Review Article
Oral Health Linked to Declining Cognition-A Literature Review
1641
Views & Citations641
Likes & Shares
Aim: This review article aims to update and consolidate the scientific data available regarding the link between cognition and oral health in the elderly population.
Background: A study was conducted to review the articles that focused on the link between oral health and specific cognitive abilities with contributing factors such as cardiovascular disease, inflammatory markers and socioeconomic status in older adults.
Method: A review was undertaken in May 2020. From many potentially relevant articles and literatures, 25 were identified that assessed oral health and at least one of the specific cognitive domains along with at least one cofactor in an older adult cohort study.
Results: The foremost consistent relationships were identified with learning and memory, complex attention, and executive function. For each of those cognitive domains, most studies identified significant unadjusted associations with oral health; where adjustments for covariates were made, a minimum of one among the associations with oral health was present in almost all the studies. In addition, poorer oral health status as determined by clinical examinations was negatively associated with frequency of dental visits. In presence of cardiovascular disease and inflammatory markers in geriatric patients, oral health status has shown poor results.
Conclusions: This review literature mediates evidence of an association between cognitive functions with oral health in old age along with other cofactors like associated systemic disease and socioeconomic status. Thus, understanding that life expectancy is impacted by systemic health and the ‘Geriatric Giants’, the dental professional's role is to make the individual comfortable and maintain function as best possible.
Clinical Significance: The present article will help clinicians better understand the role of cognitive functions in oral health conditions in elderly. Thus, it establishes the opinion that oral health management of the elderly cannot proceed in isolation and requires a multidisciplinary approach.
Keywords: Geriatric Dentistry, Periodontal Health, Edentulous
Abbreviation: DSST: Digital symbol substitution test; MMSE: Mini-Mental State Examination; DWR: Delayed word recall; WF: Word Fluency; HR: High Risk; aHR: Adjusted high risk; OHI-S: Simplified oral hygiene Index.
BACKGROUND
Cognition is critical for functional independence as people age, irrespective of whether a person is independent or dependent. Cognitive abilities can be divided into several specific cognitive domains including attention, memory, executive cognitive function, language, and visuospatial abilities. Prospective memory, specifically remembering to perform intended action in the future (e.g., taking medication after breakfast). Whereas, executive cognitive function is particularly important for novel tasks. These are not associated with a habitual response necessarily, but depends critically on the prefrontal cortex [1]. Cognitive dementia, according to WHO, is a syndrome in which there is deterioration in memory, thinking, behavior, and the ability to perform everyday activity. According to a report published by WHO in September 2019, around 50million of the population have dementia [2]. this is the major reason behind dependency and disabilities during the old age.
As per the last census report (2011), 104 million (53million female & 51 million male) of population belong to the senior citizens in India. Ageing is a natural biological process which is primarily influenced by our genetic makeup. However, in recent centuries it has become more heavily influenced by social, environmental, economic and medical changes as well as physical and mental health [3]. Age related disabilities and immunodeficiency is related to under-nutritional status in the population below the poverty line [4].
Sir Bernard Isaacs coined the term ‘Geriatric Giant’ in the 1960s to describe categories of impairments in the elderly. Falls were associated with frailty which in turn were associated with neurocognitive decline and delirium as an older person became less agile and in deteriorating health [3]. As dental and oral health issues are a newly recognized burden on the health of the elderly, only scant regard for the implications of overt dental caries and active periodontal infection has occurred [5]. However, as health issues are interconnected, maintaining poor oral health can have consequences that are not immediately evident.
Thus, the present review aims to understand & update the scientific literature regarding the link between cognition and oral health in the elderly population. Different cofactors like cardiovascular disease, diabetes, lifestyle habits are also considered and their roles in the deterioration of the oral health is mentioned.
METHOD
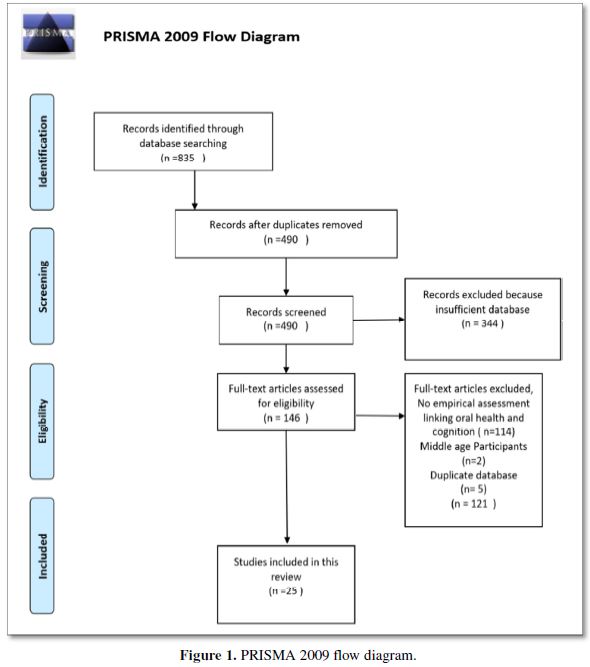
The PRISMA guidelines were followed for a methodological approach and various articles supporting the databases were searched and included. Various articles based on topics cognitive dementia; oral health and aging were assessed and screened. After excluding duplication and studies that could not establish an empirical assessment between cognitive function and oral health, 25 articles were identified for this review.
Inclusion and Exclusion Criteria
- The selected databases are based on Cohort studies that have studied the cognitive function of the older age group (>50years) by standardized DSST (Digital Symbol Substitution test), Mini-Mental State Examination (MMSE), Delayed word recall (DWR) and Word fluency (WF).
- Covariates have been considered like associated disease like cardiovascular disease and diabetes, mental health issue like depression, socioeconomic status and education background, nutrition, demography. The participants were either dependent or community dwellers.
- Oral health assessment scales like OHI-S Index, Periodontal Index, DMFT Index, self-assessment and dental follow-ups at specific time span were included.
- The date of publication of the articles were between 1990-2020. The study designs were Cohort cross-sectional and/or longitudinal with at least one above mentioned covariate.
Data Sources, Search Strategy and Study Selection
A systematic literature search was carried out in the following databases: PubMed, WHO, Medline, ScienceDirect. The keywords used are cognitive psychology, Alzheimer, diabetes, ageing, oral health, periodontal therapy, cardiovascular disease, dementia, attitude, tooth loss, denture problem, and dry mouth. The filter applied in the search included the language (English) and date of publication (1990-2020). A final search was carried out on 28 May 2020 to ensure the most recent literature was included in this review. In addition, the reference lists and bibliographies of all relevant studies were looked for additional sources. The results from the search were organized and duplicate references were removed using the Mendeley bibliographic software. The title and abstract of the remaining studies were assessed by authors independently using the inclusion and exclusion criteria for suitability. In the case where it was difficult to make a decision on the basis of the title and abstract only, the full text was obtained for further assessment. A total of 25 studies which met the inclusion criteria and were included in the review.
Data Extraction
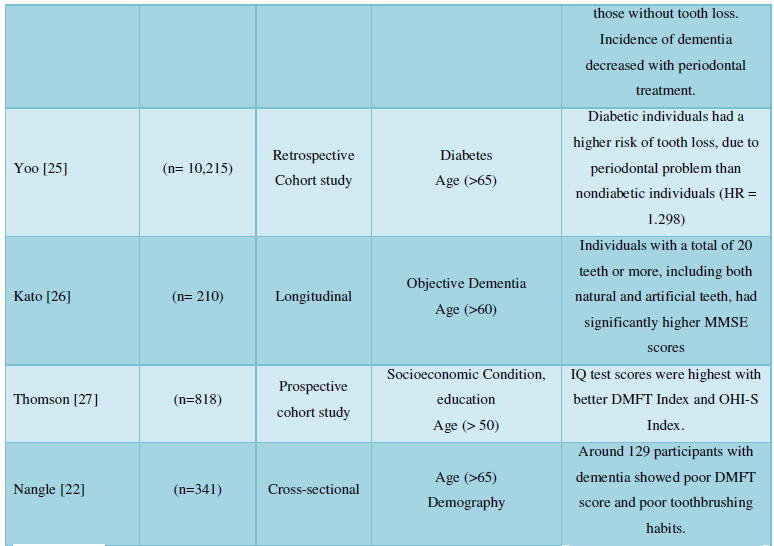
A data extraction form was developed and piloted independently by two authors and modified as required. The information including author, year of publication, country, characteristics of sample/questionnaire and key outcome items was extracted by two authors and checked by one author for accuracy and completeness of the results. There was clear heterogeneity among the studies in their approaches to measuring and reporting the knowledge, attitudes, and practices in reference to oral health care. Therefore, descriptive analysis was administered in most sections and data was pooled to calculate mean percentage wherever studies had similar outcome items to match (Figure 1).
RESULTS
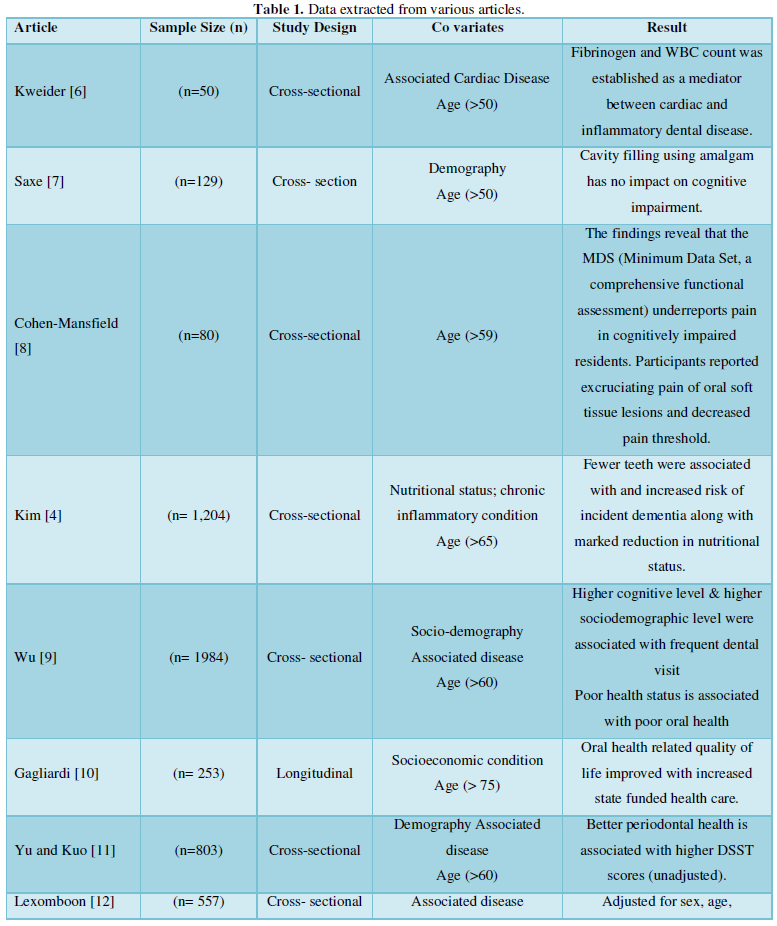
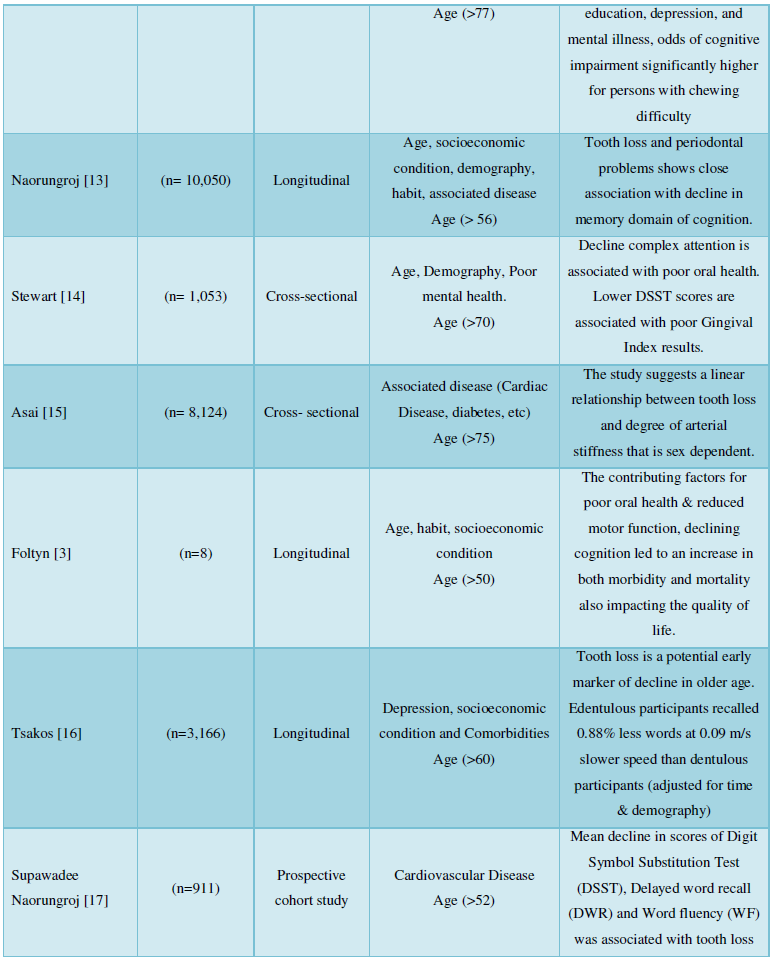
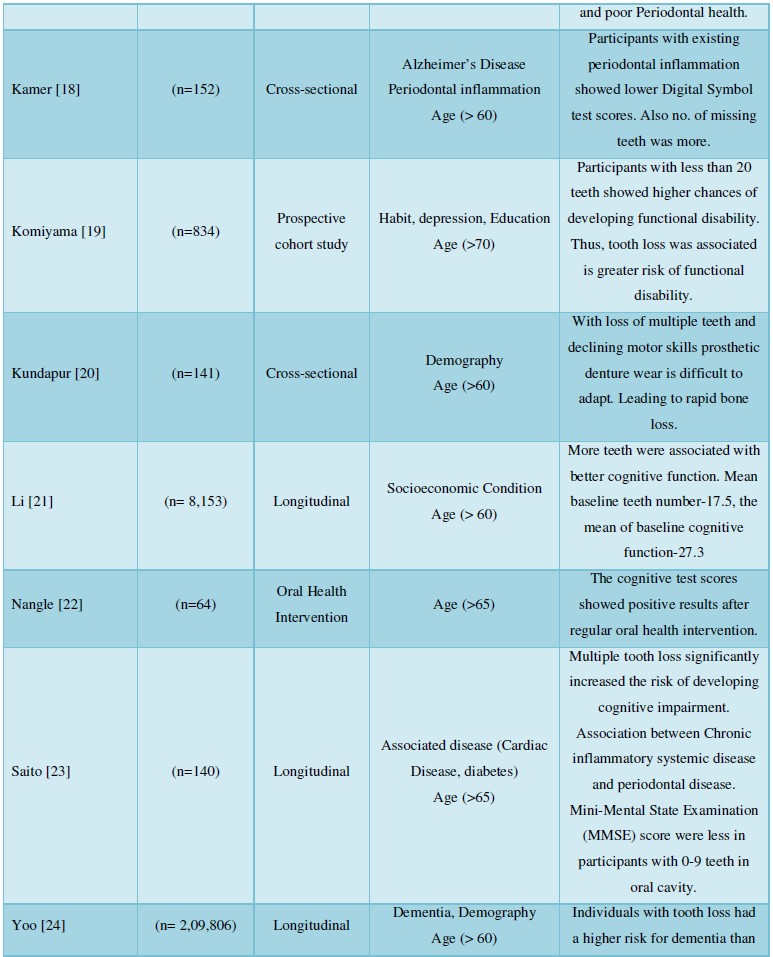
Social cognitive theory and oral health implication have presented its results in 1 study, with covariates of socioeconomic background and tobacco smoking. Covariates like associated disease and risk factor, education and socioeconomic background, smoking and tobacco abuse, nutrition have been considered. Various articles published from the year 1990 to 2020 with a sample size ranging from a minimum of n= 8 to maximum of n=2, 09,806 and participant age ranged 50years and above were compiled.
Cognitive tests using Digit Symbol Substitution Test (DSST) (12 articles) and standardized mini-mental state examination (SMMSE) (10 articles) were used. Cognitive functions of key 6 domains, according to the DSM-5 classification system, were considered for the examination. However, all the 25 articles established a link between cognitive domains of learning & memory (16 articles), executive function (13 articles), complex attention (8 articles) and their implication on the deterioration of oral health.
The participants selected in 23 studies had their oral health assessed by examinations that were conducted in a time interval of 6 months to a year in each of the studies. Periodontal health assessment and number of missing teeth was recorded and considered as standard.
Self- assessment technique was used for 1 study by preparing a questionnaire according to the GOHAI (Geriatric Oral Health Assessment Index) survey. Sample size (n=141) were subjected to 16 questions (4 on physical functions, 5 on psychological, 3 on pain and discomfort) with consent (Table 1).
DISCUSSION
Chronic periodontitis is a widespread peripheral immunoinflammatory condition; it has been proposed to play a significant role in the aggravation of Dementia. An association between peripheral inflammation and dementia was hypothesized by an article published by Kim [4] in the International Journal of Geriatric Psychiatry (2007). It was suggested that chronic systemic inflammation worsened the inflammatory processes in the brain. This was mainly attributed to increased levels of pro-inflammatory mediators, such as interleukin-1, interleukin -6 and tumor necrosis factor-α in the plasma [5]. The contributing factors for poor oral health like dental caries, acute and chronic periodontal infections and compromised systemic health causing xerostomia, reduced fine motor function [28]. Thus, the declining cognition and motivation may not only lead to both morbidity and mortality but also impact on quality of life.
Associated health problems like cardiovascular disease, diabetes and other chronic inflammatory systemic disease have shown unfavorable outcomes like plaque accumulation, periodontal disease followed by tooth loss. Oral health in later life is one of the significant determinants of quality of life (QoL) and life satisfaction as well as a key health status indicator related to functional limitations and limited daily activities [29]. When elderly become care dependent, their oral health often deteriorates due to neglect of oral (self) care. Socioeconomic factor also plays a key factor amongst this population that forms a contributing factor. The lack of attention for oral care can lead to poor oral health and can be considered a hidden health hazard as dental awareness and oral health has been shown to significantly contribute to general health and quality of life.
With age, changes in biological and physiological aspects are inevitable. There are ample of evidences that show alterations in brain structure and performance are intimately tied to alterations in cognitive function. Crystallized intelligence refers to skills, ability, and knowledge that are overlearned, well-practiced, and familiar. Crystallized abilities like vocabulary and general knowledge remain stable or gradually improve at a rate of 0.02 to 0.003 standard deviations per year through the sixth and seventh decades of life. Fluid cognition is a person’s natural ability to process and learn new knowledge, solve problems, attend to and control one’s environment. Post the third decade of life i.e., the peak, fluid cognition, especially psychomotor ability and processing speed declines at an estimated rate of - 0.02 standard deviations per year [30].
Just as age-related changes in brain structure and performance aren't uniform across the entire brain or across individuals; age-related changes in cognition aren't uniform across all cognitive domains or across all older individuals. The basic cognitive functions most suffering from age are attention and memory. Attention is that the means by which we actively process a limited amount of data from the big amount of data available through our senses, our stored memories, and our other cognitive processes. A decline in the domain of attention can have widespread effects on one’s ability to function adequately and efficiently in their daily life.
The prevalence of cardiovascular disease (CVD) is increasing rapidly in the growing aging population. Cardiovascular disease contributes to morphological alteration of the brain that leads to cognitive decline, dementia and cerebrovascular disease. The cognitive decline during this condition is especially a result of the formation of amyloid deposits that provoke neuroinflammation, ultimately leading to necrobiosis [31]. Associations between high blood pressure (BP) and poor performance on neuropsychological tests are well described in the neuropsychological literature particularly in the areas of memory, attention, and executive function. Metabolic-related conditions such as diabetes and obesity have also been associated with cognitive impairment. Periodontal disease, a local inflammatory process is a common oral problem of the older population leading to loss of natural teeth. This local inflammatory process may induce a systemic inflammatory reaction. Therefore, periodontitis could trigger and/or exacerbate an inflammatory condition especially in elderly subjects, resulting in memory impairments, contributing to accelerate the progression of neurodegenerative diseases.
Each of these articles, through cross section analysis (10 studies) and longitudinal studies (8 studies) has established satisfactory results supporting the hypothesis positively. However, none of the articles has considered all the covariates altogether. The database was collected through National health surveys or self-reported. Thus, the uniformity in the measurement is lacking.
CONCLUSION
This review literature mediates evidence of an association between cognitive functions with oral health in old age along with other cofactors like associated systemic disease and socioeconomic status. Elderly with complex care needs experience significantly more oral health problems and are more often edentulous than robust elderly. Moreover, elderly with few teeth and elderly with implant-supported overdentures reported less frailty and better quality of life [32]. However, frequent oral health check-ups for dependent as well as independent aged population can be incorporated for better oral health status. Policies at community level for population of lower socioeconomic background can achieve better quality of life.
ACKNOWLEDGMENT
There are no financial conflicts of interest to disclose.
- Sternberg RJ, Sternberg K (2012) Memory: Models and research methods. Cogn Psychol pp: 185-227.
- World Health Organization (2020) Dementia. Available online at: www.who.int/news‐room/fact‐sheets/detail/dementia
- Foltyn P (2015) Ageing, dementia and oral health. Aust Dent J 60: 86-94.
- Kim J-M, Stewart R, Prince M, Kim S-W, Yang S-J, et al. (2007) Dental health, nutritional status and recent‐onset dementia in a Korean community population. Int J Geriatr Psychiatry 22(9): 850-855.
- Gaur S, Agnihotri R (2015) Alzheimer’s disease and chronic periodontitis: Is there an association? Geriatr Gerontol Int 15(4): 391-404.
- Kweider M, Lowe GD, Murray GD, Kinane DF, McGowan DA (1993) Dental disease, fibrinogen and white cell count; links with myocardial infarction? Scott Med J 38(3): 73-74.
- Saxe SR, Snowdon DA, Wekstein MW, Henry RG, Grant FT, et al. (1995) Dental amalgam and cognitive function in older women: Findings from the Nun Study. J Am Dent Assoc 126(11): 1495-1501.
- Cohen-Mansfield J (2004) The adequacy of the minimum data set assessment of pain in cognitively impaired nursing home residents. J Pain Symptom Manage 27(4): 343-351.
- Wu B, Plassman BL, Liang J, Wei L (2007) Cognitive function and dental care utilization among community-dwelling older adults. Am J Public Health 97(12): 2216-2221.
- Gagliardi D, Slade GD, Sanders AE (2008) Impact of dental care on patients’ treatment goals and quality of life. Aust Dent J 53(1): 26-33.
- Yu YH, Kuo HK (2008) Association between cognitive function and periodontal disease in older adults. J Am Geriatr Soc 56(9): 1693-1697.
- Lexomboon D, Trulsson M, Wårdh I, Parker MG (2012) Chewing ability and tooth loss: association with cognitive impairment in an elderly population study. J Am Geriatr Soc 60(10): 1951-1956.
- Naorungroj S, Slade GD, Beck JD, Mosley TH, Gottesman RF, et al. (2013) Cognitive decline and oral health in middle-aged adults in the ARIC study. J Dent Res 92(9): 795-801.
- Stewart R, Weyant RJ, Garcia ME, Harris T, Launer LJ, et al. (2013) adverse oral health and cognitive decline: the health, aging and body composition study. J Am Geriatr Soc 61(2): 177-184.
- Asai K, Yamori M, Yamazaki T, Yamaguchi A, Takahashi K, et al. (2015) Nagahama Study Group. Tooth loss and atherosclerosis: the Nagahama Study. J Dent Res 94(3_suppl): 52S-58S.
- Tsakos G, Watt RG, Rouxel PL, de Oliveira C, Demakakos P (2015) Tooth loss associated with physical and cognitive decline in older adults. J Am Geriatr Soc 63(1): 91-99.
- Naorungroj S, Schoenbach VJ, Wruck L, Mosley TH, Gottesman RF, et al. (2015) Tooth loss, periodontal disease, and cognitive decline in the Atherosclerosis Risk in Communities (ARIC) study. Community Dent Oral Epidemiol 43(1): 47-57.
- Kamer AR, Fortea JO, Videla S, Mayoral A, Janal M, et al. (2016) Periodontal disease's contribution to Alzheimer's disease progression in Down syndrome. Alzheimers Dement (Amst) 2: 49-57.
- Komiyama T, Ohi T, Miyoshi Y, Murakami T, Tsuboi A, et al. (2016) Association between tooth loss, receipt of dental care, and functional disability in an elderly Japanese population: The Tsurugaya project. J Am Geriatr Soc 64(12): 2495-2502.
- Kundapur V, Hegde R, Shetty M, Mankar S, Hilal M (2017) Effect of loss of teeth and its association with general quality of life using geriatric Oral health assessment index (Gohai) among older individuals residing in rural areas. Int J Biomed Sci 13(1): 6-12.
- Li J, Xu H, Pan W, Wu B (2017) Association between tooth loss and cognitive decline: A 13-year longitudinal study of Chinese older adults. PloS One 12(2): e0171404.
- Nangle MR, Riches J, Grainger SA, Manchery N, Sachdev PS, et al. (2019) Oral health and cognitive function in older adults: A systematic review. Gerontology 65(6): 659-672.
- Saito S, Ohi T, Murakami T, Komiyama T, Miyoshi Y, et al. (2018) Association between tooth loss and cognitive impairment in community-dwelling older Japanese adults: A 4-year prospective cohort study from the Ohasama study. BMC Oral Health 18(1): 1-8.
- Yoo JJ, Yoon JH, Kang MJ, Kim M, Oh N (2019) The effect of missing teeth on dementia in older people: a nationwide population-based cohort study in South Korea. BMC Oral health. 19(1): 61.
- Yoo JJ, Kim DW, Kim MY, Kim YT, Yoon JH (2019) The effect of diabetes on tooth loss caused by periodontal disease: A nationwide population‐based cohort study in South Korea. J Periodontol 90(6): 576-583.
- Kato H, Takahashi Y, Iseki C, Igari R, Sato H, et al. (2019) Tooth loss-associated cognitive impairment in the elderly: A community-based study in Japan. Intern Med 58(10): 1411-1416.
- Thomson WM, Broadbent JM, Caspi A, Poulton R, Moffitt TE (2019) Childhood IQ predicts age‐38 oral disease experience and service‐use. Community Dent Oral Epidemiol 47(3): 252-258.
- Li X, Kolltveit KM, Tronstad L, Olsen I (2000) Systemic diseases caused by oral infection. Clin Microbiol Rev 13(4): 547-558.
- Baiju RM, Peter EL, Varghese NO, Sivaram R (2017) Oral health and quality of life: Current concepts. J Clin Diagn Res 11(6): ZE21-ZE26.
- Harada CN, Love MCN, Triebel KT (2013) Normal cognitive aging. Clin Geriatr Med 29(4): 737-752.
- Leritz EC, McGlinchey RE, Kellison I, Rudolph JL, Milberg WP (2011) cardiovascular disease risk factors and cognition in the elderly. Curr Cardiovasc Risk Rep 5(5): 407-412.
- Visser A, Meijer HJ, Raghoebar GM, Vissink A (2006) Implant-retained mandibular overdentures versus conventional dentures: 10 years of care and aftercare. Int J Prosthodont 19(3): 271-278.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Pathology and Toxicology Research
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)



