Review Article
Screening by Point of Care Testing: A Critical View for Community Health Service to Evaluate Anemia in Women
1112
Views & Citations112
Likes & Shares
Anemia is a public health problem that affects populations in both rich and poor countries. Although the Primary cause is iron deficiency; it is seldom present in isolation. More frequently it coexists with a number of other causes, such as malaria, parasitic infection, nutritional deficiencies, and Hemoglobinopathies Given the importance of this pathology in the world, numerous countries conduct interventions to reduce anemia; particularly in the groups most susceptible to its devastating effects: Pregnant women and young children. In the last three decades, there have been various attempts to produce estimates of the prevalence of anemia at different levels including at the global level.
Keywords: Point of care testing (POCT), Screening, anemia, Hemoglobin (Hb), Iron deficiency anemia (IDA), Prevalence, Awareness
INTRODUCTION
Anemia is defined as a decrease in the total amount of red blood cells (RBCs) or hemoglobin in the blood leading to lowered ability of the blood to carry oxygen.
Anemia a customary disorder, affecting around 25% of the global population [1]. It affects individual’s wellbeing, physical productivity, and work performance, timely treatment can restore personal health and raise national productivity levels by as much as 20% in developing countries where the prevalence of anemia is the highest [2].
Anemia affects 90.1% of adolescent girls in India; among which 7.1% have severe anemia [3].
Globally, 1.62 billion people are affected by anemia, which correlates to 24.8% of people. In preschool-age girls, the highest prevalence is (47.4%), and in men, the lowest prevalence is (12.7%). The demographic group with the highest number of persons affected, however, is pregnant women (41.8%) [4]. In women, anemia may become the underlying cause of maternal mortality and perinatal mortality [5]. Nearly 50% of women of reproductive age and 26% of men in the 15-59 age groups are anemic [6].
Nine out of ten people suffering from anemia live in developing countries, about two billion people suffer from anemia and an even greater number of people suffer from iron deficiency. In South-East Asia, an alarming 600 million people suffer from iron deficiency anemia, affecting mainly teenage girls, women of reproductive age and young children. The prevalence of the disorder in India is 87% [7].
According to the National Family Health Survey (NFHS)-(III), more than half of India's women (55%) have anemia, including 39% with mild anemia, 15% with moderate anemia and 2% with serious anemia [8].
In fact, anemia also leads to 20% of all maternal deaths. During pregnancy, several countries undertake measures to minimize anemia and its adverse effects [9].
Anemia is an indication of both inadequate nutrition and poor health. The most drastic health consequences of anemia, i.e., increased risk of maternal and infant mortality due to extreme anemia, have been reported. Furthermore, it is important to introduce the negative effects of IDA on children's cognitive and physical development and on physical performance - particularly work productivity in adults [10].
In comparison to clinical tests which are subjective and thus have more room for error, Hb concentration is the most accurate sign of anemia at population level. It is relatively simple and inexpensive to measure Hb concentration and this test is commonly used as a proxy indicator of iron deficiency. Anemia, however, can be induced by causes other than iron deficiency. Furthermore, the mean level of Hb concentration may be lowered in populations where the prevalence of inherited hemoglobinopathies is high. This underlines that if the only measure used is concentration Hb, the etiology of anemia should be viewed with caution. The main goal of the anemia assessment is to provide decision-makers with details on the type of steps to be taken to avoid and monitor anemia. This means that the causes of anemia must be established in addition to the calculation of Hb concentration, given that they may differ according to the population.
The signs are often unclear as anemia progresses slowly and include basic fatigue, exhaustion, and shortness of breath or intolerance to exercise. Secondary blood loss anemia also has greater effects, including fatigue, dizziness, fainting, or elevated thirst or heart failure at periods of high performance. Until a person becomes visibly pale anemia has to be severe. Depending on the underlying cause, extra symptoms can occur [11].
RISK FACTORS AND CAUSES OF ANEMIA
Decreased Secondary to low consumption of iron, poor absorption of iron from diets rich in phytate or phenolic compounds, and lifespan when iron needs are particularly high in micronutrient deficiencies (i.e., growth and pregnancy), including vitamins A and B12, folate, riboflavin, and copper.
Blood loss anemia due to trauma gastrointestinal bleeding Severe menstrual blood loss (gynecological causes) or parasitic infections such as hookworms, ascaris, and schistosomiasis, acute and chronic infections, including malaria, cancer, tuberculosis, and HIV, may also decrease blood Hb levels.
Haemoglobinopathies contribute to accelerated degradation. Impaired production of RBC leaded by pure red cell aplasia, aplastic anemia, anemia of renal failure, anemia of endocrine disorders.
Myelophthisic anemia, myelodysplastic syndrome, chronic inflammation, congenital dyserythropoietic anemias are other causes impaired proliferation and maturation of erythroblasts.
Nutritional and infectious causes of anemia are the primary factors. Among the nutrition factors that lead to anemia, iron deficiency is the most common. It is due to a diet that is monotonous but rich in substances (phytates) that prevent the absorption of iron, so that the body cannot use dietary iron. Iron deficiency can also be exacerbated by poor nutritional status, especially when it is associated with deficiencies in folic acid, vitamin A or B12, as is often the case in populations living in developing nations. Malaria is another significant cause of anemia when it comes to infections: it affects 300-500 million people, and in endemic areas it can be the primary cause of half of all serious. Hookworm infection and schistosomiasis also lead to anemia in some areas. Approximately 44 million pregnant women have hookworm infections, and schistosomiasis seriously infects 20 million citizens. Anemia may also be attributed to significant loss of blood, such as diarrhea-associated gastrointestinal infections. Malnutrition and water-borne or water-mediated diseases are the most significant causes of anemia mediated to the water. In India, anemia prevalence is high due to low dietary intake, poor iron intake (less than 20 mg / day) and folic acid intake (less than 70 micrograms / day); poor iron bioavailability (3-4% only) in the Indian diet rich in phytate fiber; and chronic blood loss due to infection such as malaria and hookworm infestations. The low dietary intake of iron and folic acid coupled with poor bioavailability of iron is the major factor responsible for very high prevalence of anemia in the country [12,13].
OBJECTIVES
To evaluate hemoglobin in women residing at Girinagar, Pune by POCT by cross sectional study.
MATERIALS AND METHODS
110 women participated voluntarily in a medical camp of “well women’s clinic” at Girinagar, Pune. The participants were of different age group and pre-registered a week before.
Consent was provided by all the participants and involved in the study voluntarily with their full will.
This data has been obtained from a medical camp conducted at DIAT-DRDO, Girinagar, and Pune-25. Hence it is not applicable.
Estimation of hemoglobin rendered using portable photometer Hem cue (Hb 201 system). The hemostatic hemoglobin device consists of disposable micro cuvettes containing a dry reagent and a photometer built for a single function.
It is based on the idea that a modified azide-methemoglobin reaction is the reaction mixture in the cuvette. Sodium deoxycholate disintegrates the membranes of the erythrocytes, releasing the hemoglobin. Sodium nitrite transforms the hemoglobin iron from the ferrous to the ferric state into met hemoglobin, which then combines to form azide-methemoglobin with azide. The photometer employs a double wavelength measuring process, 570 nm and 880 nm, for turbidity compensation [14].
Under aseptic precautions, the capillary sample was collected from the lancet with a penetration depth of 1.5 to 2 mm (to ensure sufficient blood flow) on the fleshy portion of the non-dominant hand side of the middle or ring finger, assisted by the operator after gentle massage with light pressure maintenance to achieve a strong penetration.
They cleaned away the first two drops of blood, using a clean lint-free sterile gauze pad. As it produces incorrect effects, thinning and clotting of the blood must be prevented. Within 30 to 45 seconds following the puncture, a strong capillary flow is observed. The third drop in blood used to measure hemoglobin.
FACTORS INFLUENCING THE MEASUREMENT [15,16]
Variability in reported hemoglobin values can be caused by a number of physiological factors and pre-analytical errors. The physiological factors affecting POCT results are capillary blood has higher Hb than venous blood, especially in women and in men with severe iron depletion (median +0.67 g/dL or +6.7 g/L for iron-depleted women to -0.1 g/dL or -1 g/L for iron-repleted men). Venous blood has a slightly higher Hb than arterial blood. Finger-stick sampling has been shown to more closely approximate venous Hb values, while ear-stick sampling tends to give higher results. Tourniquet use longer than 30 seconds increases venous hemoglobin value. Hb is higher in blood samples from standing subjects than in samples from sitting or supine subjects. Hb tends to be higher in the morning and decreases throughout the day.
RESULTS
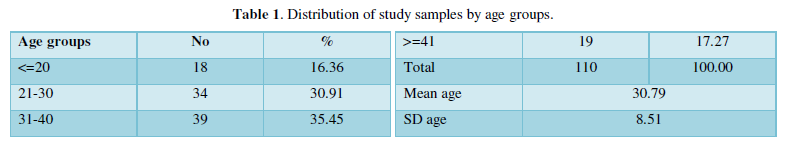
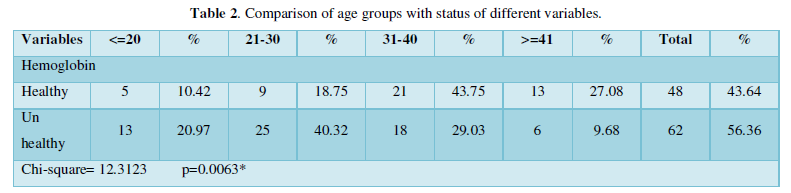
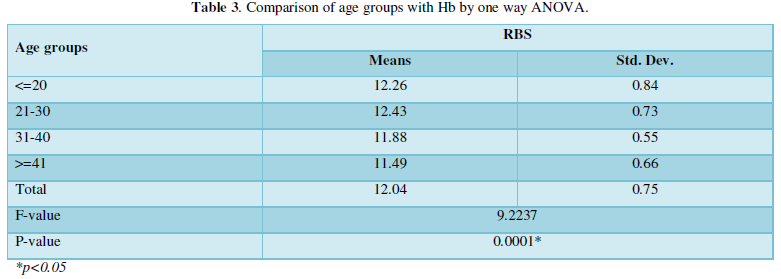
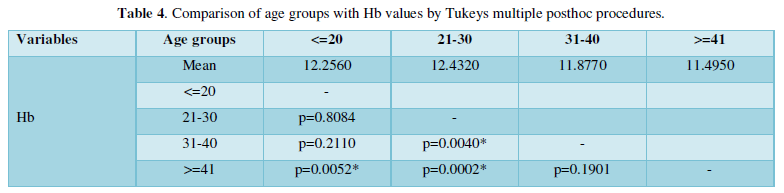
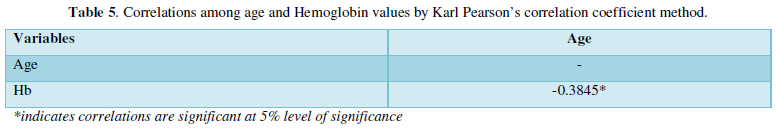
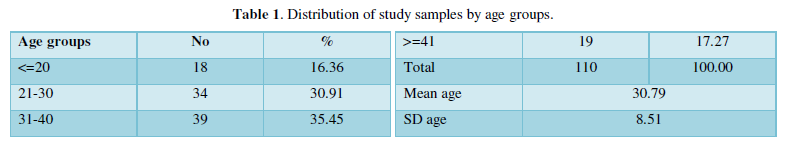
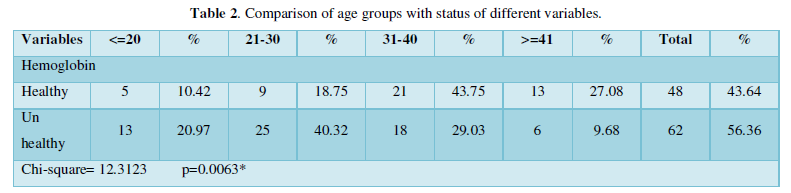
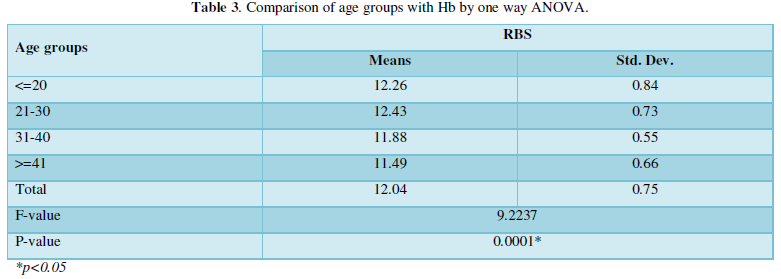
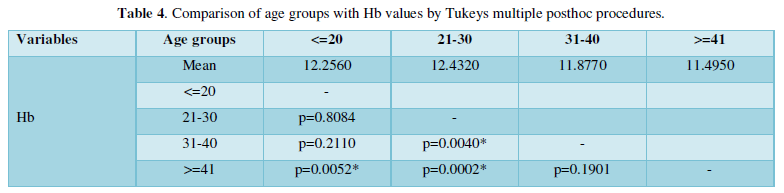
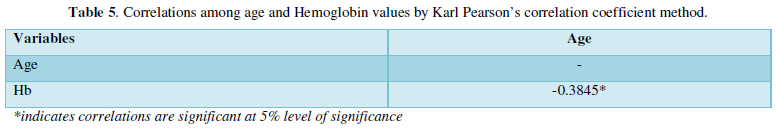
Collected data was analyzed by Tukeys multiple posthoc procedures, ANOVA and Karl Pearson’s correlation coefficient method (Table 1-5).
DISCUSSION
There have been numerous attempts over the last three decades to generate estimates of the prevalence of anemia at different levels, including at global level, but up to now there has never been a systematic analysis of all the data collected and published with the intention of deriving regional and global estimates. It's shocking that there are multiple countries missing national prevalence data considering the public health significance of anemia.
In the general population, food-based approaches to growing iron intake through food fortification and dietary diversification are effective, sustainable strategies for preventing IDA.
The largest group of the 110 participants ranged from 31-40 years of age. The typical range of hemoglobin for Indian scenario is between 12-14g / dL. 56% of women had levels of Hb well below 12g / dL and 44% of women had levels of Hb that were common. Highest prevalence was observed among the anemic women in the 21-30-year age group. Therefore, the peak reproductive community has been more affected. The findings obtained were therefore statistically relevant evaluated by several posthoc procedures by ANNOVA & Turkey’s in one way.
Given the multifactorial nature of this condition, sometimes an integrated approach is required to correct anemia. To combat it effectively, we need to recognize and resolve the contributing factors. In settings where iron deficiency is the most frequent cause, vulnerable groups typically obtain additional iron intake through iron supplements; in particular, pregnant women and young children. In addition, hematopoietic supplementation of vitamin B12 (Cyanocobalamin) and folic acid after anemia has been typed is required. In addition to these minerals such as copper & zinc vitamin C, they also affect the metabolism of iron.
CONCLUSION
The advantages of early detection by screening of asymptomatic individuals are shown through screening in a clinical environment of people at high risk.
Clinicians should also be diligent in assessing suggestive clinical presentations of anemia, and in determining the underlying cause.
Diagnosis of anemia is of utmost importance for better maternal and fetal outcome in reproductive age groups.
The undiagnosed cases can continue for decades along with low hemoglobin values, affecting oxygenation of the tissue. Thus, at the first clinic visit, specifically female (house wives) residents of the peripheral area, uneducated with ignorant attitude must be screened on a compulsory basis. Such is the case.
COMPETING INTERESTS
Authors have declared that no competing interests exist.
- Stedman TL (2006) Stedman's medical dictionary (28th) Philadelphia: Lippincott Williams & Wilkins p. Anemia. ISBN 9780781733908.
- Smith RE Jr (2010) The clinical and economic burden of anemia. Am J Manag Care. 16: S59-S66.
- Toteja GS, Singh P, Dhillon BS, Saxena BN, Ahmed FU, et al. (2006) Prevalence of anemia among pregnant women and adolescent girls in 16 districts of India. Food Nutr Bull 27(4): 311-315.
- de Benoist B, McLean E, Egli I, Cogswell M (2008) WHO global database on anemia. Retrieved on: February 6, 2014. Available online at: http://whqlibdoc.who.int/publications/2008/9789241596657_eng.pdf
- Ezzati M, Lopez AD, Rodgers A, Hoorn SV, Murray CJL (2002) Selected major risk factors and global and regional burden of disease. Lancet 360: 1347-1360.
- Beard JL, Hendricks MK, Perez EM, Murray-Kolb LE, Berg A, et al. (2005) Maternal iron deficiency anemia affects postpartum emotions and cognition. J Nutr 135: 267-274.
- Capoor I, Gade J (2000) CHETNA Team, Paper presented at the World Congress on Women’s Health on November 10th, 11th & 12th, 2000 at Science City, Calcutta.
- National Family Health Survey (NFHS-III), 2005-2006. Accessed on: February 4, 2014. Available online at: http://www.nfhsindia.org/pdf/India.pdf
- The National Nutritional Anemia Prophylaxis Programme (NNAPP) was launched in 1972 during the 4th five-year plan in India with the aim to curb the prevalence of anemia.
- World Health Organization (2001) Iron deficiency anemia: assessment, prevention, and control. A guide for programme managers. Geneva. Available online at: https://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf
- Janz TG, Johnson RL, Rubenstein SD (2013) Anemia in the emergency department: Evaluation and treatment. Emerg Med Pract 15(11): 1-15; quiz 15-16.
- National Nutrition Monitoring Bureau. NNMB Micronutrient Survey. National Institute of Nutrition, Hyderabad (2002).
- Indian Council of Medical Research, Micronutrient Profile of Indian Population, New Delhi, (2004).
- Vanzetti G (1966) An azide-methemoglobin method for hemoglobin determination in blood. J Lab Clin Med 67(1): 116-126.
- Cable RG, Steele WR, Melmed RS, Johnson B, Mast AE, et al (2012) NHLBI Retrovirus Epidemiology Donor Study-II (REDS-II). The difference between fingerstick and venous hemoglobin and hematocrit varies by sex and iron stores. Transfusion 52(5):1031-1040
- World Health Organization (2011) Hemoglobin concentrations for the diagnosis of anemia and assessment of severity. Vitamin and Mineral Nutrition Information System. Geneva. Available online at: http://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf?ua=1
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)

