3075
Views & Citations2075
Likes & Shares
Background: Atlanto-axial (C1-C2) osteoarthritis (AAOA) causes severe progressive sub occipital neck pain that is usually resistant to conservative therapy. Posterior fusion surgery is performed to stabilise the C1-C2 segment and alleviate the pain. Fusion surgery for neck pain is considered controversial due to a perceived lack of efficacy.
Methods: 23 Patients who underwent posterior atlanto-axial fixation surgery for AAOA were enrolled. Patient demographics and surgical technique were recorded. Surgical technique included trans articular fixation (TAS) and supplemental posterior Sonntag wiring or C1-C2 lateral mass fixation (Harms technique). Some patients required a combination of fixation due to anatomical variation. Primary outcome measures including patient satisfaction, pain, disability scores and range of motion were recorded for all patients pre- and post-operatively. Post-operative assessment was supplemented with CT and x-ray imaging.
Results: 23 patients (19 women, 4 males, mean age 71.8 ± 6.3 years) underwent surgical fixation. 8 underwent TAS, 7 had Harms and 8 had a hybrid fixation. All patients reported statistically significant improvement in pain scores. Average VAS preoperatively was 9.4. Average VAS postoperatively was 2.9, P
Conclusion: Posterior atlanto-axial fusion is highly effective for the surgical treatment of intractable neck pain secondary to atlanto-axial lateral mass osteoarthritis (AAOA). Surgery offers a high rate of symptom relief. If anatomical variability exists, both trans articular and pedicle screw fixation can be used in the same patient.
Keywords: Atlanto-axial, Osteoarthritis, C1-C2, Cervical, Fusion, Arthritis
INTRODUCTION
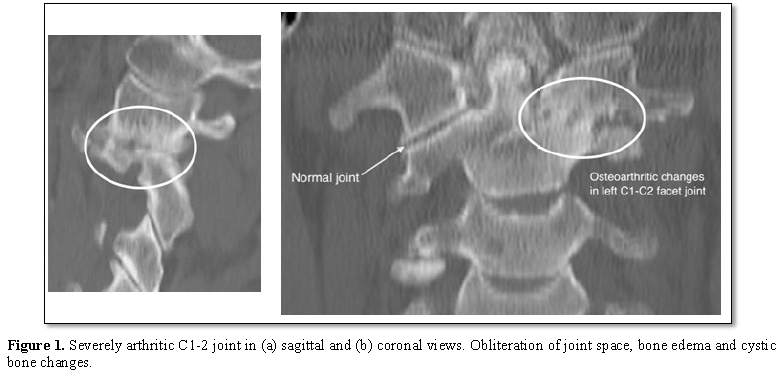
All patients will develop radiological cervical spondylotic changes with age. Sub axial cervical spine osteoarthritis (OA) is seen in virtually all patients after age 65. Atlanto-axial (AA) OA is rare, occurring in only 4% of OA sufferers. It causes unilateral suboccipital pain exacerbated by lateral rotation on the affected side with reduced range of movement (Figure 1) [1]. It may be associated with suboccipital neuralgia. Surgical intervention is considered when conservative treatment fails. C1-2 fusion was first performed in 1939 using posterior wiring [2]. Posterior transarticular screw fixation (TAS) was first performed in 1987 [3]. Harms and Melcher first performed pedicle screw fixation in 2001. This avoids the need for posterior cable fixation and allows a more minimally invasive surgical exposure [4].
The surgical objective is stabilisation of the atlanto-axial joint to provide symptomatic relief. The purpose of our study is to assess the clinical and radiographic outcomes of surgical treatment for AAOA by a single surgeon (TS). Radiological fusion was assessed using x-ray and CT. There has only been one previous study reporting on hybrid fixation techniques [5].
METHODS
The St Vincent’s Hospital Human Research Ethics Committee approved this study (SVH file number: 16/054). Patients undergoing posterior atlanto-axial surgery between 2005-2015 at our institution performed by the senior author (TS) were identified. Demographic data including gender, age, length of hospital-stay and follow-up time was recorded. Diagnosis was made via clinical and radiological criteria. CT with bone window was used to confirm the diagnosis. Unilateral C1-C2 osteoarthritis was seen in all cases with severe joint space narrowing, osteophyte formation and subchondral sclerosis on the side of pain (Figure 1).
Preoperative and postoperative satisfaction scores were recorded using the Visual Analogue Scale (VAS) and Neck Disability Index score (NDI) [6]. Patients were asked if in hindsight they would have the surgery again. Postoperative range of movement in flexion, extension and lateral rotation was recorded. Secondary outcome measures were the presence of fusion and periprosthetic complications assessed on CT. Joint fusion was assessed by the obliteration of the joint space with evidence of mature bone fusion across the C1-C2 joint.
Data analysis was carried out using SPSS Statistics version 23 (SPSS Inc., Chicago Ill USA). Data is presented as a mean ± standard deviation. One Sample Kolmogorov-Smirnov test was carried out to assess normality of data set, and Wilcoxson Signed-Rank test was performed to ascertain significance in measures in the pre-operative and follow-up setting. Non-parametric tests were used due to the sample size. Fisher’s exact test was used to determine the independence of the outcome variables. Statistical significance was accepted at the p
RESULTS
23 patients with AAOA were enrolled in the study, 19 female and 4 males (Mean age at surgery was 67.2 (range 51-77). Mean follow-up time was 55.3 months (range 11-132) (Table 1). All patients had severe progressive pain localised to the ipsilateral suboccipital region exacerbated by lateral rotation to the affected side. Most patients had limited range of lateral rotation at time of presentation. Other preoperative symptoms included suboccipital headache (15 patients), orbital pain (2 patients) and shoulder pain (6 patients). All patients had been treated conservatively prior to presentation with analgesia, immobilisation and facet joint injections.
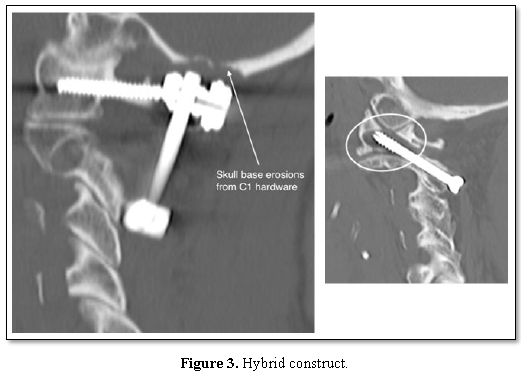
Choice of fixation technique was determined at time of surgery by the senior surgeon (TS) using image guidance (BrainLab AG Feldkirchen, Germany). 8 patients underwent TAS fixation with posterior wiring and bone graft and 8 patients had lateral mass pedicle screw fixation according to Harms’ method. 7 patients had hybrid fixations with TAS fixation on one side and pedicle screw fixation on the other due to anatomical variation. TAS fixation was revised in one patient to a Harms fixation due to lack of fusion 14 months following initial surgery. One patient with a Harms fixation was revised to a TAS fixation due to trauma causing fracture of both C1 screws 3 years post initial surgery.
VAS pain scores were significantly reduced immediately following surgery. The mean pre-operative VAS was 9.4 ± 0.8 compared to post-operative score of 2.9 ± 2.0 at the time of follow-up (Z=4.200, p<0.0005). All patients reported virtually complete abolition of pain postoperatively. In some patients, mild recurrent neck pain recurred 3-4 years following surgery.
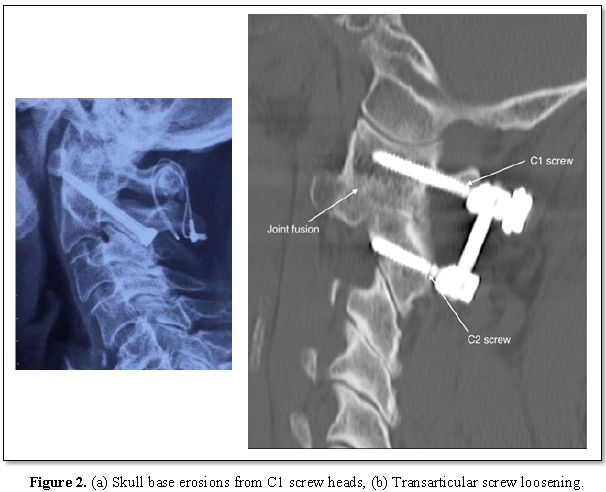
Mean NDI score prior to surgery was 72.2 which reduced to 18.9 post-operatively (Z=4.199, p<0.0005) (Table 1). Pre and post-operative range of movement measures were identical with lateral rotation most affected. Radiological fusion was shown in 21 patients (95.5%). 2 patients’ scans revealed skull base erosion around the head of the Harms screw (Figure 2a). One patient had a non-union with recurrence of pain 4 years post TAS fixation; CT demonstrated implant loosening and resorption of bone graft (Figure 2b). 21 of the 23 patients (91.3%) stated they would undergo the surgery again.
DISCUSSION
AAOA has a unique natural history compared to other degenerative spinal disorders [7,8]. Relatively few studies reporting outcomes of cervical fusion for AAOA have been published, with only one meta-analysis of 23 studies containing 246 patients in 2013 [9]. Diagnosis is often delayed due to non-specific or atypical symptoms and pain management is often the only treatment offered [9]. C2 radiofrequency lesioning and ganglionectomy have been trialled to alleviate symptoms [9]. However, these techniques fail to address the underlying pathology and symptoms inevitably progress. Internal fixation of the atlantoaxial segment presents a significant surgical challenge to the spine surgeon, with non-union rate of up to 30% [10,11]. TAS and pedicle screw fixation achieve a more rigid fixation fusion-rate >95% [4,12,13].
2 patients in our series had skull base erosions because of the proximity of the C1 screw heads to the inferior occiput (Figure 2a). One patient, a 71 year old female, underwent revision surgery one year following TAS fixation. The hardware was removed and replaced with lateral mass screws. Right sided neck pain recurred after one year; imaging showed stable fusion but significant skull base erosion (Figure 2a). C1 screws were removed and her pain improved. The second patient, a 66 year old female, developed right-sided suboccipital pain one year following the surgery. CT scan revealed similar skull base erosions, more marked on the right side.
Intraoperative stereotactic guidance was used in all our patients and all screws were in satisfactory position on post-operative imaging with no screws extending anterior to the C1 vertebra.
Only one study has previously reported the use of the hybrid fixation technique which may be required for anomalies such as a high-riding vertebral artery [5]. The 8 patients in this series who had hybrid fixations achieved identical results to those with TAS or Harms constructs (Figure 3). Our patients report satisfaction with their surgery of greater than 90%, with dramatic improvement in VAS and NDI scores postoperatively. This indicates that posterior atlantoaxial fixation is a highly successful surgical technique for the treatment of symptomatic AAOA.
CONCLUSION
Posterior cervical fixation is a highly effective technique for the surgical treatment of neck pain secondary to atlantoaxial lateral mass osteoarthritis (AAOA) that has failed to respond to conservative measures. The surgery is safe and offers a very high rate of symptom relief. Trans-articular screw and pedicle screw fusions can be used in combination with each other to adapt to anatomical and pathological variability while maintaining an extremely high surgical success rate.
CONTRIBUTIONS
· Dr Ananya Chakravorty: Paper write-up.
· Dr Ellen Frydenberg: Data collection, write-up and submission.
· Dr Timothy Steel: Original idea, design, write-up.
· Dr Mitchell Fung: Data collection and paper write-up.
1. Halla J, Hardin J (1987) Atlantoaxial (C1-C2) facet joint osteoarthritis: A distinctive clinical syndrome. Arthritis Rheum 30: 6.
2. Gallie W (1939) Fractures and dislocations of the cervical spine. Am J Surg 46: 5.
3. Magerl F, Seemann PS (1987) Stable posterior fusion of the atlas and axis by transarticular screw fixation. Springer, p: 6.
4. Harms J, Melcher RP (2001) Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine 26: 2467-2471.
5. Kang DG, Lehman Jr RA, Wagner SC, Peters C, Riew KD (2017) Outcomes following arthrodesis for atlanto-axial osteoarthritis. Spine 42: E294-E303.
6. Vernon H (2008) The neck disability index: State-of-the-art, 1991-2008. J Manipulative Physiol Ther 31: 12.
7. Goel A, Shah A, Gupta SR (2010) Craniovertebral instability due to degenerative osteoarthritis of the atlantoaxial joints: Analysis of the management of 108 cases. J Neurosurg Spine 12: 592-601.
8. Elliott R, Tansweer O, Smith M, Frempong-Boadu A (2013) Outcomes of fusion for lateral atlantoaxial osteoarthritis: Meta-analysis and review of literature. World Neurosurg 80: 10.
9. Holly LT, Batzdorf U, Foley KT (2000) Treatment of severe retromastoid pain secondary to C1-2 arthrosis by using cervical fusion. J Neurosurg 92: 162-168.
10. Gore D, Sepic S, Gardner G (1986) Roentgenographic findings of hte cervical spine in asymptomatic people. Spine 11: 4.
11. Bekelis K, Gottfried O, Wolinsky JP, Gokaslan Z, Omeis I (2010) Severe dysphagia secondary to posterior C1-C3 instrumentation in a patient with atlantoaxial traumatic injury: A case report and review of the literature. Dysphagia 25: 5.
12. Neo M, Matsushita M, Iwashita Y, Yasuda T, Sakamoto T, et al. (2003). Atlantoaxial transarticular screw fixation for a high-riding vertebral artery. Spine 28: 5.
13. Grob D, Bremerich FH, Dvorak J, Mannion AF (2006) Transarticular screw fixation for osteoarthritis of the atlanto axial segment. Eur Spine J 15: 283-291.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Alcoholism Clinical Research
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Ophthalmology Clinics and Research (ISSN:2638-115X)