Review Article
A Ten-Year Review of Palliative Procedures for Congenital Heart Diseases in KATH Kumasi: The Need for a Paradigm Shift in Africa
1041
Views & Citations41
Likes & Shares
Background: Congenital heart disease (CHD) is one of the leading causes of infant death from congenital malformations. The incidence of CHD is about 8 cases per 1,000 live births with a higher absolute number in African countries. The fifty-four countries in Africa have an estimated total annual CHD birth prevalence of 300,486 cases. Out of this 51.4% of the continental birth prevalence occurs in only seven African countries. CHD primarily remains a pediatric health issue in Africa because of the deficient health-care systems. Insufficient infrastructure adds to the list of obstacles to open-heart surgery (OHS) in this region. Africa has one Cardiac-Centre for 50 million inhabitants. Komfo Anokye Teaching Hospital (KATH), Kumasi provides surgical and perioperative care to CHD patients going for OHS from the Ashanti region, other regions of Ghana as well as neighboring countries. The purpose of this study was to describe the types of palliative surgical procedures performed in the last ten years, to compare the change in trends before and after 2014, to assess the efficiency and quality of palliative care provided patients with congenital heart diseases in a low resource setting at KATH, Kumasi.
Methods & methods: A retrospective study from 2007 to 2016 involved 118 patients from either sex, undergone OHS under general anesthesia after obtaining approval from Committee on human research publications and ethics.
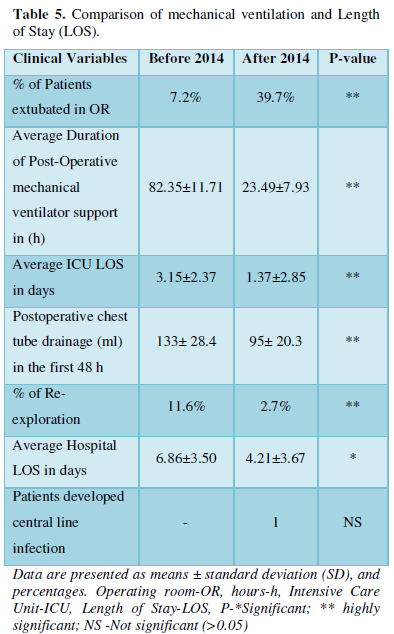
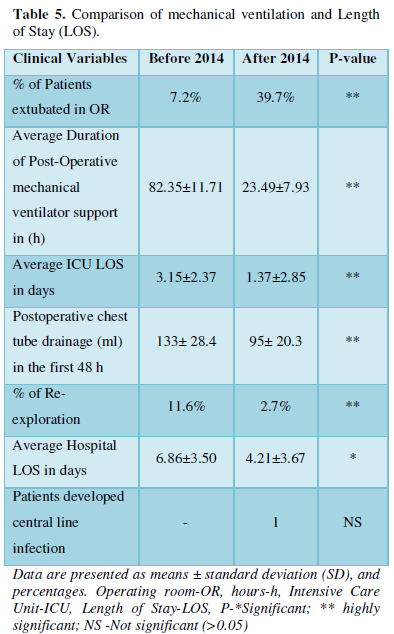
Results: The average Intensive Care Unit (ICU) Length of Stay (LOS) in days and average hospital LOS in days were (3.15±2.37 and 1.37±2.85), and (6.86±3.50 and 4.21±3.67) before 2014 and after 2014 respectively. Increase in the number of on-table extubations from 7.2% to 39.7% whereas a decrease in average mechanical ventilation time from 82.35±11.71 to 23.49±7.93 h in the group after 2014. Postoperative chest tube drainage in the first 48 h decreased from 133±28.4 to 95± 20.3 ml and re-exploration from 11.6% to 2.7%, which reduced postoperatively bleeding and re-exploration with the use of tranexamic acid after 2014.
Conclusion: The surgeries that have been performed provided good palliation for congenital heart diseases in this environment thus there is a need for a paradigm shift to achieve long-term sustainability of OHS in Africa.
Keywords: Congenital heart disease, Kumasi, Open-heart surgery, Palliative procedure, Paradigm shift
Abbreviations: ACC: Aristotle comprehensive Complexity; ASD: Atrial septal defect; BSA: Body surface area; CHD: Congenital heart disease; DORV: Double outlet right ventricle; F: Female; h: Hours; ICU: Intensive Care Unit; Kg: Kilogram; KATH: Komfo Anokye Teaching Hospital; M: Male; m: Meters; NCTC: National Cardiothoracic Centre; NYHA: New York Heart Association; NCD: Non-communicable diseases; NS: Not significant; OHS: Open-heart surgery; PDA: Patent ductus arteriosus; PFO: Patent foramen ovale; PS: Pulmonary stenosis; RHD: Rheumatic heart disease; SD: Standard deviation; TXA: Tranexamic acid; UNDP: United Nations Development Program; VSD: Ventricular septal defect; WHO: World Health Organization
INTRODUCTION
Congenital heart disease (CHD) is the most common class of major congenital malformations. Although there is a slight variation between many population-based studies, CHD affects ≈1% of or about 40,000 live births per year in the United States [1].
The incidence of CHD is 6-13 per 1000 live births in sub-Saharan Africa. In Ghana, the estimated burden of CHD is in the region of 372 per million of the population [2]. In addition to CHD, the prevalence of acquired rheumatic heart disease (RHD) is also high in Africa and Asia. It ranges from 2.7 to 20/1,000 population. According to the World Health Organization (WHO), in developing countries, RHD attacks more than four million people and causes about 90,000 deaths per year [3], which is quite different from the developed world. During the next 20-40 years, low- middle-income countries will be confronted with the persistence of RHD [4]. We know from the current United Nations Development Program (UNDP) data that roughly 70 million children may die before reaching their 5th birthday and most will be from sub-Saharan Africa [5]. These together cause a problem even more complex and bigger in Africa.
There has been a 50% global decrease in the incidence of preventable deaths of children since 1990. However, the mortality from non-communicable diseases (NCD) such as CHD has not changed. Of the estimated 1.3 million children born with CHD annually, over 90% do not have access to cardiac care [5]. The high fertility rate in much of sub-Saharan Africa leads to a disproportionate number of children born with CHD in this part of the world [2]. Many such children have no geographical or financial access to medical and surgical treatment.
Only three West-African countries have regular open-heart surgery activity, including centers in Ghana (National Cardiothoracic Center -Accra), Senegal (Centre Cardio-Pédiatrique Cuomo- Dakar) and Cote d’Ivoire (Heart Institute -Abidjan). The average number of operations performed in these three countries is insignificant, faced with the yearly number of cardiovascular patients in West-African countries [1]. Insufficient infrastructure adds to the list of obstacles to open-heart surgery (OHS) in this region. The United States of America (USA) and Europe have one OHS centre per 150 thousand and one million inhabitants, but Africa has one Centre for 50 million inhabitants [7]. Ghana is one of the few low-to-middle-income countries in West Africa that has one officially accredited tertiary center that is the National Cardiothoracic Centre (NCTC) in Accra. Currently, the Komfo Anokye Teaching Hospital (KATH), Kumasi consistently sustains a cardiothoracic program for more than one decade and slowly building towards its independent centre. The Ashanti Region is the third large administrative region in Ghana with a population of more than 2 million [8]. KATH provides surgical and perioperative care to patients with CHD going for OHS. Our efforts have primarily focused on the selection of simple cases in which a life expectancy of less than 1-2 years without corrective surgery. Expectedly, practicing cardiothoracic surgery in such a resource-poor setting has peculiar challenges. Despite challenges, human and economic we sustained our OHS programme. We accepted challenges and promise to continue our services in OHS to develop KATH as a new cardiothoracic centre in Ghana. The purpose of this study was to describe the types of surgeries performed in the last ten years, to compare the change in trends before and after 2014, to assess the efficiency and quality of care provided by the cardiac anesthesiologist in the delivery of care in a low resource setting. This review also discusses how low-middle income countries in Africa with limited resources continue their OHS programme. This needs a paradigm shift to achieve long-term goals.
METHODS
This study was performed through a retrospective chart review of 118 cases out of 121 cardiac surgeries performed from 2007-2016. Patients with insufficient data were excluded from the relevant analysis (in one case the intraoperative record was missing, and three patients’ post-operative records were missing). Institutional approval for the study was obtained from the Komfo Anokye Teaching Hospital (KATH) Committee on human research publications and ethics. KATH is the second-largest teaching hospital in Ghana and the only tertiary institution in the Ashanti region with 1264 beds. (KATH Annual Report, 2019). This study describes the types of surgeries performed in the last ten years, to compare the change in trends before and after 2014, to assess the efficiency and quality of care provided by the cardiac anesthesiologist in the delivery of this care in a low resource setting in Ghana at KATH Kumasi.
RESULTS
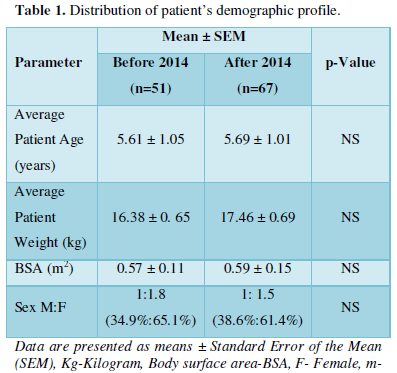
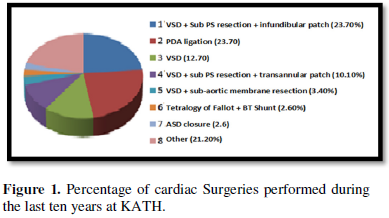
A comprehensive demographic profile of the study population is shown in Table 1. All the demographic profiles in the group before 2014 and after 2014 were comparable. As patients’ average age, weight, body surface area was 5.61 ± 1.05 and 5.69 ± 1.01 years, 16.38± 0.65 and 17.46 ± 0.69 Kg, and 0.57± 0.11 and 0.59 ± 0.15 m2, whereas the male to female ratio before and after 2014 was 1:1.8 and 1:1.5 respectively (p>0.05).
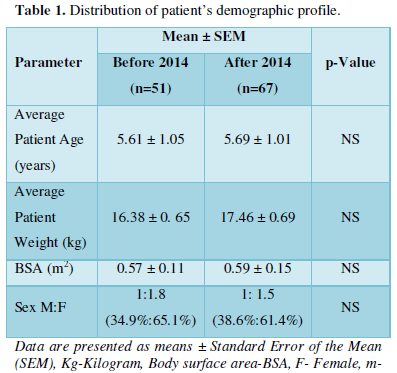
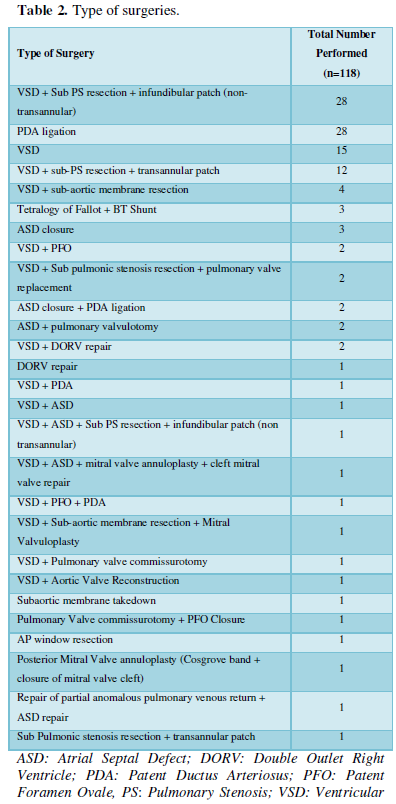
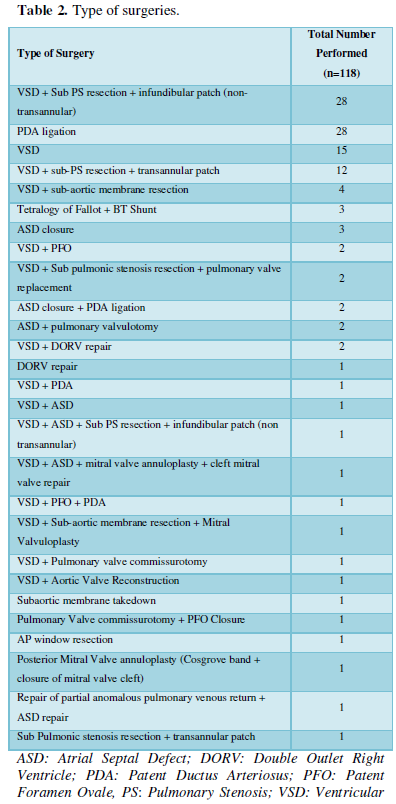
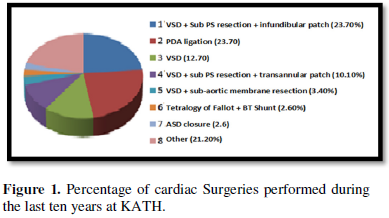
The types of surgeries that have been performed from 2007 till 2016 at Komfo Anokye Teaching Hospital including ventricular septal defect (VSD) closure, atrial septal defect (ASD) closure, patent ductus arteriosus (PDA) ligation, Double outlet right ventricle (DORV) repair and others as shown in Table 2 and Figure 1.
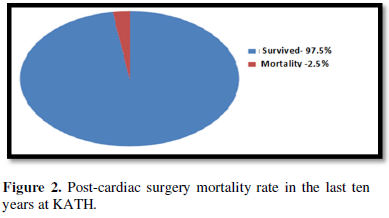
Only three mortalities occurred in the last ten years, which shows a total mortality rate of 2.5%. All mortalities occurred before 2014, first was the result of cerebral malaria, and the rest two were associated with ventilator failure (Figure 2).
Aristotle's comprehensive complexity (ACC) level and NYHA / Ross pre-operative functional class are shown in Table 3. The complexity level of cardiac operations performed in ten years had a mean of 7.1 whereas ACC means before 2014 and after 2014 were 6.9 ± 0.35 and 7.3± 0.32 respectively (p>0.05). They all belong to ACC level 2 as it represents 6.0 - 7.9 as shown in Table 3.
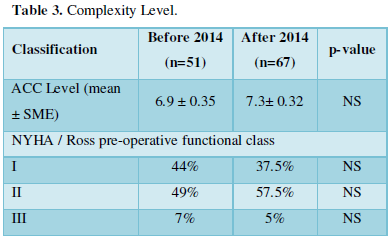
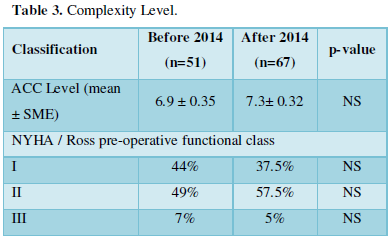
Aristotle comprehensive Complexity - ACC, New York Heart Association –NYHA, P-*Significant; ** highly significant; NS -Not significant (>0.05)
The postoperative percentage of patients extubated in the operating room was 7.2% and 39.2% before 2014 and after 2014 which statistically significantly improved after 2014 (P<0.05).
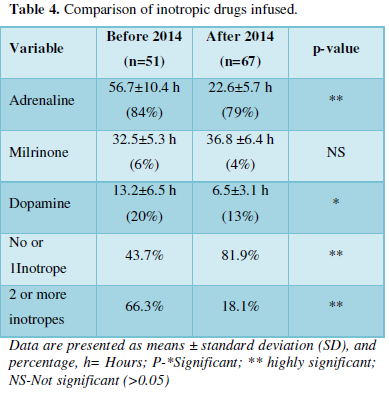
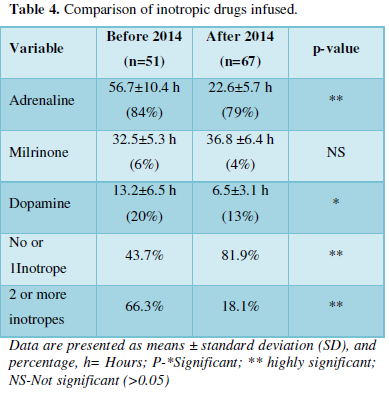
The number and duration of inotropes administered before 2014 and after 2014 groups are shown in Table 4. Adrenaline was the most commonly used in 84% and 79%, and milrinone the least commonly used inotrope 6% and 4% in before 2014 and after 2014 groups respectively. The number of hours adrenaline and dopamine required were significantly lesser after 2014 group (p < 0.05) as shown in Table 4.
The duration of postoperative mechanical ventilator support in hours, average ICU Length of Stay (LOS) in days, and average hospital LOS in days were (82.35±11.71 and 23.49±7.93), (3.15±2.37 and 1.37±2.85), and (6.86±3.50 and 4.21±3.67) before 2014 and after 2014 respectively. Postoperative chest tube drainage in the first 48 hr was significantly less after 2014 (95 ± 20.3ml) as compared with before 2014 (133 ± 28.4 ml) as shown in Table 5 (P<0.05).
DISCUSSION
Anesthesia is a specialty with a severe deficit in many developing countries of Africa and anesthetic services are often underdeveloped [9]. Similarly, it is a well-known fact that the number of the trained pediatric cardiac anesthesiologist in developing countries is very few [10]. Anesthesia is a technology-based specialty and relay on functioning monitoring devices and equipment [11]. Providing anesthesia in developing countries becomes highly challenging because more than 19% of operation theatres in this part of the world have no pulse oximeter [12], basic equipment, and drugs.
We lost two patients due to ventilator failure and one due to cerebral malaria before 2014 study group. The main focus of our anesthetic team is to reduce total perioperative and anesthetic related mortality with the help of evidence-based best practices.
The appropriate selection of cases including patients with simple cardiac defects is one of the most important contributing factors for decreasing morbidity and mortality rate in pediatric cardiac surgery patients in developing pediatric cardiac surgery centers [13]. We selected simple cases as visible from Aristotle comprehensive complexity (ACC) level we had a mean of 7.1 for our cases which represent ACC level 2.
As proved in some studies that fast track surgery and early extubation reduced mortality [13]. Before 2014 on table extubation rate was 7% as compared to after 2014 which was 39%. In our study due to ventilator failure, there was 3.9% mortality before 2014. Simplification of the care and early extubation reduced mortality and complications after 2014.
During pediatric cardiac surgery, a large increase in blood glucose has been reported when exogenous glucose was added intraoperatively. However, when glucose was excluded, hypoglycemia occurred [14]. One of our cases had hypoglycemia due to tight glycemic control before 2014. There is simply not enough evidence to suggest that tight glycemic control would be of benefit in this pediatric patient population because the risks of hypoglycemia are felt to be too great [14]. CPB significantly affects glucose homoeostasis in children, hence it seems prudent to administer a small amount of dextrose in the pre-bypass period to avoid hypoglycemia but the rate and dose of insulin we adjusted with glycemic levels without tight glycemic control due to simplification of the care protocol after 2014.
In cardiac surgery postoperative bleeding is associated with an increased incidence of surgical re-exploration to identify the source of bleeding. Increased use of blood causes significant morbidities such as renal failure, sepsis, arrhythmias, a prolonged requirement for mechanical ventilatory support, longer hospital stay, and increased mortality [13].
The main focus of our anesthetic team was to reduce post-operative complications of bleeding and re-exploration. As many studies suggested the use of tranexamic acid (TXA) safe in pediatric cardiac surgery, TXA effectively reduces postoperative blood loss as well as re-exploration [15,16]. As an evidence-based best practice, we use TXA as a bolus of 20 mg/kg after anesthetic induction and 20 mg/kg after protamine during major surgeries [15]. Postoperative chest tube drainage in the first 48 h decreased from 133±28.4 to 95± 20.3 ml and re-exploration rate from 11.6% to 2.7% in before 2014 and after 2014 groups, respectively. It was reduced significantly with TXA use in the group after 2014 which reduce post-operative complications of bleeding and re-exploration.
The low cardiac output syndrome is a common complication in cardiac surgery patients [17] and inotropic support is frequently initiated to improve post bypass ventricular function. Inotropes may improve hemodynamics, but there is a potential risk for increased myocardial oxygen and energy consumption [17,18]. It has been suggested that an increase in contractility of the hibernating but viable myocardium by low doses of inotropes can lead to a perfusion contraction mismatch with activation of anaerobe glycolysis and eventually myocardial necrosis [19-21]. Thus, the use of inotropes has been associated with adverse clinical outcomes as shown in a few studies. In a study by Fellahi [22] use of dobutamine was associated with increased postoperative morbidity. This has resulted in an ongoing debate on the value or harm associated with the use of inotropes in cardiac surgery [22,23]. The number and duration of inotropes administered before 2014 and after 2014 in our study showed a significant reduction in their use as well as reduced mortality and morbidity of patients. Inotrope management is highly dependent on the patient requirement.
CONCLUSION
The types of surgeries that have been performed from 2007 till 2016 at Komfo Anokye Teaching Hospital including Blalock-Taussig (BT) shunt, ventricular septal defect (VSD) closure, atrial septal defect (ASD) closure, patent ductus arteriosus (PDA) ligation, Double outlet right ventricle (DORV) repair provided good palliation for advanced congenital heart diseases in this environment at KATH. Efforts by the cardiac anesthesia team to diligently avoid anesthetic complications by appropriate selection of cases, minimize post-operative bleeding, and re-exploration through aggressive use of tranexamic acid, on-table extubation, and per-patient basis use of inotropic drugs with caution. All these contributed successes for our group’s experience to serve as a model for others that wish to develop a programme aimed at providing surgical care for patients with congenital heart disease in low- middle- income countries. There is a need for a paradigm shift to achieve the long-term sustainability of OHS in Africa.
COMPETING INTERESTS
The authors declare that they have no competing interests.
- Reller MD, Strickland MJ, Colarusso TR, Mahle WT, Correa A (2008) Prevalence of congenital heart defects in Atlanta, 1998-2005. J Pediatr 153: 807-813.
- Edwin F, Tettey M, Aniteye E, Tamatey M, Sereboe L, et al. (2011) The development of cardiac surgery in West Africa-the case of Ghana. Pan Afr Med J 9: 15.
- Angate KHY (2016) Open heart surgery in sub-Saharan Africa: Challenges and promise. Cardiovasc Diagn Ther 6: 1-4.
- Howson CP, Reddy KS, Ryan TJ, Bale JR (1998) Control of cardiovascular diseases in developing countries. research, development, and institutional strengthening. Washington, DC: Institute of Medicine, National Academy Press. Available online at: https://www.nap.edu/catalog/6218/control-of-cardiovascular-diseases-in-developing-countries-research-development-and
- United Nations Development Program (UNDP) (2020) Accessed on August 10, 2020. Available online at: https://www.undp.org/content/undp/en/home/sustainable-development-goals/goal-3-good-health-and-well-being/targets/
- WHO (2017) Global health observatory data. Causes of child mortality. Accessed on August 10, 2020. Available online at: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/child-mortality
- Pezzella TA (2005) Global expansion of cardiothoracic surgery.The African challenge. Afr Ann Thorac Cardiovasc Sur1: 9-11.
- World Gazetteer online (2020) World-gazetteer.com. Archived from the original on 11 January 2012.
- Walker I, Wilson I, Bogod D (2007) Anesthesia in developing countries. Anaesthesia 62: 2-3.
- Doherty C, Holtby H (2011) Pediatric cardiac anaesthesia in the developing world. Paediatr Anaesth 21: 609-614.
- Hoffman JIE (2013) The global burden of congenital heart disease. Cardiovasc J Afr 24: 141-145.
- Hodges SC, Mijumbi C, Okello M, Mc-Cormick BA, Walker IA, et al. (2007) Anaesthesia services in developing countries: Defining the problems. Anaesthesia 62: 4-11.
- Cvetkovic M (2018) Challenges in pediatric cardiac anesthesia in developing countries. Front Pediatr 6: 254.
- Singh S, Zanwar YN, Okyere I (2020) Does meticulous blood glucose control during cardiopulmonary bypass improves outcome in paediatric patients? EAS J Anesthesiol Crit Care 2: 151-159.
- Zhang Y, Zhang X, Wang Y, Shi J, Yuan S, et al. (2019) Efficacy and safety of tranexamic acid in pediatric patients undergoing cardiac surgery: A single center experience. Front Pediatr 7: 181.
- Singh S, Annamalai A (2017) The efficacy of tranexamic acid versus epsilon amino caproic acid in decreasing blood loss in patients undergoing Mitral valve replacement surgery. J Anesthesiol 5: 11-18.
- Ahmed I, House CM, Nelson WB (2009) Predictors of inotrope use in patients undergoing concomitant coronary artery bypass graft (CABG) and aortic valve replacement (AVR) surgeries at separation from cardiopulmonary bypass (CPB). J Cardiothorac Surg 4: 24.
- Nielsen DV, Hansen MK, Johnsen SP, Hansen M, Hindsholm K, et al. (2014) Jakobsen CJ. Health outcomes with and without use of inotropic therapy in cardiac surgery: Results of a propensity score-matched analysis. Anesthesiol 120: 1098-108.
- Indolfi C, Piscione F, Filardi PP, Prastaro M, Di Lorenzo E, et al. (1996) Inotropic stimulation by dobutamine increases left ventricular regional function at the expense of metabolism in hibernating myocardium. Am Heart J 132: 542-549.
- Schulz R, Rose J, Martin C, Brodde OE, Heusch G (1993) Development of short-term myocardial hibernation. Its limitation by the severity of ischemia and inotropic stimulation. Circulation 88: 684-95.
- Singh S, Okyere I, Singh A (2020) Team-based approach to surgical and anesthetic care for children with congenital heart disease in a low resource setting in Ghana West Africa. RA J Appl Res 6: 2610-615.
- Fellahi JL, Parienti JJ, Hanouz JL, Plaud B, Riou B, et al. (2008) Perioperative use of dobutamine in cardiac surgery and adverse cardiac outcome: Propensity-adjusted analyses. Anesthesiol 108: 979-987.
- Shahin J, DeVarennes B, Tse CW, Amarica DA, Dial S (2011) The relationship between inotrope exposure, six-hour postoperative physiological variables, hospital mortality and renal dysfunction in patients undergoing cardiac surgery. Crit Care 15: R16.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- International Journal of AIDS (ISSN: 2644-3023)



