3395
Views & Citations2395
Likes & Shares
INTRODUCTION
Extrarenal malignant rhabdoid tumor is a rare tumor with poor prognosis, 16 vulvar cases have been reported so far in English literature [1].
The malignant rhabdoid tumor was described as a rhabdomyosarcomatoid variant of Wilms’s tumor [2]. The rhabdoid terminology was adopted due to the similarity of tumor cells with epithelioid sarcoma and differentiation between each other is difficult. The most common site has been reported such as hemivulva, the labia majora, mons pubis and combined labia majora and mons pubis [1,3].
The “rhabdoid cells” features are composed by a diffuse proliferation of rounded or polygonal cells with eccentric nuclei, glassy eosinophilic cytoplasm containing hyaline-like inclusion bodies, arranged in nests or sheets, and prominent nucleoli. These features are present in renal cell carcinoma and soft tissue sarcoma such as leiomyosarcomas, synovial sarcomas and extra skeletal myxoid chondrosarcomas [4].
The recurrence is common in a short period of time such as 2 months to 8 months.
We report a case the 15th case of right hemi vulvar rhabdoid tumor with reconstruction with profunda artery perforator flap (PAP flap) and three years later recurrence on mons pubis with reconstruction with PAP flap combined with gracilis muscle.
CASE REPORT
44 years old woman whom 3 years before was operated for right malignant vulvar rhabdoid tumor with radical hemi vulvectomy and bilateral inguinal femoral lymph node resection. The initial lesion was a single nodular lesion, indurated, located in right labia majora with 3 cm diameter and irregular borders. The wide defect could not be closed primary and we decided to do a profunda artery perforator pedicle flap to cover the wound debulking and z-plasty procedures were performed months later after reconstruction. Three years later developed a recurrence of the tumor in hypogastric 3 cm length, nodular-like, bluish, indurated. The tumor was removed with 3.5 cm of margin around the lesion including the muscular fascia. The sample was sending to frozen pathology and reported sarcoma with rhabdoid feature with margins free.
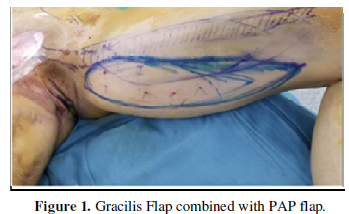
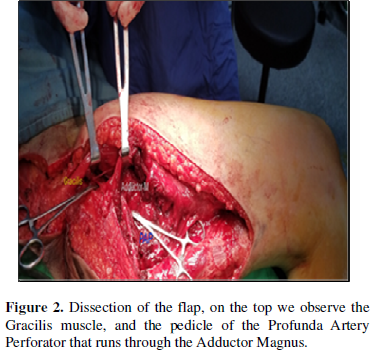
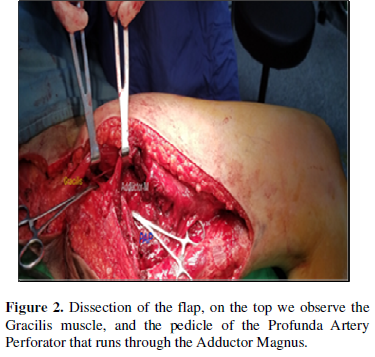
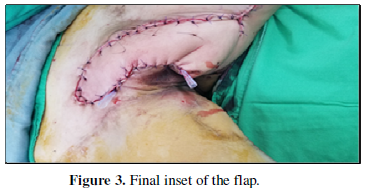
The reconstruction plan was a pedicle Profunda artery perforator (PAP) flap with gracilis pedicle muscle flap (Figures 1-3) and mesh to cover the wound and drain was placed on the wound. The donor site was closed primary and drain was placed on the wound.
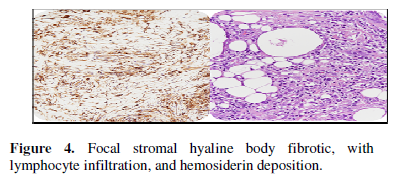
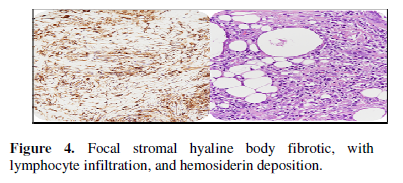
The microscopic outcomes in the initial tumor and the recurrence were compatible with malignant extrarenal rhabdoid tumor with prominent nucleoli, cytoplasm with hyaline-like inclusions and hyaline fibrosis bodies (Figure 4a), xanthogranulomatous inflammation with histiocyte and lymphocyte infiltration and high mitotic activity. INI-1 staining was not contributory. The histiocytes were positive to CD68 staining (Figure 4b). The lymph node section in the first surgery were negative for malignancy.
DISCUSSION
The malignant rhabdoid tumor initially was described as a rhabdomyosarcoma variant of Wilms’s tumor, and were described as extrarenal tumor described in soft tissue, urogenital tract, bowel, skin prostate, liver and central nervous system, then was recognized as an independent clinico-pathological entity [5,6]. The rhabdoid cells presence in a sample leads the diagnosis and the aggressivity of the tumor behavior [7]; most of the reported cases has been described as a painless firm-hard circumscribed mass of 2 to 10 cm diameter most of them with primary closure of the wound and inguinal lymphatic resection. Only one case was reported with reconstruction by pedicle rectus abdominis flap due to the large defect including the inguinal lymph node area resection (Table 1) [3]. The tumor usually express vitamin and cytokeratin, and do not retain the nuclear expression of INI-1 protein. The surgery is the first line of management with small margins usually 2 cm, there is no consensus regarding the margins neither the adjuvants therapy, and chemotherapy and radiotherapy has not shown be effective in controlling the recurrence, that is why we recommend extend the margins and closure the wound with pedicle flaps. The histopathological tumor has to include the exclusion of other sarcomas, melanomas and carcinomas due to has S100 marker and PAS marker positive in some cases [13]. The CD68 staining is a marker of histiocytes and histiocytic tumors.
The transverse upper gracilis (TUG) muscle flap combined with profunda artery perforator (PAP) flap has been described for breast and perineal reconstruction in defects that requires a large and substantial coverage [18]. The anatomical territories in the posteromedial area between the TUG-PAP gives the combination of two different major angiosome nourishment the flap, the medial circumflex femoral artery territory (TUG) and profundal femoral artery territory (PAP) [19]. Usually, the TUG flap gives its main pedicle of the muscle at 6 to 8 cm along the muscle, and PAP offers 2 to 5 perforators along the posterior medial thigh and its proximity offers a perfect match with both flaps in defects that requires muscle and skin coverage.
The rhabdoid tumor is an aggressive tumor that in every case the lymph node resection and the wide excision with its reconstruction should to be consider and the PAP-TUG flap is a wise option of reconstruction due to its proximity.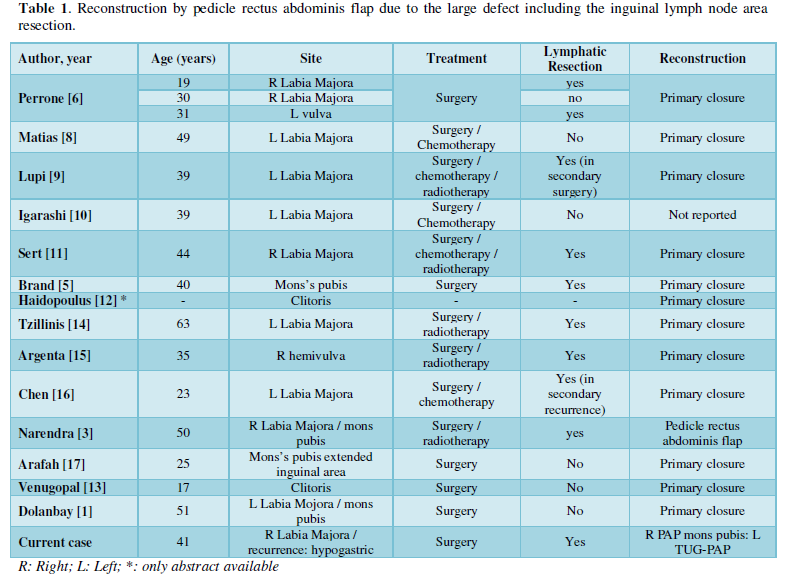
- Dolanbay M, Kutuk M, Uludag S, Tonguc M, Ozcelik B, et al. (2016) Malignant rhabdoid tumor of the vulva: A case report and review of the literature. Taiwan J Obstet Gynecol 55: 128-130.
- Beckwith JB, Palmer NF (1978) Histopathology and prognosis of Wilms tumors: Results from the First National Wilms’s Tumor Study. Cancer 41: 1937-1948.
- Narendra H, Ray S, Rao L, Geetha V (2010) Malignant extrarenal rhabdoid tumor of the vulva in an adult. J Cancer Res Ther 6: 82-85.
- Oda Y, Tsuneyoshi M (2006) Extrarenal rhabdoid tumors of soft tissue: Clinicopathological and molecular genetic review and distinction from other soft-tissue sarcomas with rhabdoid features. Pathol Int 56: 287-295.
- Brand A, Covert A (2001) Malignant rhabdoid tumor of the vulva: Case report and review of the literature with emphasis on clinical management and outcome. Gynecol Oncol 80: 99-103.
- Perrone T, Swanson PE, Twiggs L, Ulbright TM, Dehner LP (1989) Malignant rhabdoid tumor of the vulva: Is distinction from epithelioid sarcoma possible? A pathologic and immunohistochemical study. Am J Surg Pathol 13: 848-858.
- Yorulmaz G, Erdogan G, Pesterli HE, Savas B, Karaveli FS (2007) Epithelioid leiomyosarcoma with rhabdoid features. Wien Klin Wochenschr 119: 557-560.
- Matias C, Nunes JF, Vicente LF, Almeida MO (1990) Primary malignant rhabdoid tumor of the vulva. Histopathology 17: 576-578.
- Lupi G, Jin R, Clemente C (1996) Malignant rhabdoid tumor of the vulva: A case report and review of the literature. Tumori 82: 93-95.
- Igarashi T, Sasano H, Konno R, Sato S, Namiki T, et al. (1998) Malignant rhabdoid tumor of the vulva: Case report with cytological, immunohistochemical, ultrastructural and DNA ploidy studies and review of the literature. Pathol Int 48: 887-891.
- Sert MB, Onsrud M, Perrone T, Abbas F, Currie JL (1999) Malignant rhabdoid tumor of the vulva. Case report. Eur J Gynaecol Oncol 29: 258-261.
- Haidopolous D, elsheikh A, Vlahos G, Sotiropoulou M, Rodolakis A, et al. Malignant rhabdoid tumor of the clitoris in an elderly patient: Report of a case. Eur J Gynecol Oncol 23: 447-449.
- Venugopal PR, Padma R (2013) Rare Malignant tumors of clitoris: A case report. Indian J Surg 76(3): 230-233.
- Tzilinis A, Clarke LE, Affuso C, Fessenden J (2002) Successful treatment of malignant rhabdoid tumor of the vulva in an older patient: A case report and review of literature. Curr Surg 59: 570-571.
- Argenta PA, Thomas S, Chura JC (2007) Proximal-type epithelioid sarcoma vs. malignant rhabdoid tumor of the vulva: A case report, review of the literature, and an argument for consolidation. Gynecol Oncol 107: 130-135.
- Chen J-R, Tzen C-Y, Yang Y-C (2009) Metronomic paclitaxel and thalidomide for rapidly metastatic primary vulvar malignant rhabdoid tumor. Int J Gynaecol Obstet 106: 70-71.
- Arafah MA, Aljuboury MI (2011) Primary vulvar rhabdoid tumor in an adult: A case report, immunohistochemical profile and literature review. Case Rep Med 2011: 162709.
- Ciudad P, Marucia M, Orfaniotis G, Weng H-C, Constantinescu T, et al. (2016) The combined transverse upper gracilias and profunda artery perforator (TUGPAP) flap for breast reconstruction. Microsurgery 36(5): 359-366.
- Ahmadzadeh R, Bergeron L, Tang M, Geddes CR, Morris SF (2007) The posterior thigh perforator flap or profunda femoris artery perforator flap. Plast Reconstr Surg 119(1): 194-200.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Rheumatology Research (ISSN:2641-6999)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)