-up care. It is a unique electronic
record, which is both longitudinal and involves a range of professionals, and
accompanies clients from reception onwards. This medical record differs from
existing registries as it includes a record of their life history and health
events.
The creation of a
mobile app with individualized information and reminders of consultations and
prescribed actions is also planned. This can, among other actions, ask the
client to take a photo of their breakfast and send it to the nutritionist, who
will observe if the meal is balanced and if there are adequate amounts of
fiber, for example.
Caring Senior will
focus on keeping its clients within its units, avoiding the use of specialists.
However, five areas of medical specialties related to our model will be
required to assist the general practitioner – cardiology, gynecology,
urology-proctology, dermatology and ophthalmology. These are chosen based on
demand and high prevalence, and include areas where annual preventive control
examinations can be carried out and registered.
Consultation with
the specialties listed will only be possible at the request of the general
practitioner of the client. If they require the care of one specialist, Caring
Senior will not necessarily include the other specialties. The same reasoning
applies to hospitalization. Doctors and nurses will be responsible for
contacting the hospital doctor, armed with knowledge of the case and,
preferably acting to ensure the best care and the briefest period of
hospitalization, as well as being able, if necessary, to suggest a medical
specialist.
Another key element
of Caring Senior is the form of payment of physicians, the Accountable Care
Organization (ACO) system, which encourages healthcare professionals to
organize themselves as a group, managing the quality of services provided,
being responsible for cost management and the distribution of bonuses [22].
There are two key
points: the provision of services of excellence at a lower cost and a model of
remuneration based on added value. The segmented and non-integrated healthcare
that is offered to patients today is largely due to the service remuneration
model, in which the incentive is production, rather than quality [23]. In other
words, there is no benefit in seeking new forms of care or new payment models
if transferring part of the responsibilities, risks and benefits of providers
is not associated with the results achieved through the care provided. The
challenge is to make this new care model acceptable to the client, since trust
(which will lead to loyalty) is an indispensable factor if the process is to
function as planned. One cannot, after all, ask a person to trust something
they do not understand.
Simply stating that
Caring Senior is the best model is irrelevant, however, if it is not applied by
Brazilian supplementary health services. Society needs to be made fully aware
of the proposal if it is to become convinced of its benefits [6]. Otherwise,
healthcare will continue to opt for the “siren song” of excess and consumption,
which burden the system, generate higher costs, and render long-term care
unfeasible.
FINAL REMARKS
The desire for a
higher quality and more effective elderly care model is not solely a Brazilian
concern. The entire world is debating this issue, recognizing the need for
change and proposing improvements in their health systems [33].
There is no single
model, but instead a multi-faceted approach that favors low-intensity care,
constant monitoring, an efficient telephone service and the use of mobile apps,
a doctor responsible for a portfolio of clients who then accompanies them
through all the care settings, a nurse who works in partnership with the
doctor, teamwork, the use of epidemiological tools to monitor functionality,
and a quality electronic medical record. All these elements contrast with the
model based around specialist doctors, the disarticulation of professionals,
the prioritization of use of the hospital, the excessive consumption of drugs
and an overuse of laboratory and image exams [25].
There are a number
of suggestions for care pathway models. The important thing is for each health
institution to be aware of its users, their profile and their needs, to
construct the best way of organizing the delivery of its service. One thing is
certain – without the organization of elderly care and the elaboration of a
care plan, population aging and the increased prevalence of chronic diseases in
the public or supplementary health sector in Brazil may no longer be seen as
opportunities, but instead become obstacles to the sustainability of the
system.
The socioeconomic
transformations of recent decades and the consequent alterations in the
lifestyles of individuals in contemporary societies – with changes in eating
habits, increased sedentarism and stress, plus the greater life expectancy of
the population – have contributed to a higher incidence of chronic diseases,
something that today represents a serious public health problem.
The current
provision of health services fragments care for the elderly. It overburdens the
system, causes a serious financial impact at all levels and does not generate
significant benefits for quality of life. It is therefore imperative that a new
model is adopted. If we know the population is older, that diseases are chronic
and multiple, that the costs of care are increasing, that the models of care
are from an era of acute diseases and that a knowledge of epidemiology can
inform us of risk factors, why do we continue to offer an outdated and
ineffective product? Especially if we have all the information required to
implement an assistance-based care model in which everyone benefits?
It is necessary to
rethink and redesign care for the elderly, turning the focus towards the
individual and their particularities. This will bring benefits not only to this
part of the population, but also quality and sustainability to the entire
Brazilian health system.
We believe that it
is possible to grow old with health and a good quality of life, provided that
all the actors in the sector see themselves as responsible for the necessary
changes and allow themselves to innovate through improvements in care, in forms
of remuneration and in evaluating the quality of the sector [26].
Elderly persons,
because of their greater vulnerability and greater use of the health system,
are among the most affected by the current care model.
As Don Berwick [27]
wrote in the Institute for Healthcare Improvement (IHI) – “Every health system
is perfectly designed to achieve the results it achieves”. Our health system
has achieved a demographic transition (aging), an epidemiological transition
(we now have a triple burden of diseases), a nutritional transition (we have
moved from malnutrition to obesity), but we have not been able to make the
much-needed transition in our health institutions, which remain organized to
treat acute, infectious diseases [28]. Some elements are necessary if a system
is to change health outcomes, such as evaluation and remuneration based on
quality and an information system that can facilitate the care pathway of the
patient.
It is possible to
reorient the healthcare of the elderly population and to construct an
organization within this sector that provides greater well-being and better
economic-financial results. To achieve this, everyone involved must realize
they are responsible for the changes required and allow themselves to innovate
– which, in many situations, means recovering the simpler care and values that
have been lost within our health system.
The entire model
proposes a reorganization of care that has already been shown to be much more
effective and cheaper for the health system. It simply means doing what is
necessary, in the right way, focusing on the most important element of every
process, which is the patient.
Another key point
is the participation of the elderly person in the model, using strategies that
can help to convince these individuals of the importance of preventive care,
such as the rewards offered by health plans.
1. Abicalaffe CL (2011) Pagamento por
performance: O desafio de avaliar o desempenho na área da saúde. J Bras Econ
Saúde 3: 179-185.
2. Banco M (2011) Envelhecendo Em Um
Brasil Mais Velho. Washington Dc: World Bank
3. Berwick DM (2011) Launching
accountable care organizations: The proposed rule for the medicare shared
savings program. N Engl J Med 364: 32.
4. Berwick DM (2011) Making good on
Acos’ promise: The final rule for the medicare shared savings program. N Engl J
Med 365: 1753-1756.
5. Box G (2016) Understanding and
responding to demand in English general practice. Br J Gen Pract 66: 456-457.
6. Brasil (2013) Agência Nacional De
Saúde Suplementar. Plano De Cuidado Para Idosos Na Saúde Suplementar. Rio De
Janeiro: Ans.
7. Brasil (2006) Ministério Da Saúde.
Portaria Nº. 2.528, 19 De Outubro De 2006. Aprova A Política Nacional De Saúde
Da Pessoa Idosa. Brasília, Df: Ministério Da Saúde.
8. Caldas CP, Veras RP, da Motta LB
(2015) Atendimento De Emergência E Suas Interfaces: O Cuidado De Curta Duração
A Idosos. J Bras Econ Saúde 7: 62-69.
9. Carvalho VKS, Marques CP, Silva EN
(2016) Contribuição Do Programa Mais Médicos: Análise A Partir Das
Recomendações Da Oms Para Provimento De Médicos. Ciênc Saúde Colet 21:
2773-2784.
10. Closs E, Schwnake Cha. A (2012)
Evolução Do Índice De Envelhecimento No Brasil, Nas Suas Regiões E Unidades
Federativas No Período De 1970 A 2010. Rev Bras Geriatr Gerontol 15: 443-458.
11. de Lima KC, Caldas CP, Veras RP
(2016) Health promotion and education: A study of the effectiveness of programs
focusing on the aging process. Int J Health Serv.
12. Instituto Brasileiro De Geografia
E Estatística (Ibge). Population Projections. Rio De Janeiro: Ibge, 2013.
Available at: https://www.ibge.gov.br/apps/populacao/projecao/ Access: 12 May 2019.
13. Instituto Brasileiro De Geografia
E Estatística (Ibge). Indicadores Sociais. Rio De Janeiro: Ibge, 2018.
Available at: https://www.ibge.gov.br/estatisticas/sociais/trabalho/17270-pnad-continua.html?t=series-hist%25c3%25b3ricas Access: 12 May 2019.
14. Lima-Costa MF, Veras RP (2003)
Saúde Pública E Envelhecimento [Editorial]. Cad Saúde Pública 19: 700-701.
15. Médici A, Abicalaffe C, Tavares L
(2018) Pagamento Por Performance. Empreender Saúde; 2015. Disponível Em: https://www.researchgate.net/publication/281642162_pagamento_por_performance_em_saude#pf3 Access: May 17.
16. Mendes EV (2011) As Redes De
Atenção À Saúde. Brasília, Df: Opas.
17. Minayo MCS, Firmo JOA (2019)
Longevidade: Bônus Ou Ônus? Editorial. Ciênc. Saúde Colet 24. Available at: https://doi.org/10.1590/1413-81232018241.31212018
18. Moraes EN (2012) Atenção À Saúde
Do Idoso: Aspectos Conceituais. Brasília: Organização. Pan-Americana Da
Saúde.
19. Oliveira M, Veras RP, Cordeiro HA
(2017) Saúde Suplementar E O Envelhecimento Após 19 Anos De Regulação: Onde
Estamos? Rev Bras Geriatr Gerontol 20: 624-633.
20. Oliveira M, Veras RP (2015) Um
Modelo Eficiente No Cuidado À Pessoa Idosa. Correio Brasiliense 27: 13.
21. Oliveira MR, Silveira DP, Neves R
(2016) Idoso Na Saúde Suplementar: Uma Urgência Para A Saúde Da Sociedade E
Para A Sustentabilidade Do Setor. Rio De Janeiro: Ans.
22. Oliveira MR, Veras RP, Cordeiro HA
(2016) A Mudança De Modelo Assistencial De Cuidado Ao Idoso Na Saúde
Suplementar: Identificação De Seus Pontos-Chave E Obstáculos Para
Implementação. Physis: Revista De Saúde Coletiva 26: 1383-1394.
23. Silva AMM, Mambrini JVM, Peixoto
SV (2017) Uso De Serviços De Saúde Por Idosos Brasileiros Com E Sem Limitação
Funcional. Rev Saúde Pública 51: 1-10.
24. Szwarcwald CL, Damacena GN, Souza
Júnior PRB (2016) Percepção Da População Brasileira Sobre A Assistência
Prestada Pelo Médico. Cienc Saúde Colet 21: 339-350.
25. Veras RP, Amorim AE (2015)
Relatório Final Unati/ Uerj: Projeto: Modelo De Hierarquização Da Atenção Ao
Idoso Com Base Na Complexidade Dos Cuidados: Proposta De Monitoramento Dos Três
Níveis De Cuidado Na Assistência Suplementar. Rio De Janeiro Contrato
Br/Cnt/1401445.001.
26. Veras RP, Caldas CP, Cordeiro HA
(2013) Desenvolvimento De Uma Linha De Cuidados Para O Idoso: Hierarquização Da
Atenção Baseada Na Capacidade Funcional. Rev Bras Geriatr Gerontol 16: 385-392.
27. Veras RP, Caldas CP, Cordeiro HA
(2013) Modelos De Atenção À Saúde Do Idoso: Repensando O Sentido Da Prevenção
Physis: Revista De Saúde Coletiva 23: 1189-1213.
28. Veras RP, Caldas CP, Motta LB
(2014) Integração E Continuidade Do Cuidado Em Modelos De Rede De Atenção À Saúde
Para Idosos Frágeis. Rev Saúde Pública 48: 357-365.
29. Veras RP, Estevam A (2015)Modelo
De Atenção À Saúde Do Idoso: Ênfase Sobre O Primeiro Nível De Atenção. In:
Lozer AC, Godoy CVC, Leles FAG, (Eds.). Conhecimento Técnico-Científico Para
Qualificação Da Saúde Suplementar. Brasília, Df: Opas/Ans, pp: 73-84.
30. Veras RP, Lima-Costa MF (2011)
Epidemiologia Do Envelhecimento. In: De Almeida Filho N, Barreto Ml.
Epidemiologia E Saúde: Fundamentos, Métodos, Aplicações. Rio De Janeiro:
Guanabara Koogan, pp: 427-437.
31. Veras RP, Oliveira M (2018)
Envelhecer No Brasil: A Construção De Um Modelo De Cuidado. Ciênc Saúde Colet
23: 1929-1936.
32. Veras RP, Oliveira MR (2016) Linha
De Cuidado Para O Idoso: Detalhando O Modelo. Rev Bras Geriatr Gerontol 19:
887-905.
33. Veras RP (2011) A Necessária
Gestão Qualificada Na Área Da Saúde: Decorrência Da Ampliação Do Segmento
Etário Dos Idosos. J Bras Econ Saúde 3: 31-39.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Advance Research on Alzheimers and Parkinsons Disease
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)