Research Article
Factors Related to Nutritional Status Among Preoperative Abdominal Patients in Dak Lak, Vietnam.
1387
Views & Citations387
Likes & Shares
Nutrition is very important and necessary for every person. For those who undergoing surgery, nutrition plays an important role extremely.
Objectives: This study was conducted to describe the nutritional status before surgery and find out the relationship between demographic factors, subclinical indicators with the preoperative nutritional status among patients had scheduled abdominal surgery. They were being treated at the Department of General Surgery, Tay Nguyen Regional General Hospital in 2019.
Research subjects and methods: A cross-sectional descriptive study was performed among patients who hospitalized for treatment and indicated for abdominal surgery at the Department of General Surgery - Tay Nguyen Regional General Hospital.
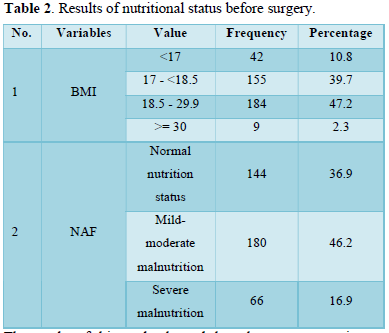
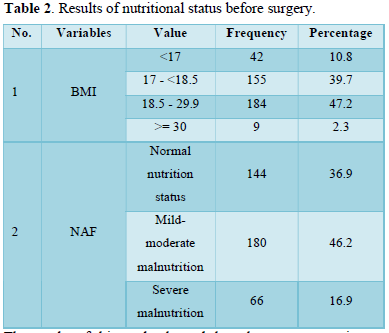
Results: According to Body Mass Index (BMI), 10.8% of patients had severe malnutrition; 39.7% have mild malnutrition; 47.2% of patients in normal nutritional status; 2.3% patients overweight. According to Nutrition Alert Form (NAF), 36.9% of patients had normal nutritional status; 46.2% have mild to moderate malnutrition; 16.9% severe malnutrition.
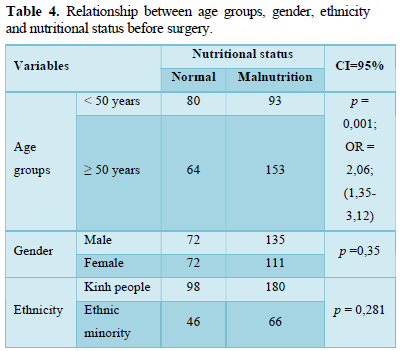
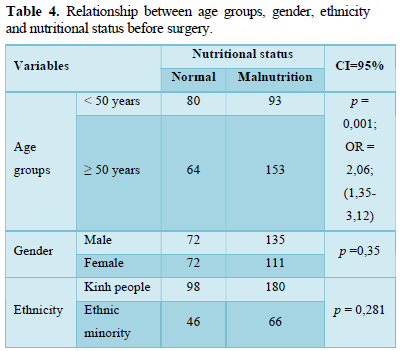
There was a difference in nutritional status between two groups: the proportion of participants over 50 years of age at risk of malnutrition was higher than 2.06 times of participants under 50 years old, statistically significant with p = 0.001.
Preoperative malnutrition was associated to age groups (p = 0.001); decreased of Albumin in blood (p < 0.01; OR= 2.32 (1.49-3.61); decreased of Hb in blood (p < 0.001; OR = 5.98; CI 95%: 3.63-9.86).
Keywords: Nutrition, Abdominal surgery, Related factors, Preoperative
Abbreviations: BMI: Body Mass Index; NAF: Nutrition Alert Form; Alb: Albumin; Hb: Hemoglobin; OR: Odds Ratio; CI: Confidence Interval
INTRODUCTION
According to the anatomical structure of the human body, the digestive tract is composed of specialized parts capable of digesting food, and breaking down food into nutrients, which can be absorbed into the body to provide energy [1]. When these organs had problem, the functions of the digestive tract are reduced, not achieving the normal digestive function as physiologically. Specifically, patients may present with a variety of discomfort symptoms, such as abdominal pain, loss of appetite, nausea/vomiting, heart burn, indigestion, constipation, diarrhea, etc. [2]. The above symptoms repeated continuously are the cause of hindering the ability to eat and absorb nutrients, causing the patient to fall into a state of undernutrition. As the consequence, the patients had risk of malnutrition naturally. Surgery is a solution for patients in order to get rid of the weakened digestive system and preserve health [3]. Malnutrition is one of the factors that increase surgical complications such as: surgical site infection, anastomosis, delayed wound healing, etc. Besides, malnutrition is also associated with other complications such as: pneumonia, sepsis. These complications are the cause prolonged hospital stay, increased treatment costs, and mortality [4,5]. It proves that the assessment and intervention of nutritional status among preoperative abdominal patients is still an urgent issue to be solved. In Vietnam, there are many studies on nutrition assessment. However, most of the research focused on nutrition in the community, especially nutrition in children. In recent years, a number of studies in central hospitals have shown a high rate of malnutrition among surgical patients, especially gastrointestinal tract surgery [6,7]. Currently, there are no studies in Dak Lak province on nutritional status among surgical patients. Therefore, this study was conducted to evaluate the nutritional status in group of patients who had scheduled gastrointestinal surgery at Tay Nguyen Regional General Hospital. From there, researchers provide the appropriate intervention strategies in order to reduce the proportion of malnutrition before surgery. It will contribute to shortening hospital stay and reducing treatment costs for patients as well.
RESEARCH METHODOLOGY
Objectives
- To describe nutrition status among preoperative abdominal patients at the Department of General Surgery, Tay Nguyen Regional General Hospital, Vietnam
- To examine the relationship between demographic factors, paraclinical indicators with the preoperative nutritional status among patients who had scheduled abdominal surgery in Tay Nguyen Regional General Hospital,
Design and setting
A cross-sectional descriptive research design was employed for this study. Data collection was performed at the Tay Nguyen Regional General Hospital, Vietnam, from May to September, 2019.
Sample:
Sample size was calculated following the formula:
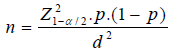
In there:
n: Sample size
Z: With significance level α = 5%, then Z (1-α/2) = 1.96.
p: Based on the previous published data, we chosen p = 0.5
d: confidence interval of true value of sensitivity, using d = 0.05.
In this study, 10% of patients were added to reduce the risk patient withdraw out of the research. So that, a sample of 390 patients who were waiting for major elective abdominal surgery was recruited using simple random sampling technique.
Inclusion criteria were: (1) 18 years of age or older; (2) agree to participate in the study; (3) hospitalized for treatment within 48 hours and indicated for elective surgery.
Exclusion criteria were: (1) undergone surgery at the local health; (2) inability to answer interviews such as mental disorders, dementia, mute, deaf.
Data were collected through a structured questionnaire, consisting of two parts: (1) General information; (2) Assessment of nutritional status before surgery: BMI, NAF, clinical characteristics, paraclinical indexes. The researchers conducted direct interviews with the participants; combined with the observation and measuring anthropometric parameters, other body indicators. The collected information was carefully remarked on the survey form which avoid confusion or missing. Other information was gathered from the medical record which were completed after the patients interviewing.
Data analysis
Data were analyzed using the Student Version of Statistical Package for Social Sciences (SPSS) version 17.0. The alpha level for significance was set at .05. Categorical variables were presented by frequency and percentages, and continuous variables by mean and standard deviation. The Chi-square (Fisher’s exact tests where necessary) were used to analyze the relationship between demographic factors, subclinical indicators with the preoperative nutritional status.
Ethical considerations
Prior to data collection, the study protocol was approved by the Research Review Board, Faculty of Medicine and Pharmacy, Tay Nguyen University, and permission to collect data was obtained from the Director of Dak Lak General Hospital. Patients were clearly informed about the study’s aims, benefits, data collection procedure, and of their rights. All data was stored in a secure place and utilized only for this study.
RESULTS AND DISCUSSION
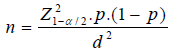
The results showed that the average age of the participants was 53.19 ± 18.29 years. After divide into subgroups, the group under the age of 50 years accounted for 44.36%, the group over the age of 50 was 55.64%. Kinh people is the majority ethnic group (71.3%). The proportion of male (53.1%) was higher than female (46.9%), but not significantly. Education level was differentiated from low to high, most of them have high school level (30.3%). Perhaps, that is also the reason why most of the participants were farmer (55.4%).
General characteristics of research subjects (Table 1).
According to BMI, 10.8% of patients had severe malnutrition (BMI <17); 39.7% had mild malnutrition (BMI from 17 - <18.5). There were 47.2% of patients in normal nutritional status, and 2.3% patients in overweight. As we known, BMI is the instrument so simple and easy which can assess the nutritional status. BMI less than 17 is considered severe malnutrition, high risk of death. The research result of Nguyen Thuy An (2010), only 25.8% of the patients were malnourished (BMI below 18.5) [8]. The study of Luu Ngan Tam and colleagues was performed at Cho Ray hospital in 2009 accounted for 24.5% of the total 710 patients with malnutrition (BMI below 18.5) [9]. This could be due to many reasons, in which, the average age of the participants was a little bit high (Mean= 53.19). The body had begun the changes in digestive function such as taste changes, decreased gastric secretion due to physiological changes. At the same time, the impact of pathological disorders, such as vomiting, diarrhea, abdominal pain led to unintentional weight loss for a long time, resulting in a marked change in BMI. On the other hands, 390 patients were assessed by NAF, the results showed that 144 (36.9%) patients were classified as normal nutritional status, 180 (46.2%) patients were classified as mild to moderate malnutrition, 66 (16.9%) patients were classified as severely malnourished. Thus, the proportion of patients with malnutrition in this study was 63.1% which higher than other research results, such as Dang Tran Khiem (2011) at Cho Ray hospital (53.1%) [6]; Doan Duy Tan in 2016 (55.2%) [7]. The study results also showed that, the proportion of malnutrition assessed by NAF which higher than by BMI. It seems to be that the assessment of nutritional status by only BMI can sometimes be limited, because it ignores other characteristics affecting nutritional status.
Characteristics of the preoperative nutritional status of the participants (n=390) (Table 2).
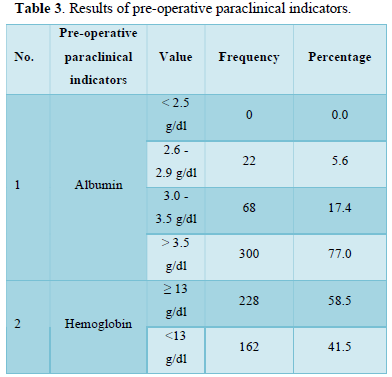
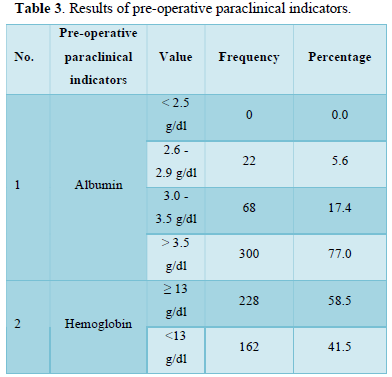
The results of this study showed that, there was no patient with severe hypoalbuminemia (< 2.5g/dl). There was 23% of patients who had decreased of Albumin in blood (≤ 3.5 g/dl). Most of the patients had Albumin in blood index within the normal range (>3.5 g/dl), accounted for 77% patients. If the concentration of Albumin in blood decreases, the risk of postoperative complications and death increases. Our study showed a higher result than Nguyen Thuy An’s study (2010) by 18.3% [8] but lower than the research result of Nguyen Thi Van Anh at Bach Mai hospital [10] in 2010 was 32.3% patients with Albumin in blood index <35g/l. Investigation the Hemoglobin (Hb) in blood index, the results showed that: 41.5% participants had Hb in blood index < 13g/dl and 58.5% of the patients had a blood Hb index ≥ 13g/dl. Thus, the proportion of patients had Hb in blood index in the normal range still prevails. Compare with the research results of Duong Thi Phuong [11], the proportion of patients with anemia (Hb in blood <13g/dl) was 59.2% [11]. According to the study results of Trinh Hong Son [12], the proportion of patients with low Hb/ blood index was 70% [12]. In summary, when taking care of patients, the health care professional should be focusing on adding nutritious, high-energy foods. It is also necessary to pay attention to iron-rich food groups which help stimulate the proliferation of red blood cells, and other blood cells.
Characteristics of the pre-operative paraclinical indicators of the participants (n=390) (Table 3).
There was a difference in nutritional status between two groups of age, the proportion of participants over 50 years of age at risk of malnutrition was higher than 2.06 times of participants under 50 years old, statistically significant with p = 0.001. In which, the group of participants has a slightly high average age (Mean= 53.19; SD = 18.29). The age of participants in this study is higher than the experimental group of Dang Tran Khiem [6], which is 49.6 ± 15.7. However, the research results are similar to the result of Nguyen Thuy An in 2011 with the mean age of the study population was 53.70 ± 18.06 [8]. In fact, age is a factor that could not change, the clinical impact of age in each person occurs naturally. We have recorded that the more older patients, the more their body has problems with changing in digestive function such as reducing the taste, decreasing secretion of gastric juice, etc due to physiological reasons. At the same time, the impact of pathological disorders such as vomiting, diarrhea, abdominal pain, etc. leads to a higher risk of malnutrition. The results of this study are similar with other research, including Doan Duy Tan’s study in 2016 (p < 0.001; OR = 2.89, CI: 95%:1.75-4.78) [7]; study of Lee et al. in 2013 (p < 0.00; OR = 1,043 CI: 95%: 1,027-1,058) [13]. Therefore, we should regularly pay attention into evaluation and managing the nutritional status among elderly subjects. The results also showed that there was no statistically significant difference in gender with the nutritional status of patients. The previous research result of Burgos [14] also have the same opinion on this issue. However, study of Duong Thi Phuong [11] reported that the difference in sex related to the nutritional status of patients, statistically significant with p = 0.025. Research results of Álvarez-Hernández [4], Kruizenga [15] also confirmed that gender is related to the nutritional status of patients.
The relationship between demographic, subclinical factors and nutritional status before surgery (Table 4).
There was no difference in nutritional status between Kinh people and minority ethnic groups (p > 0.05). Dak Lak province includes many ethnic groups, in there, characteristics of the sample are mainly Kinh people, then Ede people and other ethnic groups such as Bana, J’rai, Tay, and Mnong. With the particularity of economic difficulties, the conditions for receiving medical and health care knowledge of minority ethnic groups are often less than Kinh people. They were encounter the barriers in culture, languages, beliefs and the faith with health care services in community. Thus, this research results are also a good sign that the health status of the minority ethnic groups is getting more attention and improve in particularly. Regarding the paraclinical indexes, malnutrition was related to the level of Albumin in blood reduction (p<0.01; OR=2.32(1.49-3.61)). This result is similar to the research results of Duong Thi Phuong [11] in 2017 (p= 0.003). In addition, research results of Lee in 2013 [13] had the consensus (OR = 0.994, 0.267- 0.737; p < 0.01). Study of Nguyen Thuy An in 2010 [8] also confirmed that although the mean of Albumin in serum value was within the normal range, the authors noted there was decreased of Albumin in serum among the group of patients with severely impaired nutritional status (p<0.001). As the consequence, the Alb in blood test is one of the appropriate tests in order to assess the patient's overall nutritional status. Therefore, in the recent years, testing level of Albumin in blood is a routine preoperative test. After that, patients shall receive nutritional support before surgery if the test result was less than 3.0 g/dl. Results of this study showed that the number of patients whose Hemoglobin in blood value was within normal range accounted for a large number. However, the reduction of Hb in blood was related to the patient's nutritional status (p <0.001; OR = 5.98; 95% CI: 3.63-9.86). The results of other studies also confirm this opinion such as: study of Doan Duy Tan in 2016 (p<0.001; OR = 2.77 (1.68- 4.58)) [7]; study of Duong Thi Phuong et al. in 2017 (p= 0.01) [11]. In contrast, study of Lee in 2013 [13] reported that there was no association between malnutrition and the decreased of Hemoglobin in the blood (p > 0.05) (Table 5).
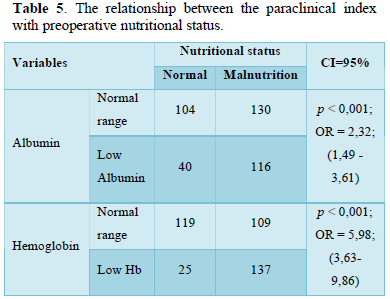
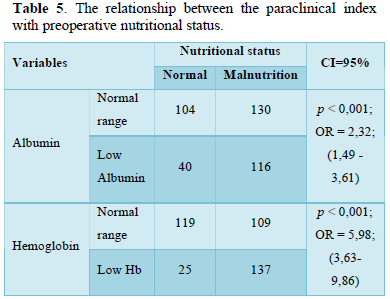
As we known, the patients had diseases related to the digestive tract directly, so the ability to eating the food as well as absorb nutrients less leads to reducing Hemoglobin in blood index. In this study, there was an interesting thing that the number of patients with Hemoglobin in blood index within the normal range accounted for a large number. Perhaps, because the patient’s population were excluded malignancies of the gastrointestinal tract, so the number of patients with anemia accounted for low percentage. Thus, when health care providers take care the patients, it is very necessary to ensure supporting nutrition before surgery. Also, doctors should be providing the proper nutrition to restore patients’ health until post-surgery period. Moreover, as mentioned above, they should pay attention to iron rich foods that stimulate the proliferation of red blood cells and other blood cells.
CONCLUSIONS
Nutritional status before surgery of participants
According to Body Mass Index (BMI), 10.8% of patients had severe malnutrition; 39.7% have mild malnutrition; 47.2% of patients in normal nutritional status; 2.3% patients overweight.
According to Nutrition Alert Form (NAF), 36.9% of patients had normal nutritional status; 46.2% have mild to moderate malnutrition; 16.9% severe malnutrition.
Factors related to nutritional status among preoperative abdominal patients
There was a difference in nutritional status between two groups: the proportion of participants over 50 years of age at risk of malnutrition was higher than 2.06 times of participants under 50 years old, statistically significant with p = 0.001, OR = 2.06; 95% CI:1.35-3.12.
Preoperative malnutrition was significantly associated with decreased of Albumin in blood (p < 0.01; OR= 2.32 (1.49-3.61). In addition, there was a significant association between preoperative malnutrition with decreased of Hb in blood (p < 0.001; OR = 5.98; CI 95%: 3.63-9.86).
RECOMMENDATIONS
- For patients undergoing gastrointestinal surgery, the medical staffs should be pay more attention to preoperative nutritional status, especially elderly patients with changes in paraclinical index (Hb in blood index; Alb in blood index). From there, they can detect early poor nutritional status as well as design a nutritional support plan in preoperative period. As a consequence, these patients can avoid postoperative complications, reducing the treatment costs and hospitalization.
- Coordinating between the clinicians and the nutritionist in monitoring the nutritional status and treatment among this group of patients.
- Combining the investigation of the dietary intake for each specific patient as well as the assessment of micronutrient deficiencies in order to provide a proper nutrition.
- Propagate health education, improve patients' knowledge about the role of nutrition in treatment to coordinate adherence and improve treatment effectiveness.
- Pellico LH (2013) Focus on adult health: Medical- Surgical nursing (1st). Philadelphia: Lippincott Williams & Wilkins.
- Hall M, Frances DC, Williams S, Golosinskiy A, Schwartzman (2010) 2007 National hospital discharge survey. Natl Health Stat Report 29: 1-21
- Cerantola Y, Grass F, Cristaudi A, Demartines N, Schäfer M, et al. (2011) Perioperative Nutrition in Abdominal Surgery: Recommendations and Reality. Available online at: http://dx.doi.org/10.1155/2011/739347
- Álvarez HJ, Planas VM, León SM, García de LA, Celaya PS, et al. (2012) Prevalence and costs of malnutrition in hospitalized patients: The PREDyCES Study. Nutr Hosp 27(4): 1049-1059.
- Leiva BE, Badia TM, Virgili CN, Elguezabal SG, Faz MC, et al. (2017) Hospital malnutrition screening at admission: Malnutrition increases mortality and length of stay. Nutr Hosp 34: 907-913.
- Dang TK, Luu NT, Nguyen TC (2013) Perioperative nutritional status and early outcomes of patients at department of hepatobiliary and pancreatic surgery at Cho Ray hospital. Ho Chi Minh City Med J 17(1): 328-334.
- Doan DT (2016) Nutritional status before surgery and related factors with patients of gastroenterology department at Nguyen Tri Phuong hospital in 2016. Master's thesis of nursing: University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City.
- Nguyen TA (2010) Nutritional status and infectious complications after surgery of hepatobiliary and pancreatic disease. Master's thesis of nursing: University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City.
- Luu NT, Nguyen TQH (2009) Nutritional status of patients at the time of admission at Cho Ray hospital. Ho Chi Minh City Med J 13(1).
- Nguyen TVA (2010) Nutritional status of chronic renal failure patients undergoing dialysis and related factors at the artificial kidney department of Bach Mai hospital. Bachelor's thesis of Public Health: Hanoi Medical University, Hanoi.
- Duong TP, Le TH, Nguyen TL, Duong TY (2017) Nutritional status of cancer patients at Hanoi Medical University hospital. J Med Res 106(1): 163-169.
- Trinh HS, Nguyen BA, Le MH, Nguyen TL (2013) Assessment of nutritional status of patients before gastric cancer surgery. J Pra Med 884: 3-7.
- Lee HK, Choi HS, Son EJ, Lyu ES (2013) Analysis of the Prevalence and Risk Factors of Malnutrition among Hospitalized Patients in Busan. Prev Nutr Food Sci 18(2): 117-123.
- Burgos R, Sarto B, Elío I, Planas M, Forga M, et al. (2012) Prevalence of malnutrition and its etiological factors in hospitals. Nutr Hosp 27(2): 469-476.
- Kruizenga H, Keeken S, Weijs P, Bastiaanse L, Beijer S, et al. (2016) 2 Undernutrition screening survey in 564,063 patients: patients with a positive undernutrition screening score stay in hospital 1.4 d longer. Am J Clin Nut 103: 1026-1032.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Pathology and Toxicology Research
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)

