742
Views & Citations10
Likes & Shares
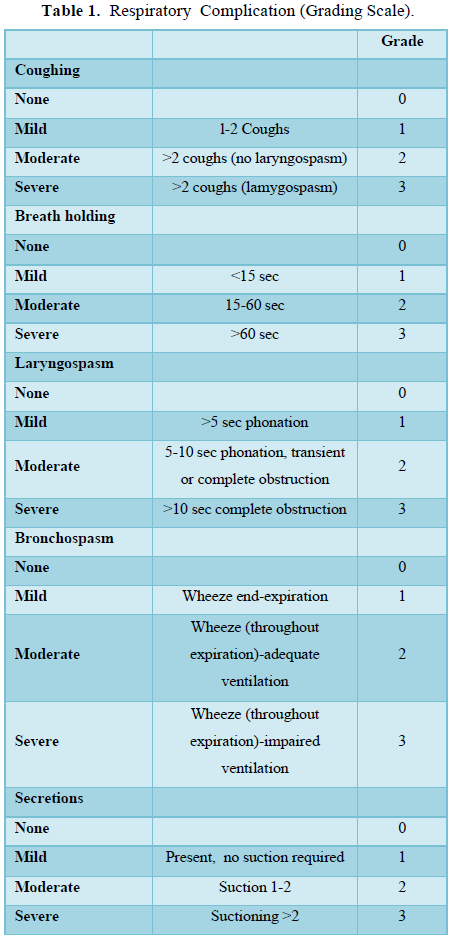
Statistical analysis
The data analyzed using Statistical Package for Social Science (SPSS) version 26.
Demographic data were compared using Statistical t-test. Data presented by frequency and percentage. The incidence, severity of respiratory.
Complications and episodes of arterial oxygen desaturation were analyzed using Mann-Whitney U test and Chi-squared analysis. Statistical significance was a P < 0.05.
RESULTS
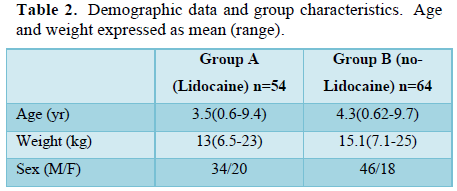
There were no demographic differences between groups (Table 2). The incidence and severity of respiratory complications occurring in emergence were recorded in Table 3.
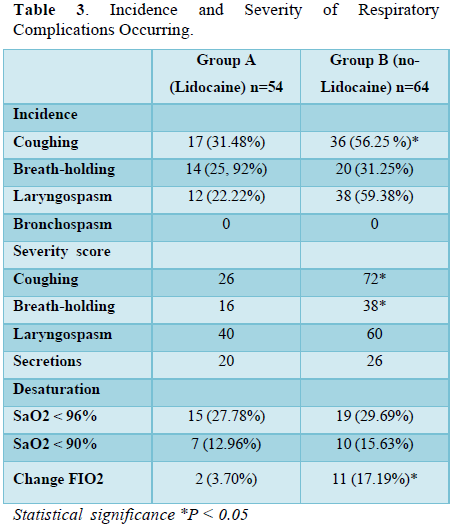
The incidence and severity of cough were greater in Group B (no-Lidocaine) (P < 0.05). In Group A (Lidocaine) 31% of children (17/54) coughed, compared with 56% of children (36/64) in Group B (no-Lidocaine). Coughing severity score of 2 or 3 was recorded in 6% children (Group A), and 33% children (Group B). Coughing severity score of 3 occurred in 7% children (Group A), and 26% children (Group B).
Episodes of breath-holding were longer in Group B (no-Lidocaine) (P < 0.05). Moderate breath-holding (15-60 sec) and severe breath-holding (>60 sec) (severity score of 2 or 3) occurred with two children in Group A, compared with 14 children (26%) in Group B.
There was a high incidence of laryngospasm in Group A (Lidocaine), i.e. 52% of children (28/54), compared to Group B (no-Lidocaine) 59% of children (38/64) (P > 0.05).
A higher incidence (17%) (P < 0.05) of respiratory complications requiring change to 100% oxygen occurred in Group B (no-Lidocaine) compared to 4% of children in Group A (Lidocaine).
There were no differences between groups (Group A vs. Group B) with regard to the incidence of breath holding (26% vs. 31%), and secretions (30% vs. 31%), (P > 0.05).
Episodes of oxygen desaturation that occurred in both groups were not different (P >0.05). Oxygen saturation (SaO2) <96% occurred in 28% of children (15/54) (Group A), and 30% of children (19/64) (Group B). Oxygen saturation (SaO2) <90% occurred in 13% of children (7/54) (Group A), and 15.6% of children (10/64) (Group B).
DISCUSSION
The most commonly used inhalational anesthetic agents, Desflurane and Sevoflurane, substantially more expensive than isofurane [12]. However, Isolurane is also used for induction and maintenance of anesthesia. But, because of its pungency, it is irritant to the airways, causing cough, breath-holding, laryngospasm and episodes of arterial oxygen desaturation [13,14].
These problems are more prevalent in pediatric population, especially unpremedicated patients [15-17].
Methods of topical lidocaine application included lidocaine spray onto the larynx, lidocaine spray to the supraglottic [18], glottic and subglottic areas, aerosol administration [19] or lidocaine jelly placed on the dorsal surface of the supraglottic airway device [20].
The use of IV lidocaine, compared with placebo, led to a large reduction in the incidence and severity of postoperative complications after Isoflurane anesthesia, The incidence and severity of coughing, and the incidence of laryngospasm, were greater and the duration of breath-holding was longer in the control group, Group B (no-Lidocaine) than in Group A (Lidocaine) (P< 0.05). There were no differences between groups regarding the incidence of breath-holding, and secretions (P > 0.05).
The exact mechanism of action of IV Lidocaine appears to be unknown. One postulated mechanism could be because of the fact that IV lidocaine suppresses the airway’s excitatory sensory C-fibers and the release of sensory neuropeptides [21], which decrease irritation and inflammation.
IV lidocaine appeared to be safe and did not result in any difference in adverse events.
There are insufficient data to determine a conclusion on the ideal dose of IV lidocaine for the prevention of cough. Both low dose (<1.5mg/kg) and high dose (1.5 mg/kg) represent effective measures for cough prevention with a non-significant statistical difference. However, in our study, we use a dose of 1.5 mg/kg which was reviewed by Clivio and colleagues, who examined the use of IV lidocaine to prevent intubation, extubation, and opioid-induced cough [22]. They reported a large reduction in cough with the use of IV lidocaine at 1.5mg/kg, as we concluded.
CONCLUSION
In conclusion, the use of IV lidocaine decreases the incidence and severity of coughing, the incidence of laryngospasm, the duration of breath-holding, and the need to change to 100% oxygen in pediatrics which was related to Isoflurane pungency. There was no effect on the incidence of secretions or breath-holding. Further work is needed to decide the most appropriate dose, time of administration, and any adverse effect of IV. Lidocaine in pediatrics.
- Phillips AJ, Brimacombe JR, Simpson DL (1988) Anesthetic induction with isoflurane or halothane. Anaesthesia 43: 927-929.
- Neelakanta G, Miller J (1994) Minimum alveolar concentration of isoflurane for tracheal extubation in deeply anesthetized children. Anesthesiology 80: 811e3.
- Lee B, Lee JR, Na S (2009) Targeting smooth emergence: the effect site concentration of remifentanil for preventing cough during emergence during propofol remifentanil anesthesia for thyroid Br J Anaesth 102: 775e8.
- Crerar C, Weldon E, Salazar J, Gann K, Kelly JA, et al. (2008) Comparison of 2 laryngeal tracheal anesthesia techniques in reducing emergence AANA J 76: 425e31.
- Lam F, Lin YC, Tsai HC, Chen TL, Tam KW, et al. (2015) Effect of intracuff lidocaine on postoperative sore throat and the emergence phenomenon: A systematic review and meta-analysis of randomized controlled PLoS One 10: e0136184.
- Burki NK, Lee LY (2010) Blockade of airway sensory nerves and dyspnea in Pulm Pharmacol Ther 23: 279e82.
- Tanelian DL, MacIver MB (1991) Analgesic concentrations of lidocaine suppress tonic A-delta and C fiber discharges produced by acute Anesthesiology 74: 934e6.
- Woolf CJ, Wiesenfeld-Hallin Z (1985) The systemic administration of local anesthetics produces a selective depression of C afferent fiber evoked activity in the spinal Pain 23: 361e74.
- Kamei J, Nakanishi Y, Ishikawa Y, Hayashi SS, Asato M (2011) Possible involvement of tetrodotoxin-resistant sodium channels in cough reflex. Eur J Pharmacol 652: 117-120.
- Poulton TJ, James FM III (1979) Cough suppression by Anesthesiology 50: 470-472.
- Adcock JJ, Douglas GJ, Garabette M, Gascoigne M, Beatch G, et al. (2003) RSD931, a novel antitussive agent acting on airway sensory Br J Pharmacol 138: 40-416.
- Golembiewski J (2013) Economic considerations in the use of inhaled anesthetic agents CIR MAY AMB 18 (2):
- Kingston HGG (1986) Halothane and isoflurane anesthesia in pediatric Anesth Analg 65: 181-184.
- Warde D, Nagi H, Raflery S (1991) Respiratory complications and hypoxic episodes during inhalation induction with isoflurane in Br J Anaesth 66: 327-330.
- Fisher DM, Robinson S, Brett CM, Perin G, Gregory GA (1985) Comparison of enflurane, halothane, and isoflurane for diagnostic and therapeutic procedures in children with Anesthesiology 63: 647-650.
- McAuliffe GL, Sanders D J, Mills PJ (1994) Effect of humidification on inhalation induction with isoflurane in children. Br J Anaesth 73: 587-589.
- Raftery S, Warde D (1990) Oxygen saturation during inhalation induction with halothane and isoflurane in children: Effect of premedication with rectal thiopentone. Br J Anaesth 64: 167-169.
- Staffel JG, Weissler MC, Tyler EP, Drake AF (1991) The prevention of postoperative stridor and laryngospasm with topical lidocaine. Arch Otolaryngol Head Neck Surg 117: 1123-1128.
- Penaloza IV, Diaz MVP, Jimenez TD (1999) Use of beclametazone dipropionate for prevention of post intubation laryngospasm in pediatrics topical lidocaine. Anestesiaen Mexico 11: 162-166.
- O’Neill B, Templeton JJ, CaramicoL, Schreiner MS (1994) The laryngeal mask airway in pediatric patients: Factors affecting ease of use during insertion and Anesth Analg 78: 659-662.
- Solway J, Leff AR (1991) Sensory neuropeptides and airway J Appl Physiol 71: 2077e87.
- Clivio S, Putzu A, Tramer MR (2019) Intravenous lidocaine for the prevention of cough: systematic review and meta-analysis of randomized controlled trials. Anesth Analg 129: 1249e55.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Dermatology Clinics and Research (ISSN:2380-5609)
- International Journal of AIDS (ISSN: 2644-3023)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Oncology Clinics and Research (ISSN: 2643-055X)

