2583
Views & Citations1583
Likes & Shares
Knee osteoarthritis
is one of the most prevalent musculoskeletal diseases affecting the elderly.
Because it is characterized by the progressive degeneration of synovial joint
structure, it causes pain, loss of motion and physical disability, thus
impairing quality of life.
The
purposes of symptomatic treatment of OA of the knee are to control joint pain
and to improve joint function. The well-known pharmacological approach for
symptomatic treatment includes oral administration of paracetamol, NSAIDs and
opioids, but these therapies expose patients to risk of adverse events.
Here we present the therapeutic effects
of intra articular clodronate in four patients with knee osteoarthritis. All
patients showed an important improvement in pain VAS (mean 8.6 pre-therapy vs.
3.5 post-therapy). In addition, there has been a marked improvement in the
signs of inflammation of the treated joints: Hyperthermia and swelling. Our
therapeutic proposal would be to precede the injections of hyaluronic acid by
3-4 injections with intra-articular clodronate in order to exploit the
exclusive anti-inflammatory effect of this bisphosphonate and thus reduce the
amount of pro-inflammatory cytokines and of metalloproteases within the joint.
INTRODUCTION
Osteoarthritis
(OA) is considered to be the most common form of arthritis that results in structural
and functional failure of synovial joints [1,2].The current paradigm holds that
OA is a disease of the entire joint, involving not only the degradation of
articular cartilage but also an important subchondral bone reaction and
alteration of other joint structures, including the synovial membrane,
meniscus, capsule, ligaments and periarticular muscle. The clinical features of
OA include joint pain with activity, transient stiffness in the morning or
after rest, restricted motion, joint crepitus, periarticular tenderness, bony
swelling and functional disability. The knee is regarded as one of the most
common joints frequently affected by OA.
The
purposes of symptomatic treatment of OA of the knee are to control joint pain
and to improve joint function. The well-known pharmacological approach for
symptomatic treatment includes oral administration of paracetamol, NSAIDs,
opioids and intra-articular corticosteroid injections [3,4]. However, NSAIDs
should be used with caution in patients with peptic ulcer disease, renal
insufficiency, or cardiovascular risk [5,6]. Additionally, whereas opioids can
be used for pain relief when NSAIDs have failed, their advantageous effects are
outweighed by increased risk of adverse events and therefore should not be prescribed
routinely [7]. Intra-articular corticosteroid injections should be considered
in patients who do not respond satisfactorily to the aforementioned treatments
as well as in patients with acute exacerbations of pain and signs of local
inflammation [8].
Macrophages might play a role in the development and progression of osteoarthritis (OA). Once activated, macrophages can produce large quantities of growth factors, enzymes and proinflammatory cytokines. It has previously been shown that macrophages enhance osteophyte growth in animal models of OA [9, 10]. Furthermore, it is possible that macrophages play a role in the maintenance and progression of the disease by their contribution to synovial fibrosis, cartilage catabolism and maintenance of an inflammatory state in the joint [11] by production of growth factors [12], enzymes [13] and cytokines, respectively [14,15].
Agents
that suppress bone turnover, including bisphosphonates, have been associated
with fewer subchondral bony lesions, as visualized by MRI, in patients with OA
[16]. In several studies clodronate-laden liposomes were used for macrophage
depletion. Clodronate-laden liposomes are selectively ingested by phagocytosing
cells. After uptake, the clodronate is released, and subsequently, the cell
undergoes apoptosis [17]. Seven days after injection of clodronate-laden
liposomes, optimal depletion of macrophages is established [18]. Recently
Rossini et al. [19] indicates that intra-articular clodronate provides
symptomatic and functional improvements at least as good as those obtained with
hyaluronic acid.
Here we
present the therapeutic effects of intraarticular clodronate in four patients
with knee osteoarthritis.
PATIENTS AND METHODS
Four patients never subjected to hyaluronic acid
infiltrations (2 men and 2 women, men aged 68 years) were recruited. All of
them showed a clinical picture of acute knee osteoarthritis, with severe pain,
effusion and impaired function. Patients had undergone a knee MRI, which showed
inflammation of subchondral bone and the typical “bone marrow lesions”.
Considering the clinical and radiological analogy with
algodystrophy, we decided to treat patients with clodronate, but the intensity
of pain reported by patients (mean VAS
pain 8.6) prompted us to use clodronate by intra-articular
route of administration. Obtained the informed consent of the patients and
given the excellent tolerability of this route of administration, as reported
by previous studies [19], we adopted the following therapeutic scheme:
Clodronate 25 mg intra-articular every week for 3 weeks; patients who still had
a VAS of pain of more than 5 at week 7 underwent further administration of
intra-articular Clodronate 25 mg.
All patients underwent a careful clinical examination
before each single infiltration (weeks 1, 2 and 3) and at the last control
visit (week 11). In order to identify any allergic reactions and/or signs of
intra-periarticular infection they performed blood chemistry tests at week 1
and week 11 and performed an MRI of the infiltrated knee 11 weeks after the 1st
infiltration with clodronate.
During the 11 weeks of the study, patients were asked not
to modify therapy with NSAIDs and/or Paracetamol, which they were taking before
starting infiltrative therapy with clodronate, without notifying their
rheumatologist.
RESULTS
Of the
four patients studied, only one needed further infiltration at week 11. The
patient was a 69-year-old male, diabetic and obese.
All patients showed an important improvement in pain VAS (mean 8.6 pre-therapy vs 3.5 post-therapy; Table 1. In addition, there has been a marked improvement in the signs of inflammation of the treated joints: hyperthermia and swelling.
Patients
did not report adverse events during the weeks of observation; joint and/or
skin infections did not occur and liver and kidney function parameters did not
change during the observation period. Two patients reported burning sensation
during the infiltration, which resolved spontaneously after a few minutes,
without requiring any medical intervention.
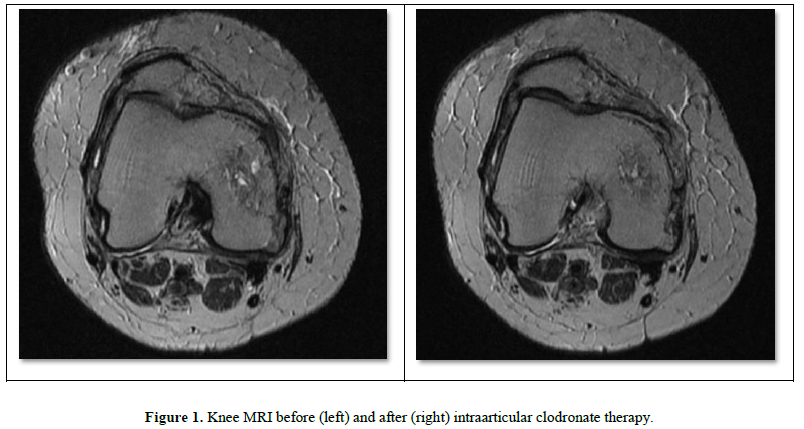
Three
out of four patients showed a significant reduction in bone marrow edema
encountered with MRI of the knee at the beginning of the observation (MRI knee
of patient No. 2: Figure 1A before and Figure 1B after 11 weeks of
observation). The fourth patient, for whom a 4th infiltration had become
necessary at the 7th week, did not show important improvements in the
radiological picture of bone marrow edema, although they presented a
significant reduction in the pain VAS.
DISCUSSION
Knee
osteoarthritis is one of the most prevalent musculoskeletal diseases affecting
the elderly. Because it is characterized by the progressive degeneration of
synovial joint structure, it causes pain, loss of motion and physical
disability, thus impairing quality of life. Current treatment strategies also
aim to alleviate joint pain, reduce physical disability and limit the
progression of joint damage [1,3]. In line with this concept, basic efforts to
establish treatment guidelines often focus on treatment efficacy.
Furthermore,
it is clear that multiple signaling molecules produced either by chondrocytes
or by neighboring fibroblasts or macrophages can also cause an activity response,
as was recently shown by Blom and colleagues [20]. Cartilage disruption leads
to leakage of large molecular complexes, such as collagens and proteoglycans,
into the synovial fluid. MMP-3 is involved in the generation of severe
cartilage damage in murine OA and synovial macrophages are crucial in early
MMP-3 activity and appear to mediate MMP-3 production in synovium rather than
cartilage [12].
In
addition, clodronate plays an important role in the transmission of pain.
Vesicular nucleotide transporter (VNUT/SLC17A9) carries ATP into secretory
vesicles in a membrane potential Cl−-dependent manner, is expressed in neurons
at primary afferent nerve terminals and in the dorsal horn of the spinal cord
and is responsible for vesicular storage and release of ATP. Experiments in
VNUT knockout (KO) (VNUT−/−) mice have revealed that VNUT in spinal dorsal horn
neurons is involved in pain and that VNUT inhibition leads to improvement of
pathological conditions with no significant changes in phenotype. Such findings
suggest that VNUT inhibitors may be effective analgesic agents with few side
effects, although therapeutic inhibitors of purinergic chemical transmission
have yet to be developed. Clodronate was the strongest VNUT inhibitor among the
bisphosphonates [21].
Numerous
studies have found that clodronate inhibits the production of several
pro-inflammatory mediators [22], inhibits the collagenase activity of MMP-1
[23] and reduces in vitro macrophage production of IL-1beta, TNF alpha and NO
[24]. The physiopathogenetic mechanisms described so far could explain the
clear reduction in pain, swelling and hyperthermia that our patients treated
with intra-articular clodronate presented; symptoms all started and worsened by
the cytokines produced by macrophages.
There
is no doubt the positive effect of intra-articular hyaluronic acid therapy on
the integrity of the cartilage layer, but in patients in whom an inflammatory
clinical picture prevails, the effect of intra-articular hyaluronic acid is
reduced or requires a greater number of intra-articular injections. Evidently a
high concentration of pro-inflammatory cytokines and metalloproteases increases
the rate of degradation of the hyaluronic acid administered, reducing or even
frustrating the therapeutic effect.
CONCLUSION
Then,
in patients with major joint inflammation, our therapeutic proposal would be to
precede the injections of hyaluronic acid by 3-4 injections with
intra-articular clodronate in order to exploit the exclusive anti-inflammatory
effect of this bisphosphonate and thus reduce the amount of pro-inflammatory
cytokines and of metalloproteases within the joint. In this way, a longer
stability of hyaluronic acid could also be obtained, with greater permanence in
the joint cavity and therefore greater therapeutic efficacy with significantly
reduced costs compared to other therapies [25].
The
experience of other authors [26] would seem to confirm our proposal for
therapy, but further studies with a wider range of cases would be needed to
confirm the goodness of our results.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- International Journal of Diabetes (ISSN: 2644-3031)