2969
Views & Citations1969
Likes & Shares
Objective: To assess the existing evidence
regarding opioid use among rural dwellers.
Methods: A
detailed electronic search strategy was developed using the following
databases: CINAHL Complete, Health Source, Nursing/Academic Edition, MEDLINE
with Full Text, Psych ARTICLES, Psychology and Behavioral Sciences Collection,
Psych INFO and Social Sciences Full Text. Each study included rural subjects or
areas. Data were
extracted from 22 articles found through a systematic search encompassing 2013
– early 2018.
Results: In most of the studies (64%), the
reported findings included both rural and urban settings. Definition of the
term rural varied considerably among the different articles based on the
criteria. There is an overall increase in opioid use across the nation, but a
new research focus is the prominence of opioid use in rural communities.
Conclusion: This systematic search indicates a
need for further research in the prevention and treatment of opioid misuse and
addiction. Most of the reviewed
articles were descriptive in nature, limiting the evidence regarding the
interventions used to address the opioid crisis. There was no evidence
regarding the prescribing factors pertaining to nurse practitioners, certified
midwives and physician assistants that affect the accessibility to treatment
options in rural areas. The policy implications are to support the qualified
health care providers in rural areas to obtain waivers to provide Medication
Assisted Treatment (MAT) for opioid use disorder. Moreover, it is imperative to
develop and implement policies to address the barriers to opioid addiction
treatment services provision and access in rural areas.
Keywords: Opioid use, Disuse, Misuse, Medication assisted treatment, Rural
INTRODUCTION
Effectively managing pain in patients has become an integral part of
healthcare today; it is also cause for concern with regard to the misuse of
prescribed medications and opioid abuse. Although the number of opiate prescriptions
decreased from 282 million to 236 million, national data illustrates 11.5
million persons aged 12 and over misused prescription pain relievers in 2016
[1,2]. These startling statistics have caused a prioritization shift among
national organizations and many healthcare providers when it comes to assessing
community needs. In a position statement by the American Nurses Association
addressing pain management and the opioid epidemic, nurses have an ethical
responsibility to relieve pain and the suffering it causes as well as serve as societal leaders in the development of
multimodal/interdisciplinary approaches to safely manage this crippling disease
[3]. Several factors, including a shortage of primary care providers and pain
specialists in rural areas, coalesce in rural communities to form an
environment that is conductive to an opioid crisis. Innovative, creative
collaboration between communities, national leaders and healthcare providers is
needed to provide an antidote for the many rural dwellers experiencing
adversity in opioid medication use.
Opioid
use in rural areas has unfolded into a story that highlights an increase in the
availability of prescription opioid medications as well as a brewing epidemic.
In some instances, opioid use presents as a greater challenge in rural than
urban communities. Although rural dwellers possess many positive traits such as
resilience, these areas are often inhabited with a smaller population and
equipped with limited health and social resources compared to urban communities.
Coupled with individual socioeconomic vulnerabilities (limited
education, poor health status, low income), the perfect storm is created and serves as a catalyst for an opioid
crisis [4]. While national data shows an overall increase in opioid use,
rural areas are noted to have higher prevalence of opioid and naloxone use as
well as opioid related deaths [5]. Until recently, existing bodies of
literature have largely focused on opioid use in urban areas and have often
used rural areas for comparative purposes. The aim of this review is to assess
the current evidence concerning opioid use among rural dwellers.
METHODOLOGY
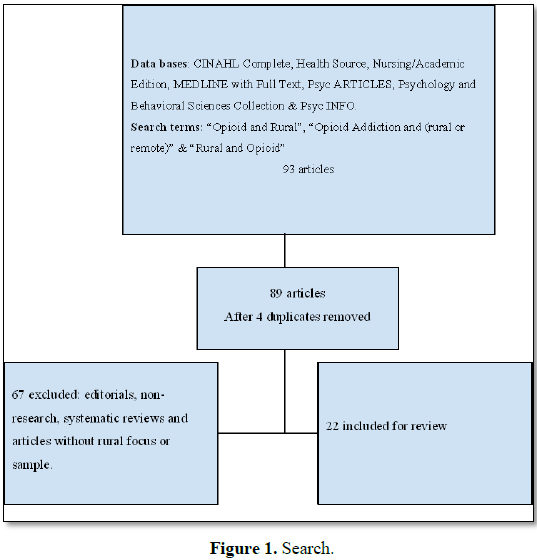
This systematic review is reported using the
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA)
standards [6]. This method of reporting consists of an internationally
recognized 27-item checklist developed to ensure quality in systematic
reviewing. To identify literature for review, a detailed online search strategy
was developed using the following databases: CINAHL Complete, Health Source,
Nursing/Academic Edition, MEDLINE with Full Text, Psych ARTICLES, Psychology
and Behavioral Sciences Collection, Psych INFO and Social Sciences Full Text.
These databases were searched with the intention of reviewing literature
pertaining to opioid drugs and rural areas. Search terms “opioid AND rural” as
well as “opioid addiction AND (rural or remote)” did not provide adequate
search results. A different strategy including the terms: “rural n5 opioid”
(rural within 5 words of opioid) was applied. This new strategy presented
adequate results and was thus utilized in this review. The search was limited
to English language and peer reviewed domestic or international articles
published between the years of 2013-2018. This search produced 93 possible
results. Four articles were duplicates and removed leaving 89 for further
consideration.
A careful
review of the abstract and methodology of each article resulted in deletion of
67 articles that were editorials, non-research, systematic reviews or did not
pertain to rural populations. 22 articles were appropriate for final review (Figure 1).
RESULTS
The literature in this systematic review was
primarily descriptive or epidemiological in design (Table 1) [7-28] Table 2
provides information on sampling methodology and sample size on all of the
studies. Sample sizes range from 28-75,964 with the studies with high sample
sizes coming from secondary analysis of national data sets [9,28]. Slightly
less than half (10) used secondary data to conduct research [10,12-14,18-20,26-28].
Several articles used federal data set to identify physician waivers for
prescribing opioid treatments [13,14,20]. Three studies used the National
Survey of Drug Use and Health (NSDUH) [19,27,28]. Finally, authors of two
papers used the same data source (NSDUH) for the same time period (2011-2012)
to release two different studies with different populations [19,27].
Rural
Although rural was used in the search terms, 64% of the articles sampled rural and urban
populations. The remaining 36% of the articles discussed rural only (Table 3). Another factor that varied greatly between
studies was the definition of the term rural (Table 4). Some articles defined rural based on codes such as zip
codes, Rural-Urban Continuum Codes (RUCC) or Urban Influence Codes (UIC). Other
articles used abstract quantifiers such as perceived social and health status
of underserved areas and simply the name of a region, such as Appalachia.
Additionally, several articles identified rural areas as those considered
underserved in access to health and social services or provided no definition
of rural.
Place
Two studies were conducted outside of the
United States, in Australia; New South Wales and Vietnam [7,9]. All remaining
articles were conducted in the United States. A few locations are mentioned
more than others. For example, two groups conducted their studies in Cortland
County, NY [20,23]. Three groups of authors conducted their studies in Kentucky
[10,21,22]. Both upstate NY and the eastern region of KY are part of the
Appalachia Mountain Range and presented as rural in the research.
Similarities and differences in findings
Findings indicate that there is little
research regarding interventions for opioid drug abuse in either rural or
non-rural locations. The intervention that received the most attention in the
review of literature was the number and distribution of Medication Assisted
Treatment (MAT) for opioid use and misuse The major intervention reported in
the literature was regarding efforts to increase the number of providers who
can prescribe MAT for opioid use disorder in both rural and more metropolitan
areas [8,13,14,20].
The Comprehensive Addiction and Recovery Act
(CARA) originally authorized physicians to prescribe buprenorphine in the
treatment of opioid use disorders and have been expended to include prescribers
such as nurse practitioners, and physician assistants. This law was enacted in
2016 for the purpose of opioid abuse prevention and treatment. Following the
enactment of CARA, there were moderate increases in the number of providers
with waivers. At the conclusion of 2017, 33,876 physicians, 3,534 Nurse
practitioners and 912 Physician assistants had received waivers to prescribe
Buprenorphine [29]. More research is warranted in this area so interventions
can be developed and implemented to increase the knowledge of prescribers and
to make the use of MAT readily available. There was a dearth of literature
focused on prevention of opioid abuse.
Another area deserving further research is
the use of Fentanyl on the streets. Fentanyl is an opioid used to treat pain
and can be used as an anesthetic drug when combined with other substances. In
the literature reviewed for this paper, there was no mention of Fentanyl.
However, prior to completion of this manuscript, a National Public Radio story
was released that focused on the use of Fentanyl on the streets and the high
overdose rates associated with its use [30]. The media indicates that Fentanyl
is being used illegally on the streets along with other opioids such as Heroin.
Antidotal evidence indicates overdose deaths are higher with the use of
Fentanyl, which is often combined with Heroin as an additive. This is referred to
as the third wave in the opioid crisis stating that prescription drug misuse
was the first wave, heroin the second and Fentanyl is the third. The story did
not indicate if there is a rural/urban difference in Fentanyl misuse. The
incidence of misuse of Fentanyl is occurring most frequently in the eastern
part of the United States [30]. The above news release can be traced back to a
National Vital Statistics report from the U. S. Department of Health and Human
Services, Centers for Disease Control and Prevention, National Center for
Health Statistics report in 2019 [31]. This warrants further study and research
into the effects of this specific drug in relation to the opioid crisis.
Opioid use is increasing as supported by more
than one article. For example researchers illustrated that opioid
poisoning almost doubled between 2001-2011 in the state of California [12]. An
international report examined four rural sites in an area of Australia
and found an increase in individuals on opioid maintenance treatment over a
period of four years [9]. The increase was more than 30% for three of the sites
over the four years and this study referred to opioid misuse as a global
crisis. No single study refuted the existence of an opioid crisis.
The questions of whether opioid use has
increased more in rural than urban environments is still under debate. Research
results indicated that Neonatal Abstinence Syndrome (NAS) increased
2-2.5 times per 10,000 births in rural and Appalachian counties compared to
urban and non-Appalachian Kentucky counties between 2008-2014 [10]. In 2013,
Kentucky NAS was more than double the national rate. Moreover, opioid
facilities were further from rural and Appalachian areas compared to
micropolitan/metropolitan and non-Appalachian areas (p<0.001) [10]. Similarly,
the conclusion of one national study was that rural adolescents had 35% greater
odds than their urban counterparts in Prescription Opioid Misuse (POM) [27]. The
opioid misuse was reported as 6.8% rural, 6% small urban and 5.3% for urban adolescents.
Although there is a clear trend of less POM in areas of increasing population;
reporting the level of residency in three levels may have slightly inflated the
odds of rural misuse over the more traditional two level comparisons. A spread
in prescription opioid poisoning hospital discharges, from rural and
suburban/exurban to urban areas, was found in a California state wide study [12]. One study
utilized primary care patient record forms to examine the difference
between rural residency and non-rural residency in obtaining opioid
prescription for Non-Malignant Chronic Pain (NMCP) and found that “rural
residents had higher odds of having an opioid prescription than similar
non-rural adults. Rural residency was the strongest predictor for having an
opioid prescription and a diagnosis for NMCP” (p.5) [18].
Although there were some studies that
reported an increase of opioid use in rural areas over urban, there were a few
studies that did not support this hypothesis [11,19,28]. One national study reported
that prescription opioid misuse was more common in urban than rural areas;
while another found no difference between the two [19,28]. Rigg and Monnat [19]
speculated that previous studies finding more opioid misuse in rural areas may
have had too small or a specific geographical limit in sample.
In addition to demographics, several surveys
used self-report, paper and pencil instruments to measure attributes for a wide
array of variables, such as alcohol disorders, chronic diseases, depression,
drug abuse status, health status, mental status, opioid misuse, pain, quality
of life, psychological distress, post-traumatic stress disorder and sleep
disorders.
Two articles used pain scales [7,25]. One study utilized
a visual analogue scale for pain assessment, with respiratory rate and blood
pressure to conclude that ketamine is equitable to morphine in its analgesic
effect in emergency situations where evacuation is particularly difficult [7].
One study had three pain measures, appropriate to their population of rural
patients with chronic pain [25]. The first measure was a structured pain
interview. The Wisconsin Brief Pain Inventory, measure of pain intensity and
interference and the pain catastrophizing scale both were reported as having
good psychometrics [25]. Most authors used more than one instrument for data
collection.
Social determinants of health
Increase in opioid use was sometimes
associated with other health disorders and socio-economic factors. Patients
receiving opioid medications in rural settings have poorer overall health,
higher pain levels, lower levels of education and higher rates of unemployment
than their urban counterparts [11,15]. Similarly, another study showed
that rural individuals who reported good health were less likely to use opioid
prescriptions for non-medical reasons than those who reported poor health [28].
Studies showed that lower income and manual labor were associated with an
increase in prescription opioid poisoning or prescription opioid misuse [12,19].
In addition to the general health
deteriorations that are associated with opioid use or misuse, one study found
an association between the hospital discharge diagnostic code, prescription
opioid misuse and major psychological distress [20]. Another showed an association between Anti-Social Personality
Disorder (ASPD) and hydrocodone, crack or powder cocaine, marijuana, alcohol
and heroin use [21]. One study reported significant association between
HCV (Hepatitis C Virus) and a network of non-medical prescription opioid users [23].
Similarly, another found a strong association between prescription opioid
analgesics and positive HCV [24]. In addition, arthritis was associated with
opioid use in two different studies [12,15].
The issue of ethnicity/race and opioid use is
conflicting and may be shaped by media that emphasis the newness of rural opioid reports [16,18,19,28]. In
exploring opioid prescription risk factors in a sample with Non-Malignant
Chronic Pain (NMCP), race was reported as a factor; “being non-Caucasian
was a strong predictor of having an opioid prescription and a diagnosis for
NMCP” (p 5) [18]. In a study that was not limited to chronic pain patients, black
and non-Hispanic residents were less likely than white urban residents to use
prescription opioids for non-medical reasons [28]. Yet another concluded that
white urban residents were significantly more likely to misuse prescription
opioids [19]. A content analysis of a random selection of 100 popular media
articles on the opioid crises reported “…a consistent contrast between
criminalized urban black and Latino heroin injectors with sympathetic
portrayals of suburban white prescription opioid users (p. 664) [16]. Media
reporting of drug use in urbanized areas was found to be reported in stories
that emphasized violence and arrests [16]. In contrast stories regarding rural
drug use emphasized the unexpectedness of the problem and highlighted personal
stories that humanized the individual [16].
In addition to race, social network was one
of the considered variables in rural opioid use. One study reported that
rural residents who have used drugs associated with network characteristics,
such as having trust above the average in one’s network, had lower odds of
being diagnosed with ASPD [21]. Those non-medical prescription opioid users with HCV
tended to cluster together, which suggests the need for the development of a
network-based intervention to prevent the spread of HCV [23]. Still
another suggested the utilization of school nurses, technology and
social media in opioid management [17].
Opioid use was associated with individuals
with low income and manual labor jobs in a at least two studies [12,20]. Results of
one study showed that lower income and manual labor were associated with
an increase in the hospital discharge diagnosis of prescription opioid
poisoning [12]. Another, also found those working in manual labor had
higher rates of prescription opioid misuse [20].
An intersection between other demographic
variables and the opioid use or misuse emerged in this review of the literature. A study by
Rigg and Monnat [19] found misuse of prescription opioids were
associated with other factors such as age (young), marital status (unmarried),
difficult financial status and less religiosity. Unsurprisingly, these findings
were similar to the findings in another national analysis of the NSDUH data set
[28]. These findings indicate opioid use and misuse are influenced by different
demographic variables and no one set of variables can explain an opioid
problem.
Physician waivers for buprenorphine
prescriptions were discussed in several articles [8,13,14,20,24]. A possible
rationale for the lack of research in the published literature on waiver
practices beyond that of physicians is the newness of the extension of CARA [29].
Two studies
that went beyond the numbers of physicians with prescription waivers, found
that there were barriers for obtaining the waiver of buprenorphine maintenance
treatment [8,24]. These barriers included time, finances, clients’ needs and
worries about violating patient confidentiality. After examining the Drug
Enforcement Administration (DEA) list questionnaire, a different study found
that family physicians were five times more likely to prescribe buprenorphine
than other physicians, a statistically significant finding [24]. Only 28% of
trained physicians reported prescribing buprenorphine. Abstaining from
prescribing buprenorphine was associated with lack of institutional support
[24].
A study in Washington state including
American Indian and non-American Indian, rural and urban sites offering Opioid
Assisted Treatment (OAT) found that “the number of clinics offering OAT in
rural versus urban regions was significantly lower, indicating that
difficulties may remain for rural residents in terms of accessing most OAT
services offered in these facilities” (p. 105) [14]. One study found that the
number of physicians with waivers increased in shortage counties between
2002-2011; however, opioid treatment program access remained the lowest in
counties with populations less than 2,500 individuals [13].
Around 90% of physicians with waivers are located in urban areas and only
about 1.3% practiced in the most rural areas [20]. These authors concluded
rural residency was associated with lack of access to buprenorphine
prescriptions [20].
LITERATURE
LIMITATIONS
Authors routinely discussed possible
limitations of their research. One limitation pertinent to research on
sensitive topics included recognition that participants may be reluctant to
disclose opioid use or misuse due to stigma and possible legal ramifications.
Lack of anonymity is often considered inherent in rural research (particularly
with small sample sizes) and clinical practice in rural areas. Although
appropriate to the design, at least one article reported data collected from
twenty years ago [15].
CONCLUSION
Although there is no doubt about the spread of
negative effects and side-effects of opioid use and misuse, past perceptions of
drug use as primarily an urban problem, were not supported in this review. The
research was inconclusive on the question of where opioid abuse is worse, in
rural or urban environments. How rural was operationalized differed from one
study to another, adding to the lack of clarity regarding exactly how severe an
opioid problem exists in rural areas. In addition to the geographical factors
that may be associated with opioid use and misuse; physical, psychological,
social, financial, occupational and religious factors were reported.
Although buprenorphine prescribing was
studied in a sub-set of the articles, more interventional studies about opioid
management are needed. More than half of the reviewed articles were descriptive
and based on secondary data analysis. Interventional studies for opioid misuse
prevention and management is suggested. These types of interventional studies
are needed to provide evidence on how to best decrease the opioid crisis. The
literature reviewed failed to produce data on implementation of solutions,
beyond measuring the number of and location of physicians with MAT prescribing
waivers. As interventions are developed and tested, healthcare providers,
public health officials and policy makers need to expect that transcribing
potential urban solutions into rural settings will be difficult given the many
differences in lifestyle and circumstances among rural and urban residents,
Further study is needed to develop rural-specific solutions.
The literature reviewed did not provide
evidence of prescribing factors of Nurse Practitioners, Certified Nurse
Midwives and Physician Assistants and how this may influence the accessibility
to drug treatment in rural areas. As more data is collected on the prescribing
practices of waivered healthcare providers beyond physicians, it will be
critical to conduct research to see if these types of prescribers will help
meet the needs for MAT in rural areas. Policy makers should ensure that all
qualified healthcare providers, not only physicians, are able to provide MAT in
order to improve treatment access to people in rural areas. Reports continue to
come forth regarding the work being done to overcome barriers to providing MAT,
particularly buprenorphine, in rural areas [29].
Strengths of this systematic review include
the wide search for peer-reviewed literature on the chosen topic. This review
establishes baseline data with which to compare future research. The review
also establishes the current state of knowledge and identifies gaps in the
literature to date. The topic of opioid use and misuse is crucially important
and has been identified as a public health crisis. Exploring the trend of
opioid addiction in rural areas along with approaches for prevention and
treatment progress are needed to meet the goals of public health.
1. Ahrnsbrak R, Bose J, Hedden SL, Lipari RN, Park-Lee E (2017) Key
substance use and mental health indicators in the United States: Results from
the 2016 national survey on drug use and health (HHS Publication No. SMA
17-5044, NSDUH Series H-52). Rockville, MD: Center for Behavioral Health
Statistics and Quality, Substance Abuse and Mental Health Services
Administration.
2. Centers for Disease Control and Prevention (2018) U. S. Prescribing Rate
Maps.
3. American Nurses Association (2018) Practice & Policy. American
Nurses Association Website.
4. Noonan R (2018) Rural America in crisis: The changing opioid overdose
epidemic. CDC Website.
5. National Advisory Committee on Rural Health and Humand Services (2016)
Families in crisis: The human service implications of rural opiod misuse.
Rockville: Health Resources & Services Administration.
6. Moher D, Liberati A, Tezlaff J, Altman D (2009) Preferred reporting
items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 339:
332.
7. Tran KP, Nguyen Q, Truong XN, Le V, Le VP, et al. (2014) A comparison of
ketamine and morphine analgesia in pre-hospital trauma care: A cluster
randomized clinical trial in rural Quang Tri Province, Vietnam. Prehospital
Emergency Care 18: 257-264.
8. Andrilla CHA, Coulthard C, Larson EH (2017) Barriers rural physicians
face prescribing buprenorphine for opioid use disorder. Ann Fam Med 15:
359-362.
9. Berends L, Larner A, Lubman DI (2015) Delivering opioid maintenance
treatment in rural and remote settings. Austr J Rural Health 23: 201-206.
10. Brown JD, Goodin AJ, Talbert JC (2018) Rural and Appalachian disparities
in neonatal abstinence syndrome incidence and access to opioid abuse treatment.
J Rural Health 34: 6-13.
11. Cochran GT, Engel RJ, Hruschak VJ, Tarter RE (2017) Prescription opioid
misuse among rural community pharmacy patients: Pilot study for screening and
implications for future practice and research. J Pharmacy Pract 30: 498-505.
12. Cerdá M, Gaidus A, Keyes KM, Ponicki W, Martins S, et al. (2017)
Prescription opioid poisoning across urban and rural areas: Identifying
vulnerable groups and geographic areas. Addiction 112: 103-112.
13. Dick AW, Pacula RL, Gordon AJ, Mark Sorbero, Rachel M, et al. (2015)
Growth in buprenorphine waivers for physicians increased potential access to
opioid agonist treatment, 2002-11. Health Affairs 34: 1028-1034.
14. Hirchak KA, Murphy SM (2017) Assessing differences in the availability
of opioid addiction therapy options: Rural versus urban and American Indian reservation
versus non-reservation. J Rural Health 33: 102-109.
15. Karp JF, Lee CW, McGovern J, Stoehr G, Chang CCH, et al. (2013) Clinical
and demographic covariates of chronic opioid and non-opioid analgesic use in
rural-dwelling older adults: The MoVIES project. Int Psychogeriatr 25:
1801-1810.
16. Netherland J, Hansen HV (2016) The war on drugs that wasn’t: Wasted
whiteness, “dirty doctors” and race in media coverage of prescription opioid
misuse. Cult Med Psychiatry 40: 664-686.
17. Pattison-Sharp E, Estrada RD, Elio A, Prendergast M, Carpenter DM (2017)
School nurse experiences with prescription opioids in urban and rural schools:
A cross-sectional survey. J Addict Dis 36: 236-242.
18. Prunuske JP, St Hill CA, Hager KD, Lemieux AM, Swanoski MT, et al.
(2014) Opioid prescribing patterns for non-malignant chronic pain for rural
versus non-rural US adults: A population-based study using 2010 NAMCS data. BMC
Health Serv Res 14: 563.
19. Rigg KK, Monnat SM (2015) Urban vs. rural differences in prescription
opioid misuse among adults in the United States: Informing region specific drug
policies and interventions. Int J Drug Policy 26: 484-491.
20. Rosenblatt RA, Andrilla CH, Catlin M, Larson EH, Andrilla CHA (2015)
Geographic and specialty distribution of US physicians trained to treat opioid
use disorder. Ann Fam Med 13: 23-26.
21. Smith RV, Young AM, Mullins UL, Havens JR (2017) Individual and network
correlates of anti-social personality disorder among rural nonmedical
prescription opioid users. J Rural Health 33: 198-207.
22. Young AM, Jonas AB, Havens JR (2013) Social networks and HCV viremia in
anti-HCV-positive rural drug users. Epidemiol Infect 141: 402-411.
23. Zibbell JE, Hart-Malloy R, Barry J, Fan L, Flanigan C (2014) Risk
factors for HCV infection among young adults in rural New York who inject
prescription opioid analgesics. Am J Public Health 104: 2226-2232.
24. Hutchinson E, Catlin M, Andrilla CHA, Baldwin LM, Rosenblatt RA (2014)
Barriers to primary care physicians prescribing buprenorphine. Ann Fam Med 12:
128-133.
25. Kapoor S, Thorn BE (2014) Healthcare use and prescription of opioids in
rural residents with pain. Rural Remote Health 14: 1-12.
26. Mosher H, Zhou Y, Thurman AL, Sarrazin MV, Ohl ME (2017) Trends in
hospitalization for opioid overdose among rural compared to urban residents of
the United States, 2007-2014. J Hosp Med 12: 925-929.
27. Monnat SM, Rigg KK (2016) Examining rural/urban differences in
prescription opioid misuse among US adolescents. J Rural Health 32: 204-218.
28. Wang KH, Becker WC, Fiellin DA (2013) Prevalence and correlates for
non-medical use of prescription opioids among urban and rural residents. Drug
Alcohol Dependence 127: 156-162.
29. Andrilla CHA, Moore TE, Patterson DG, Larson EH (2019) Geographic
distribution of providers with a DEA waiver to prescribe buprenorphine for the
treatment of opioid use disorder: A 5 year update. J Rural Health 35: 108-112.
30. Bebinger M (2019) Fentanyl-linked deaths: The U.S. opioid epidemic’s
third wave begins.
31. Spencer MR, Warner M, Bastian BA, Trinidad JP, Hedegaard H (2019) Drug
overdose deaths involving fentanyl, 2011-2016. Natl Vital Statistics Rep 68:
1-19.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Journal of Allergy Research (ISSN:2642-326X)