Research Article
A Study on Correlation Between Menstrual Cycle Irregularities and BMI Among Residential Female Students of Mawlana Bhashani Science and Technology University, Santosh, Tangail
1807
Views & Citations807
Likes & Shares
The study was conducted to evaluate the correlation between menstrual cycle irregularities and Body Mass Index (BMI) among residential female students of Mawlana Bhashani Science and Technology University, Santosh, Tangail. This study was at university female halls, different female hostels and different faculty of the university using a validated questionnaire which was developed for this study. A total 250 female students, at the age of (18-26) years were participated. Collected information was analyzed using SPSS version 20.0 and MS Excel 2007, out of the 250 respondents, 72.4% had regular menstrual cycles and 27.6% had abnormal and irregular cycles. According to the BMI categorization, underweight is 62 (24.8%), normal is 147 (58.8%), overweight is 32 (12.8%) and obese reported in 9 (3.6%) respondents. Among the students, 24% respondents had reported in menorrhagia, 12% polymenorrhea, 37.2% oligomenorrhea, 14% hypomenorrhea, 77.2% had dysmenorrhea and 72% had premenstrual syndrome. Irregular menstrual cycle, were found in underweight (10.4%) and overweight students. About (8.4%) were underweight and they faced their menstrual cycle once in three months. 3.6%, 7.6% and 0.8% were underweight, normal and overweight respectively and they had polymenorrhea. 9.6%, 18.4%, 6.8% and 2.4% were underweight, normal, overweight and obese respectively and they had oligomenorrhea. 2%, 3.6% and 0 .4% respondents were underweight, normal, overweight and respectively and they had hypomenorrhea. 3.2%, 7.6%, 2% and 0.4% respondents were underweight, normal, overweight and respectively and the duration of menstrual flow of them were greater than 7 days. This study shows a strong positive correlation between BMI and menstrual profile as menstrual cycle (r=0.651), menstrual cycle irregularities (r=0.820) and premenstrual syndrome (r=0.646). There was weak positive correlation between BMI and menstrual profile as cycle length (r=0.044), duration of menstrual flow (r=0.434), amount of menstrual flow (r=0.185) and dysmenorrhea (r=0.106).
Keywords: Body Mass Index (BMI), Menstrual cycle irregularities, Premenstrual Syndrome (PMS)
INTRODUCTION
Menstruation is a woman’s monthly bleeding caused by the reduction of hormones, estrogen and progesterone at the end of the monthly ovarian cycle [1,2]. When menstruation occurs repeatedly, it is called the menstrual cycle [3]. The menstrual cycle is important as female reproductive function which prepares the female body for conception and pregnancy [2,3]. In recent years, there is an escalation of menstrual disorders in both developing and developed countries. However, the exact prevalence or incidence of menstrual dysfunction is still very scarce [1]. Example of menstrual disorders are amenorrhea, which is lack of menstrual period, dysmenorrheal (painful periods), irregular cycles, heavy and excessive bleeding called menorrhagia [1,3-5].
Factors that often play a role in the regularity and flow of a woman's menstrual cycle include hormonal changes, genetics, serious medical conditions and body mass index (BMI). Of all these factors, BMI had the most control over menstrual irregularity. Having a high or low BMI may cause to experience an absence of menstruation, irregular menstruation and painful menstruation [6,7]. Menstrual cycle irregularities and an ovulation have been found to occur with increased frequency in women who deviate considerably from normal weight.
Obesity is becoming a growing public health issue and is one of the leading causes of morbidity and mortality in many diseases. Obesity also increases the risk for developing gynecological diseases including infertility and menstrual dysfunction [8], although a variety of sex hormones also play an important role in these disorders. The gynecological diseases include a wide range of abnormalities including the length of menstrual cycle, length of menses, irregular menstrual cycle and menstrual blood loss. It was reported that obese women had more irregular and longer menstrual cycle [9-15]. There is growing evidences also suggesting that menstrual cycle dysfunction in women is linked to breast cancer, endometrial cancer, cardiovascular disease and neurologic disorders [16-18]. The risk of developing endometrial hyperplasia is significantly increased in overweight women.
A number of studies have shown that higher obesity grades were associated with higher probabilities of irregular pattern of menstrual cycles [19,20]. The increasing trends in the prevalence of childhood obesity, early puberty and menarche, and ethno racial differences in the effect of BMI on the reproductive characteristics of young females around the world, warrant continuous evaluation.
Disorders in menstrual cycle have multiple etiologies and studies of associated variables have found relationships with body mass index (BMI). Regulation of reproduction affected by body fat, an extreme body mass undesirably affects reproduction, starting from pubertal development, menstrual function and fertility [12,21,22]. Body mass index influenced the age at menarche, duration and regularity of menstrual cycle and significantly associated with the menstrual problem as dysmenorrhea, hypomenorrhea, oligomenorrhea, amenorrhea and premenstrual syndrome [23]. Menorrhagia denotes regular cycles with bleeding either excessive in amount (>80ml) &/or, in duration with flow lasting >7 days. Hypomenorrhea is scanty menstrual flow which lasts for 35 days.
Therefore, this study was conducted to assess the body mass index and menstrual disorders among the residential students of Mawlana Bhashani Science and Technology University. Also shows a correlation between BMI and irregularities of menstrual cycle.
MATERIALS AND METHODS
Study design
A cross-sectional study which assesses the menstrual disorders of residential students of Mawlana Bhashani Science and Technology University. In this study data were collected among 250 individuals from residential students to assess their menstrual abnormalities. The ranges of age of all participants were 20-25 years. The data had been collected by face-to-face interview.
Questionnaire Formation
A self-administered questionnaire prepared by the author. The questionnaire consisted of previously validated menstrual disorders knowledge-based published surveys.
Statistical analysis
Data were analyzed using Statistical Packages for Social Sciences (IBM SPSS version 20.) software. The correlation between menstrual disorders and BMI were assessed by ‘r’ test. The prevalence of menstrual disorders was counted by frequency. Graphical representation of the results was done with Microsoft Excel programme 2007 and SPSS.
RESULTS
A total 250 students completed the questionnaire. The age, BMI, qualification of study, marital status, menarche age, menstrual cycle, cycle length, duration of menstruation, menstrual flow, PMS, painful menstruation, treatment for menstruation abnormalities, any other major diseases, exercise, meal and hygiene management of individual were recorded.
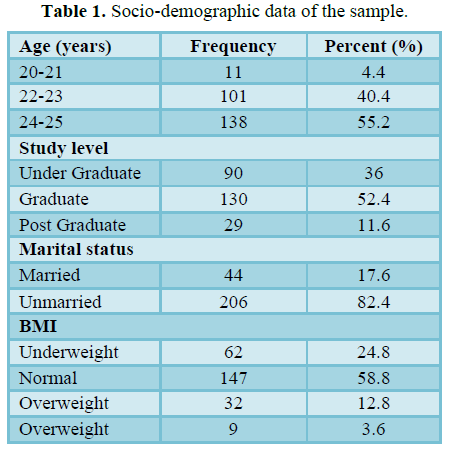
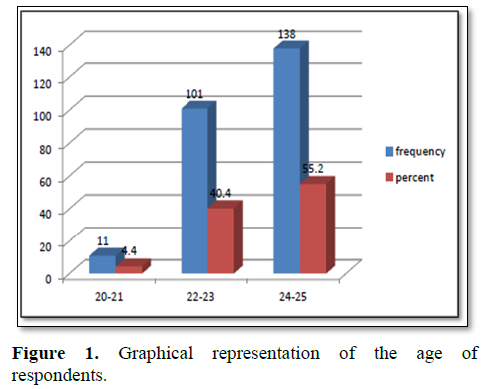
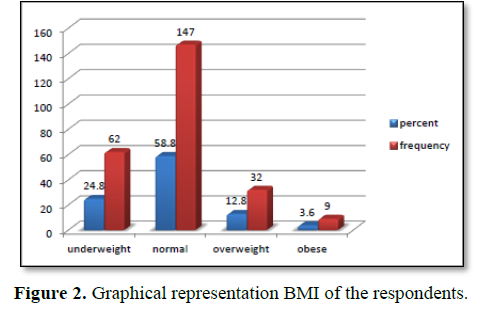
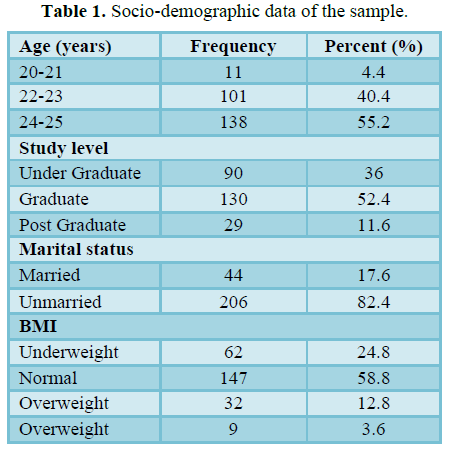
Table 1 represents socio-demographic characteristics of respondents. It shows that, the mean age of the participants was 23.48 years (SD 1.038) with range 20-25 years. Among 250 students, 36% were undergraduate, 52.4% were graduate and 11.6% were postgraduate. It was also observed that, 17.6% were married and 82.4% were unmarried. According to the BMI categorization, 24.8% of the respondents were underweight, 58.8% were normal, 12.8% were overweight and 3.6% were obese (Figures 1 and 2).
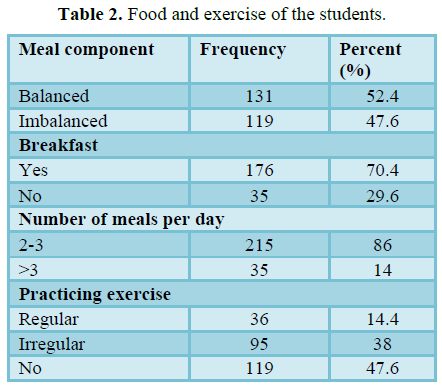
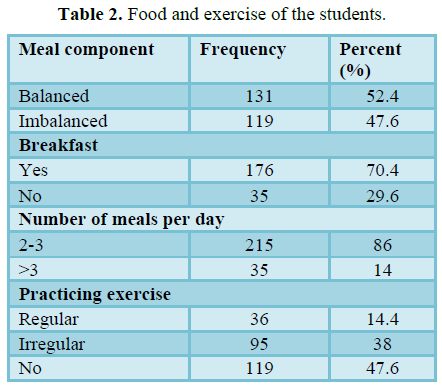
Table 2 represents some life style habits of the students. Out of the 250 respondents, the meals components (52.4%) respondents were balanced and 47.6% respondents were balanced. 70.4% respondents had breakfast and 29.6% are not. 86% student have meal 2- 3 times per day and 14% have >3 times per day. It was also observed that 14.4% student practicing exercise regularly, 38% students were irregular and most of the students (47.6%) were not.
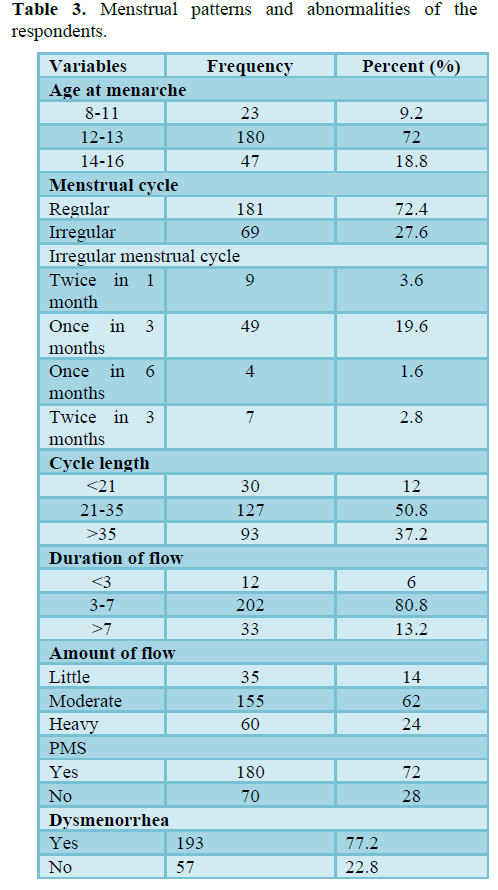
Table 3 represents that, the mean age of the menarche of the respondent was 12.73 (SD 1.140). Out of the 250 respondents, 72.4% have regular menstrual cycles and 27.6% have abnormal and irregular cycles. Moderate blood flow was reported by 62% of respondents, 24% had heavy
blood flow and 14% had scanty or little blood flow. The length of the menstrual cycle of the 127 respondents (50.8%) were 21-35, of the 93 respondents (37.2%) were greater than 35 and of the 30 respondents (12%) were less than 21. Most of them reported their menstruation duration range between 4-7 days (80.8%), 13.2% were greater than 7 and 6% were less than 3. 77.2% dysmenorrhea (painful menstruation) and 72% premenstrual syndrome were reported by the respondents. Figure 3 shows that 72.40% had regular menstrual cycle and 27.60% had irregular menstrual cycle.
Figure 4 shows that, 3.6% respondents faced their menstrual cycle twice in one month. Once in three months were reported in 19.6% respondents, once in six months were in 1.6% and twice in three months were reported in 2.8% respondents out of the 69 respondents (27.6%).
Figure 5 shows the menstrual disorders experienced by the study population. Dysmenorrhea reported in 193 (77.2%), premenstrual syndrome reported in 180 (72%), heavy menstrual flow reported in 60 (24%), hypomenorrhea reported in 15 (14%), polymenorrhea reported in 30 (12%) and oligomenorhea reported in (37.2%) of the respondents.
Figure 6 shows that 8% respondents whose menstrual cycle were regular and 4% respondents whose menstrual cycle were irregular and menstrual length of them were less than 21 days. Most of the respondents (48.8%) whose menstrual cycle were regular and only 2% of the respondents whose menstrual cycle were irregular and menstrual length of them were normal range (21-35 days). that 15.6% respondents whose menstrual cycle were regular and 21.6% respondents whose menstrual cycle were irregular and menstrual length of them were less than 21 days.
Figure 7 shows that 1.2%, 3.2% and 0.8% respondents had regular menstrual cycle and duration of menstruation were less than 3 and amount of flow of menstruation were little, moderate and heavy respectively. 0.8% respondents had irregular menstrual cycle and duration and amount of flow of
menstruation was less than 3 and moderate respectively.8.8%, 38.4% and 12.8% respondents had regular menstrual cycle and duration of menstruation were 3-7 and amount of flow of menstruation were little, moderate and heavy respectively. 2.8%, 12.8% and 5.2% respondents had irregular menstrual cycle and duration of menstruation were 3-7 and amount of flow of menstruation were little, moderate and heavy respectively. 0.4%, 6.4% and 0.4% respondents had regular menstrual cycle and duration of menstruation were greater than 7 and amount of flow of menstruation were little, moderate and heavy respectively. 0.8%, 0.4% and 4.8% respondents had irregular menstrual cycle and duration of menstruation were greater than 7 and amount of flow of menstruation was little, moderate and heavy respectively.
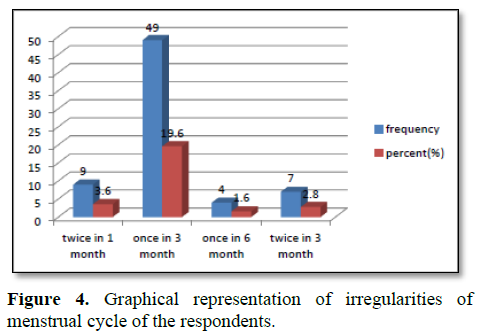
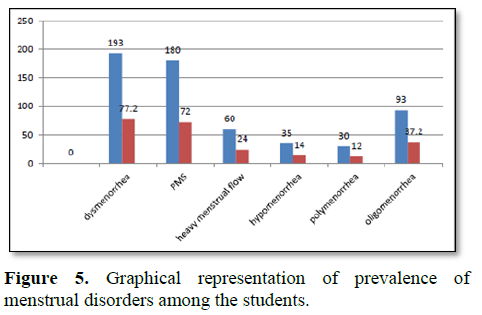
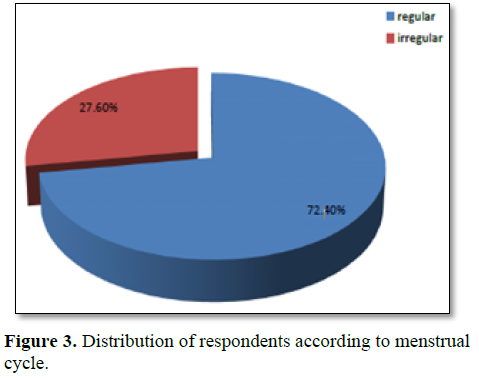
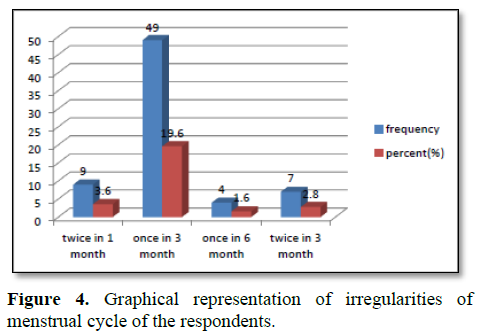
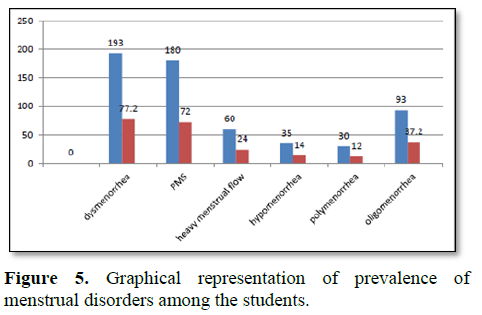
Table 4 represents PMS symptoms of the respondents. Out of the 180 students most of the students were experienced by joint or muscle pain (44%), breast tenderness (42.8) and abdominal bloating (42%). More than one symptom was reported in one respondent before the menstruation (Figure 8).
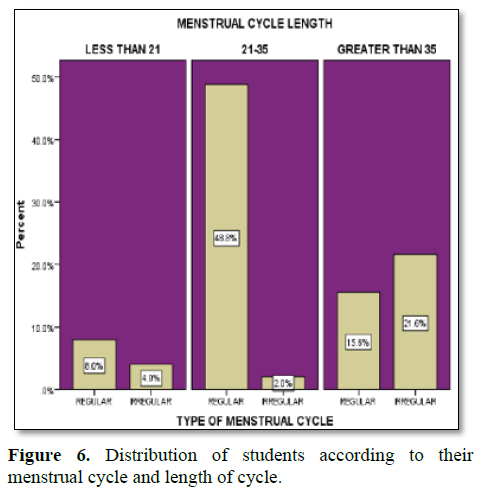
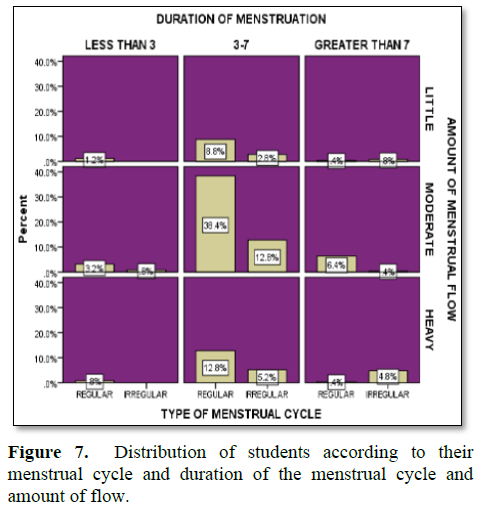
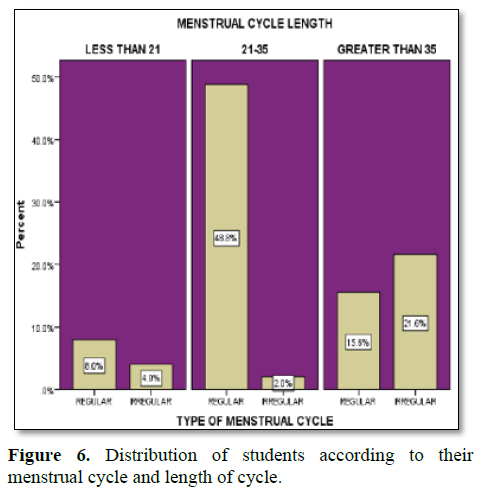
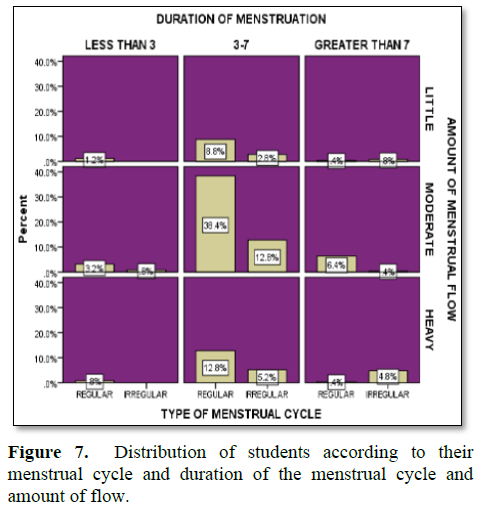
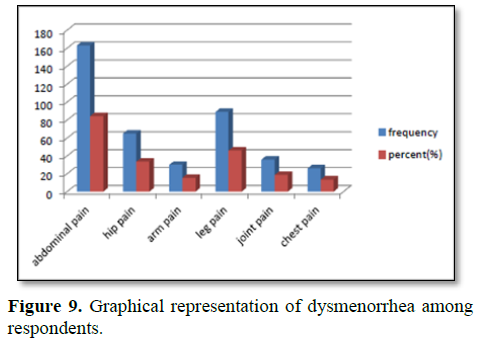
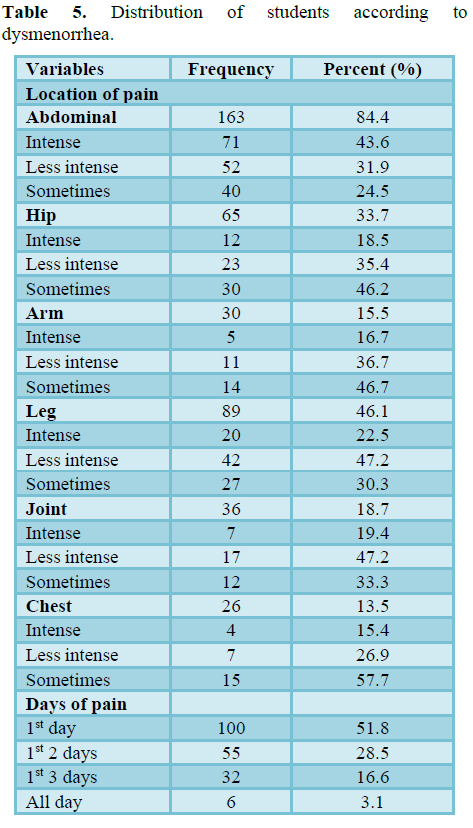
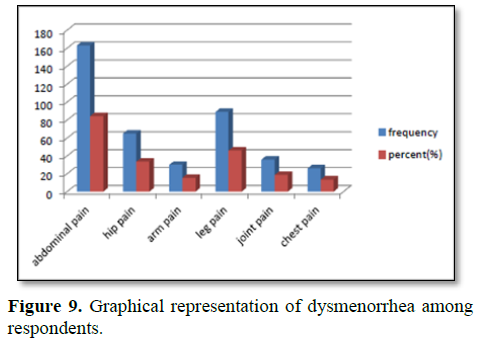
Table 5 represents dysmenorrhea of the students. Out of the 193 participants, most of the students were suffered from abdominal pain (84.4%). 33.7% hip pain, 15.5% arm pain, 46.1% leg pain, 18.7% join pain and chest pain 13.5% of the respondent were reported. One respondent was suffered from different pain and various intensity. Abdominal in pain were most intense among the students. The pain was lasting in various range 51.8% of the student’s 1st day, 28.5% 1st 2 days, 16.6% 1st 3 days and 3.1% all day suffered from pain (Figure 9).
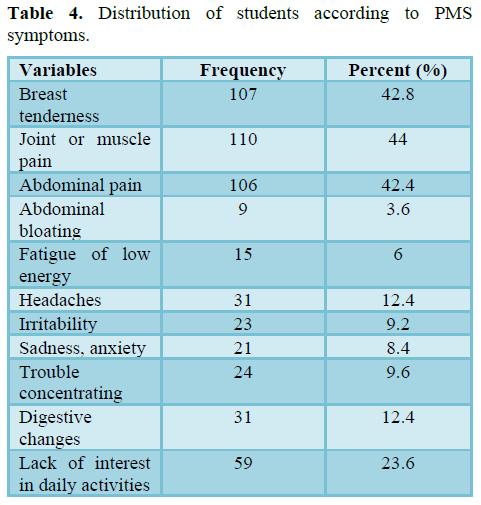
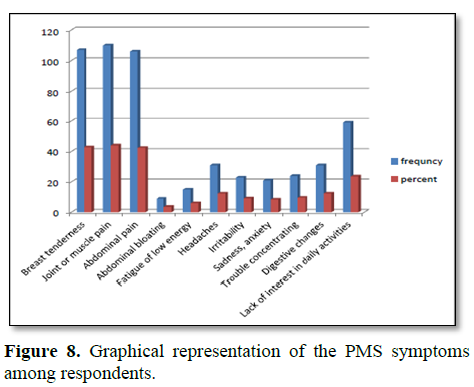
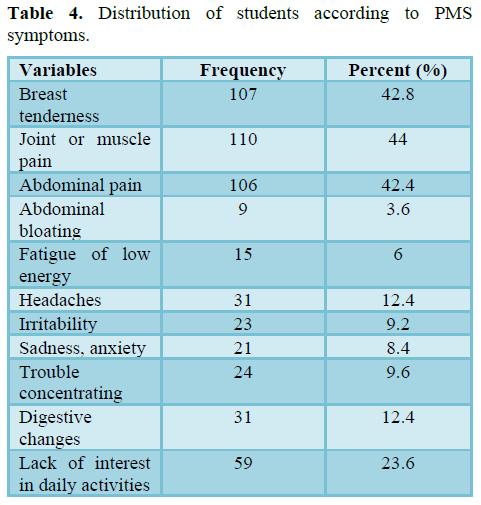
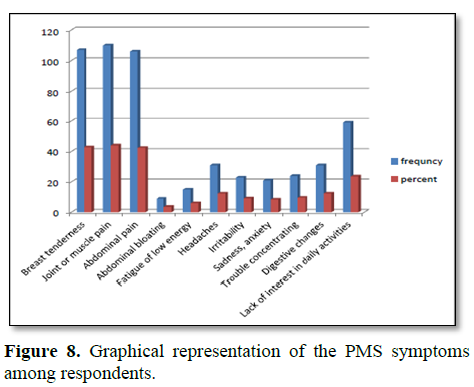
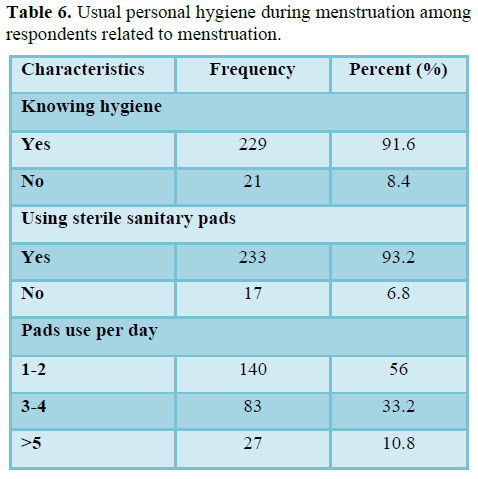
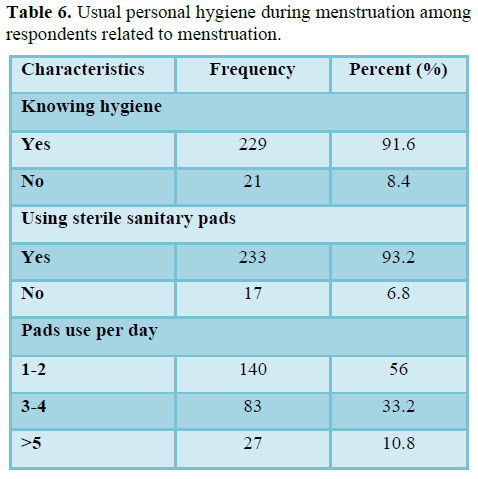
Table 6 shows that, out of 250 students, most of the student known about hygiene and 8.4% of the students don’t know about hygiene. 6.8% of the students did not use sterile sanitary pad during menstruation. Most of the students used 1-2 pads per day (56%), 33.2% used 3-4 pads and 10.8% used more than 5 pads per day.
Table 7 shows that there was positive correlation between BMI of students and their menstrual cycle (r = 0.651). 10.4% respondents were underweight, 8.8% respondents whose BMI were normal, 6.8% respondents were overweight, 1.6% respondents were obese and their menstrual cycle were irregular. 14.4% respondents are underweight. 50% respondents were normal, 6% were overweight, 2%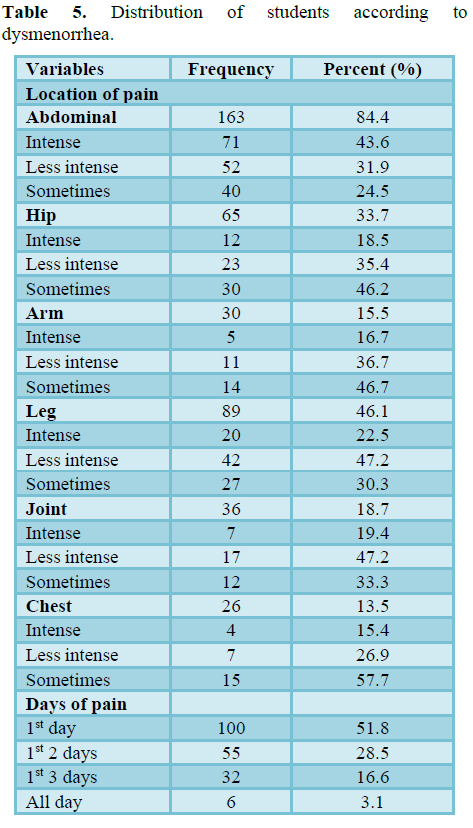
respondents were obese and their menstrual cycles were regular.
Table 8 shows that there was strong positive correlation of body mass index and menstrual cycle irregularities of students (r = 0.820). 1.6% respondents were underweight and normal BMI, 0.4% respondents were overweight and they faced their menstrual cycle twice in one month. Most of the respondents (8.4%) were underweight and they faced their menstrual cycle once in three months. 2% respondents were normal and they faced their menstrual cycle twice in three months.
Table 9 shows that there was very weak positive Correlation of body mass index and menstrual cycle length of students (r = 0.044). Most of the respondents (32.8%) whose BMI were normal and they faced their menstrual cycle 21-35. 3.6%, 7.6% and 0.8% were underweight, normal and overweight respectively and they had polymenorrhea. 9.6%, 18.4%, 6.8% and 2.4% were underweight, normal, overweight and obese respectively and they had oligomenorrhea.
Table 10 shows that there was positive correlation of body mass index and duration of menstrual flow of students (r = 0.434). 2%, 3.6% and 0 .4% respondents were underweight, normal, overweight and respectively and they had hypomenorrhea. 19.6%, 47,6%, 10.4% and 3.2% respondents were underweight, normal, overweight and respectively and they have normal duration of menstrual flow. 3.2%, 7.6%, 2% and 0.4% respondents were underweight, normal, overweight and respectively and the duration of menstrual flow of them were greater than 7.
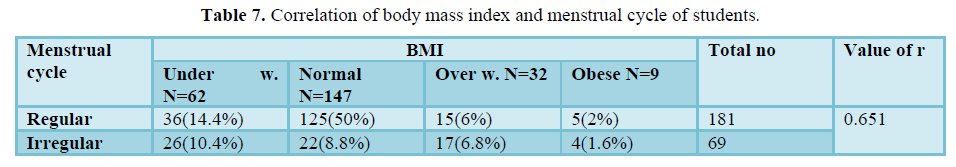
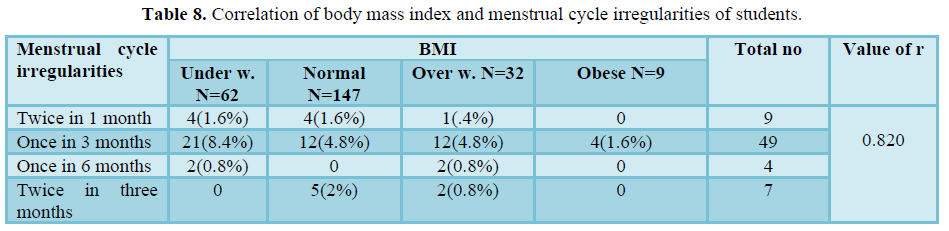
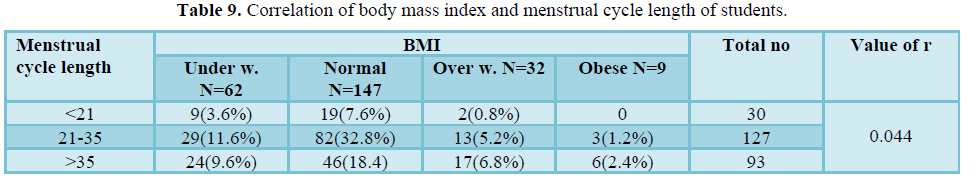
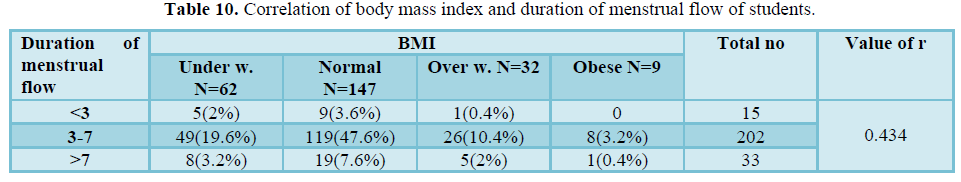 Table 11 shows that there was weak positive Correlation of body mass index and amount of menstrual flow of students (r = 0.185). Most of the respondents whose BMI were normal and they had moderate menstrual flow.
Table 11 shows that there was weak positive Correlation of body mass index and amount of menstrual flow of students (r = 0.185). Most of the respondents whose BMI were normal and they had moderate menstrual flow.
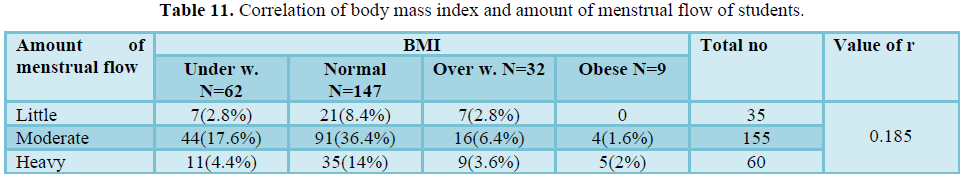
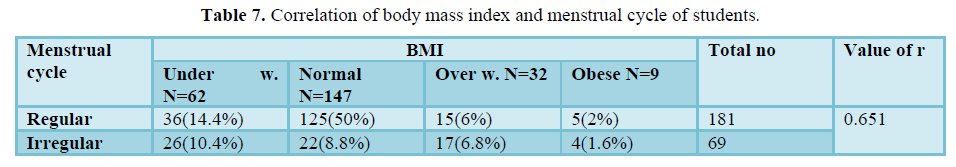
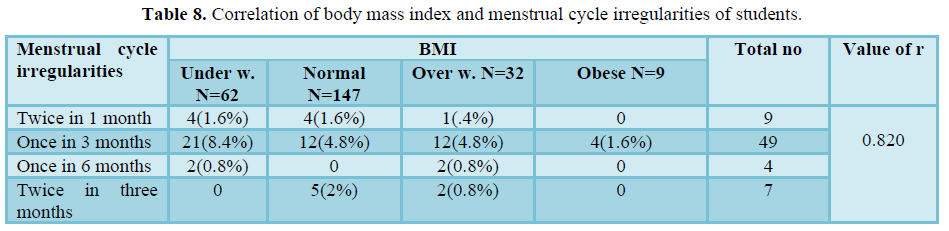
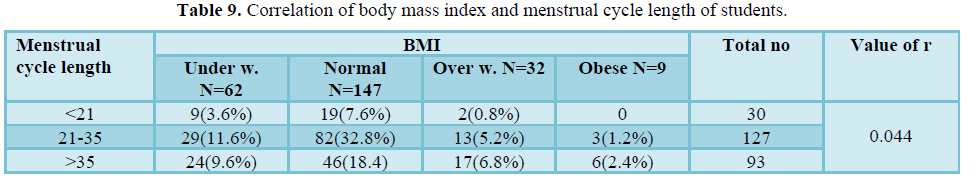
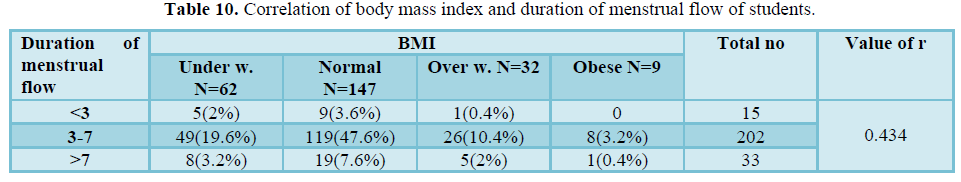 Table 11 shows that there was weak positive Correlation of body mass index and amount of menstrual flow of students (r = 0.185). Most of the respondents whose BMI were normal and they had moderate menstrual flow.
Table 11 shows that there was weak positive Correlation of body mass index and amount of menstrual flow of students (r = 0.185). Most of the respondents whose BMI were normal and they had moderate menstrual flow.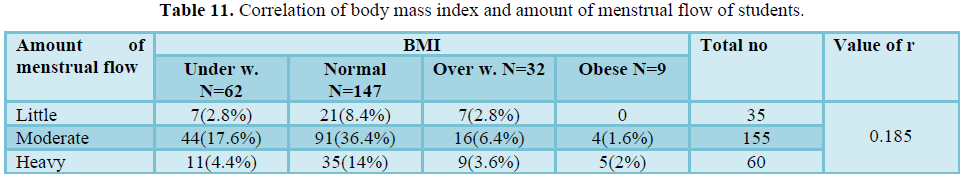
Table 12 shows that there was positive correlation of body mass index of students and their premenstrual syndrome (r = 0.646).
Most of the respondents who experienced PMS symptoms were normal (40.4%), underweight (19.6%), overweight (3.2%) and obese (3.2%).
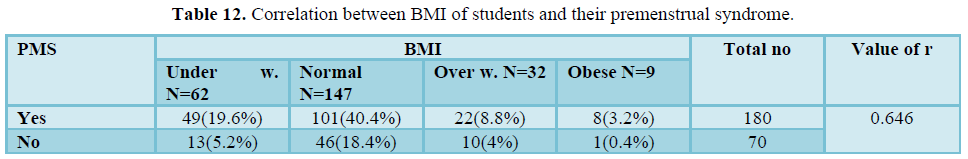 Table 13 shows that there was weak positive correlation of body mass index of students and dysmenorrhea (r = 0.106). There was very weak relation between BMI and dysmenorrhea
Table 13 shows that there was weak positive correlation of body mass index of students and dysmenorrhea (r = 0.106). There was very weak relation between BMI and dysmenorrhea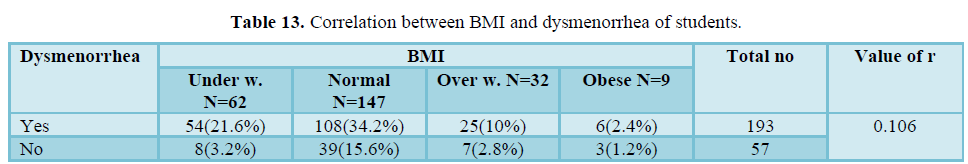
DISCUSSION
Menstruation is a female phenomenon and an important component of the active reproductive life of a woman. It starting with menarche in young girls and terminates with menopause. Thereby it becomes a regular monthly event that culminates into social, sexual, and reproductive life. It is considered as indicator of women’s health [24,25]. Menstrual problems include menstrual cycle irregularities (of duration or length), hyper-or hypomenorrhea, poly-or oligomenorrhea, dysmenorrhea, amenorrhea, menorrhagia and premenstrual syndrome [16]. In this study, out of the 250 respondents, 72.4% had regular menstrual cycles and 27.6% had abnormal and irregular cycles. According to the BMI categorization, underweight reported in 62 (24.8%), normal reported in 147 (58.8%), overweight reported in 32 (12.8%) and obese reported in 9 (3.6%) respondents. In this study, 24% respondents had heavy menstrual blood flow and lasting more than 7 days, these students were reported in menorrhagia, 12% polymenorrhea, 37.2% oligomenorrhea, 14% hypomenorrhea (scanty or little blood flow) were reported by the students. Here, 77.2% had dysmenorrhea and 72% had premenstrual syndrome were reported by the students among 250 participants. The students whose have irregular menstrual cycle, most of them were underweight (10.4%) and overweight. In this study, most of the students (8.4%) were underweight and they faced their menstrual cycle once in three months. 3.6%, 7.6% and 0.8% were underweight, normal and overweight respectively and they had polymenorrhea. 9.6%, 18.4%, 6.8% and 2.4% were underweight, normal, overweight and obese respectively and they had oligomenorrhea. 2%, 3.6% and 0.4% respondents were underweight, normal, overweight and respectively and they had hypomenorrhea. 3.2%, 7.6%, 2% and 0.4% respondents were underweight, normal, overweight and respectively and the duration of menstrual flow of them were greater than 7 days. Most of the respondents who experienced PMS symptoms were normal 40.4%, underweight 19.6%, overweight 3.2% and obese 3.2%. Most of the student known about hygiene and 8.4% of the students don’t know about hygiene. 6.8% of the students did not use sterile sanitary pad during menstruation. Most of the students used 1-2 pads per day (56%), 33.2% used 3-4 pads and 10.8% used more than 5 pads per day. A study reported a positive correlation between body mass index and menstrual profile as duration, length and amount of menstruation (r = 0.138, 0.313, 0.144) respectively. This study shows a strong positive correlation between BMI and menstrual profile as menstrual cycle (r = 0.651), menstrual cycle irregularities (r= 0.820) and premenstrual syndrome (r = 0.646). There was weak positive correlation between BMI and menstrual profile as cycle length (r = 0.044), duration of menstrual flow (r = 0.434), amount of menstrual flow (r = 0.185) and dysmenorrhea (r = 0.106). A study found that 37.67% girls seek the treatment for their menstrual problems [9]. Another study showed that 6% girls from Dhaka seek the treatment from physician for common menstrual problem [26]. In my study, 30.4% students were used various type of treatment like drug, hormone and other types. The respondents were used various type of drugs like Paracetamol Butapen, Nospa, Algine, Losectine, Met500, Norvis, Hprds, Neso, Sonap, Bigmet and so on. Some of the respondents have any other major disease like asthma, hormonal problem and migraine problem. A few respondents (3.1%) have asthma. There were some limitations of this study including a small group of populations from a particular area and age limitation. Menstrual irregularities associated with multiple factors. Menstrual cycle regulated by different hormones. This study only symptom-based prevalence study. In these study molecular and genetic factors were not analyzed. Further more precise study will be required to take this consideration into account.
CONCLUSION
This population based cross-sectional study demonstrated menstrual profile and BMI and correlation of menstrual irregularities with BMI of some populations. The result showed that there was a significant positive correlation between menstrual cycle irregularities and BMI. The result also showed that there was a significant positive correlation between BMI and menstrual profile. Therefore, objective and findings of this study are very much relevant to the public health concern of Bangladesh.
-
Goldman MB, Hatch MC (2004) Menstruation and menstrual disorders. Women & Health. California, USA. Academic Press, pp: 99-113.
-
Hall JE (2011) Guyton and Hall Textbook of Medical Physiology. 12th edition, Pennsylvania, USA, Saunders Elsevier, pp: 987-1002.
-
Lawrence M, Nelson MD (2009) Menstruation and menstrual cycle fact sheet. Accessed on: January 13, 2013. Available online at: https://www.womenshealth.gov/files/documents/fact-sheet-menstrual-cycle.pdf
-
Harlow SD, Campbell OMR (2004) Epidemiology of menstrual disorders in developing countries: A systematic review. BJOG 111(1): 6-16.
-
Liu Y, Gold EB, Lasley BL, Johnson WO (2004) Factors affecting menstrual cycle characteristics. Am J Epidemiol 160(2): 131-140.
-
Berek SJ (2015) Berek and Novak’s Gynecology. 16th edition, Lippincott Williams & Wilkins, pp: 998-999.
-
Fujiwara T (2005) The discrepancy between BMI and self-recognition of adequate body weight may cause insufficient food intake and habits in young women in Japan. Bullet Ashiya Coll 27: 75-80.
-
Hollmann M, Runnebaum B, Gerhard I (1997) Impact of waist-hip-ratio and body-mass-index on hormonal and metabolic parameters in young, obese women. Int J Obes Relat Metab Disord 21: 476-483.
-
Hartz AJ, Barboriak PN, Wong A, Katayama KP, Rimm AA (1997) The association of obesity with infertility and related menstrual abnormalities in women. Int J Obes 3: 57-73.
-
Harlow SD, Matanoski GM (1991) The association between weight, physical activity and stress and variation in the length of the menstrual cycle. Am J Epidemiol 133: 38-49.
-
Tayebi N, Yazdanpanahi Z, Yektatalab S, Pourahmad S, Akbarzadeh M (2018) The relationship between body mass index (BMI) and menstrual disorders at different ages of menarche and sex hormones. J Natl Med Assoc 110: 440-447.
-
Chang PJ, Chen PC, Hsieh CJ, Chiu LT (2009) Risk factors on the menstrual cycle of healthy Taiwanese college nursing students. Aust N Z J Obstet Gynaecol 49: 689-694.
-
Mustaqeem M, Sadullah S, Waqar W, Farooq MZ, Khan A, et al. (2015) Obesity with irregular menstrual cycle in young girls. Mymensingh Med J 24: 161-167.
-
Bae J, Park S, Kwon JW (2018) Factors associated with menstrual cycle irregularity and menopause. BMC Womens Health 18: 36.
-
Rowland AS, Baird DD, Long S, Wegienka G, Harlow SD, et al. (2002) Influence of medical conditions and lifestyle factors on the menstrual cycle. Epidemiology 13: 668-674.
-
Joffe H, Hayes FJ (2008) Menstrual cycle dysfunction associated with neurologic and psychiatric disorders: Their treatment in adolescents. Ann N Y Acad Sci 1135: 219-229.
-
Saso S, Chatterjee J, Georgiou E, Ditri AM, Smith JR, et al. (2011) Endometrial cancer. BMJ 343: d3954.
-
Harlow SD, Ephross SA (1995) Epidemiology of menstruation and its relevance to women’s health. Epidemiol Rev 17: 265-286.
-
Alam T, Jiwane R, Choudhary AK, Kishanrao SS (2015) Relationship of Body Mass Index & the age at Menarche among Young Girls. J Den Med Sci 14: 79-83.
-
Begum J, Hossain AM, Nazneen SA (2009) Menstrual pattern and common menstrual disorders among students in Dinajpur Medical College. Dinajpur Med Col J 2: 37-43.
-
Brown JB (2011) Types of ovarian activity in women and their significance: The continuum (a reinterpretation of early findings). Hum Reprod Update 17: 141-158.
-
Forrester-Knauss C, Stutz EZ, Weiss C Tschudin S (2011) The interrelation between premenstrual syndrome and major depression: Results from a population-based sample. BMC Pub Health 11: 795.
- Dars S, Sayed K, Yousufzai Z (2014) Relationship of menstrual irregularities to BMI and nutritional status in adolescent girls. Pak J Med Sci 30: 141-144.
- Samir N, Fattah HN, Sayed EM (2015) The correlation between body mass index and menstrual profile among nursing students of Ain Shams University. Egypt Nurs J 10: 1.
- Adebimpe WO, Farinloye EO, Adeleke NA (2017) menstrual pattern and disorders and impact on quality of life among university students in south-western Nigeria. J Basic Clin Reprod Sci 5: 27-32.
- Kabir H, Saha CN, Gazi R, Wirtz AL (2014) Treatment-seeking behavior of unmarried adolescent girls for selected reproductive health problems in two rural areas and one urban slum area of Bangladesh. Reprod Health 11(1): 54.







