3277
Views & Citations2277
Likes & Shares
The cytosteatonecrosis newborn (neonatal CSN) is a rare neonatal emergency.
It occurs in the newborn term or post-term, macrosome, with a history of hypoxia, hypothermia, instrumental extraction or caesarean section. Maternal factors such as gestational diabetes and pre-eclampsia were incriminated. A terrain related to the child has been suspected in several cases such as anemia or thrombocytosis. The major complication is hypercalcemia, which occurs in about one third of cases.
The treatment of is not codified, it is essentially symptomatic. We report 4 observations, to remind you of the urgency of a neonatal clinical entity who is here cytosteatonecrosis, often revealing hypercalcemia can be fatal if diagnosed late.
Keywords: Cytosteatonecrosis, Newborn, Hypercalcemia
INTRODUCTION
The fat necrosis of the newborn (CSN) is an acute hypodermitis that develop during the first days of life [1]. It is in the form of indurated and purplish cutaneous cups on light skin or hyperchromic on black skin, often located on the face, trunk, buttocks and root of the limbs. Histologically, under a normal epidermis and dermis, there is a lobular panniculitis with focal areas of eosinophilic necrosis of the adipose tissue, including optically empty intra- adipocyte radiative clefts corresponding to dissolution and lipid crystallization [2].
The main risk situations classically reported are fetal macrosomia, often in the context of a diabetic mother, perinatal asphyxia, severe hypothermia and tissue trauma during instrumental maneuvers or during neonatal resuscitation [2,3]. The evolution of cytosteatonecrosis is in good condition. However, in some cases, the occurrence of severe hypercalcemia may lead to some life-threatening complications [3,4]. We report here four observations of CSN in the newborn with a description of the context of occurrence and evolution in the medium term.
CASE STUDY
Case 1
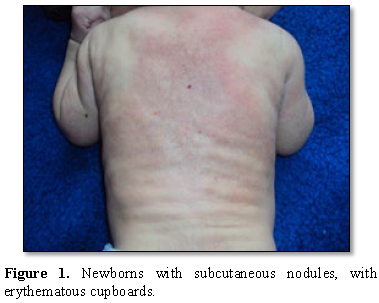
It is a newborn male, born at term, vaginally in a context of perinatal asphyxia with a purulent amniotic fluid. A maneuver of abdominal expression was performed by the midwife to promote expulsion. The child was resuscitated. The birth weight was 4200 g. He was referred for skin induration observed by parents on the 10th day of life. The observation of the lesions showed erythematous placards evoking neonatal cytosteatonecrosis of right dorsal and scapulo-axillary location and arms (Figure 1).
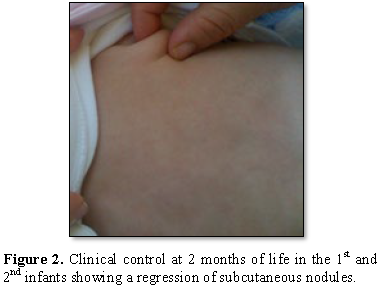
Calcemia was normal as well as abdominal ultrasound. He was put under surveillance without supplementation with vitamin D. At 2 months of life, the cutaneous lesions had completely regressed without sequels (Figure 2).
Case 2
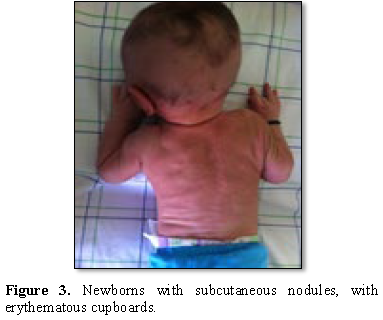
This is a new born male with notion of sufferance fetal birth with gestational diabetes maternal history. He presented three days after his birth of the subcutaneous cupboards, hard, painful on the back, buttock and cheeks; with at biological assessment hypercalcemia (Figure 3).
erythematous cupboards.
Renal ultrasound not found nephrocalcinosis and the Facial CT showed jugular nodules of fat density without calcification. The diagnosis this cytosteatonecrosis has been retained on all clinical criteria. Treatment consisted of analgesic treatment, hydration and a low calcium diet in 4 infants. A parenteral saline hyperhydration associated with a loop diuretic (furosemide/Lasilix ™) allowing a long-term normalization of the calcemia and a complete regression of the cutaneous signs from the age of two months (Figure 4).
Case 3
This is a newborn male, born vaginally in a context of acute fetal distress, with a birth weight of 4700 g, requiring resuscitation at birth, the score of APGAR was at 3/6/8. The lesions were found on day 12 of life. These are cervico-dorsal indurated inflammatory placards, suggestive of cytosteatonecrosis (Figures 5 and 6).
The serum calcium was normal. There was an inflammatory syndrome with CRP at 26 mg/L and leukocytosis at 20,500/mm3. It has benefited from a simple monitoring with no vitamin D supplementation. The cutaneous lesions have totally regressed 5 months of life with persistence of thin e atrophy in places.
Case 4
This is a newborn male admitted to 6 days of life, born at the end of 40 weeks of amenorrhea (SA), by caesarean section for acute fetal distress. The birth weight was 4300 g. He was successfully resuscitated at birth with aspiration, ventilation and external cardiac massage. On the sixth day of life, subcutaneous placards appeared, nodular in places, fairly extensive, sitting all over the back, buttocks, thighs, shoulders and cheeks. The diagnosis of neonatal cytosteatonecrosis was retained. There was a biological inflammatory syndrome with leukocytosis at 22,800/mm3 and CRP at 192 mg/L. The initial serum calcium level was 86 mg / L, and then gradually increased to 124 mg/L to 27th day of life. ECG and abdominal ultrasound were normal.
Treatment, consisting of intravenous hyperhydration with isotonic saline at 150 mL/kg and furosemide at 1 mg/kg daily, allowed rapid normalization of serum calcium in 72 h. The infant was then fed within its purposes any vitamin D. At the 6th months of life, the cupboards had totally regressed. Calcium and renal function were normal at 6 months.
DISCUSSION
We reported these 4 cases of early neonatal CSN in order to describe the symptomatology and to specify the evolution of lesions in the medium term.
The cytosteatonecrosis of the newborn is a panniculitis, whose frequency is difficult to estimate. It occurs in the newborn term or post-term, macrosome, with a history of hypoxia, hypothermia, instrumental extraction or caesarean section [1-3]. Maternal factors such as gestational diabetes and pre-eclampsia were offending. Child-related terrain has been suspected in several cases such as anemia or thrombocytosis.
Although the CSN in the neonatal period is very well described, its occurrence remains very rare. Lesions usually appear early in the first week of life [5-7].
CSNN is manifested by subcutaneous nodules, painful; with erythematous placards appear on average 4 days after birth on the face, buttocks, trunk or root of the limbs. Histologically, it is granulomatous panniculitis lobular. The differential diagnosis arises with the sclerema neonatal and the erysipelas painful. The topography of lesions observed in our patients overlaps with that reported in clinical observations, in particular their location in the buttocks, thighs, trunk and cheeks [4,5].
The major complication is hypercalcemia, which occurs in about one third of cases. She could be explained by the increase in bone resorption or by the 1.25 synthesis dihydroxycholecalciferol by the cells granulomatous. hypercalcemia may lead to kidney complications (nephrocalcinoses and lithiasis) threaten the functional prognosis, cardiac and neurological sometimes lethal [3,4].
The risk of this hypercalcemia is directly related to the extension of skin lesions.
The treatment of neonatal CSN is not codified; it is essentially symptomatic (warming, rehydration). Conventional treatment in case of severe hypercalcemia associates saline hyperhydration, diuretics hypercalciuriants, low dose corticosteroids and a diet low in calcium and vitamin D. The use of bisphosphonates remains questionable.
Biological monitoring of serum calcium and ultrasound is essential and extended up to 1 year [8,9].
The CSN is in good standing with an evolution towards healing without sequelae. Clinically, the local inflammation progressively fades, the fatty infiltrate regresses more slowly in a few weeks to a few months to give way to atrophy of the subcutaneous tissue of variable duration [10].
CONCLUSION
Neonatal fat necrosis is a condition well described but rarely seen in current practice and therefore often ignored by practitioners. It is generally of benign evolution. The main complication is hypercalcemia which is often asymptomatic but can sometimes be threatening, justifying prolonged monitoring of the calcium level, if possible even after the disappearance of the cutaneous lesions. Progression to superinfection andabcédation lesions is possible but seems rare. Through these observation, we recall the urgency of this neonatal clinical entity which is often revealing hypercalcemia can be fatal if diagnosed late.
1. Mahe E, De Prost Y (2007) The cytosteatonecrosis of the newborn. Ann Dermatol Venereol 134: 494-498.
2. Begon E, Blum L, Petitjean B, Jacomet L, Merbouche S, et al. (2012) Subcutaneous fat necrosis of the newborn (fat necrosis) and hypercalcemia after hypothermia therapeutic. Ann Dermatol Venereol 139: 601-602.
3. Tizki S, Lehlimi M, Habzi A, Benomar S (2013) Neonatal cytosteatonecrosis: Pay attention to hypercalcemia, even late! J Pediatr Puericult 26: 105-108.
4. Barltrop D (1963) Hypercalcemia associated with neonatal subcutaneous fat necrosis. Arch Dis Child 38: 516-518.
5. Singalavanija S, Limponsanurak W, Wannaprasert T (2007) Subcutaneous fat necrosis of the newborn. J Med Assoc Thai 90: 1214-1220.
6. Perrotta R, Virzi D, Tarico MS (2010) A rare case of congenital ulcerated subcutaneous fat necrosis of the newborn. J Plast Reconstr Aesth Surg 63: e801-802.
7. Lewis HM, Ferryman S, Gatrad AR (1994) Subcutaneous Moss C fat necrosis of the newborn associated with hypercalcemia. J R Soc Med 87: 482-483.
8. Holzel A (1950) Subcutaneous fat necrosis of the newborn. Arch Dis Child 26: 89-91.
9. Vijayakumar M, Prahlad N, Nammalwar BR, Shanmughasundha R (2006) Subcutaneous fat necrosis with hypercalcemia. Indian Pediatr 43: 360-363.
10. Sfaihi L, Kmiha S, Aloulou H, Kamoun T, Hachicha M (2013) Biphosphonate therapy in subcutaneous fat necrosis with hypercalcemia and nephrocalcinosis in the newborn. J Neonatal Nurs 19: 76-79.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)