2562
Views & Citations1562
Likes & Shares
We report a case of a young patient with keratoconus, whose left eye
presented with high myopia astigmatism (-2.25 -8.5 × 100) following penetrating
keratoplasty. Femtosecond laser assisted arcuate keratotomy (FLAK) was
performed and the patient’s astigmatism was significantly reduced after the
procedure. However, the visual acuity was still limited by residual myopia
astigmatism (-8.00 -3.75 × 110). A Toric implantable collamer lens (TICL) was
used to this condition. The refraction after implantation improved to -0.50
-0.75 × 65 with an uncorrected distance visual acuity (UDVA) of 20/25 and a
corrected distance visual acuity (CDVA) of 20/20. The combination of TICL
implantation and FLAK is a candidate for correcting residual myopia astigmatism
following PKP.
INTRODUCTION
Arcuate keratotomy (AK) is a procedure which
has been widely used in correction of astigmatism after penetrating
keratoplasty (PKP) [1,2]. However, AK has certain limitations such as low
reproducibility and tendency to undercorrect [3,4]. Despite that the
application of femtosecond laser in AK has improved its
accuracy, this procedure is still not effective enough, as evidenced by the
frequent occurrences of residual astigmatism or/and myopia [5,6]. Nonsurgical
therapies such as spectacles and contact lenses are not always effective in
correcting these residual refractive errors, because spectacles correction is
unsuitable for high level of anisometropia, and the use of contact lenses is
dependent on lens tolerance of patients. Laser in situ keratomileusis (LASIK)
and photorefractive keratectomy (PRK) are common procedures for correcting
these residual refractive errors are limited by the thickness of graft and
therefore, are not appropriate in ameliorating high level of residual
refractive errors after AK. Here, we present a case of high myopia
astigmatism post-PKP, which was not completely corrected by femtosecond
laser-assisted arcuate keratotomy (FLAK) alone, but was properly corrected by a
combined therapy of FLAK and Toric implantable collamer lens (TICL
implantation).
CASE REPORT
The patient was a 23-year-old man
who had received PKP in his left eye. Three months after suture removal, the
vision in his left eye could not be improved to a satisfying level due to high
residual myopia astigmatism (Table 1).
Regarding his right eye, the manifest refraction was -0.75 -0.75×60. The UDVA
was 20/20. The examination of intraocular pressure (IOP), crystalline lens and
retina was normal. AK was implemented under topical anesthesia with INTRALASE
FS SYSTEM (Advanced Medical Optics) after receiving patient’s informed consent.
The length and location of the arcuate incisions were determined based on the
borders of the steep semi-meridians, which were identified by corneal
topography [1] Parameter settings including posterior depth (469 µm,
80% depth of the thinnest corneal thickness), anterior diameter (6.0 mm),
anterior energy (1.5 µJ), cut position 1 (35 degree), cut angle 1 (70 degree),
cut position 2 (175 degree), cut angle 2 (90 degree), anterior side cut angle
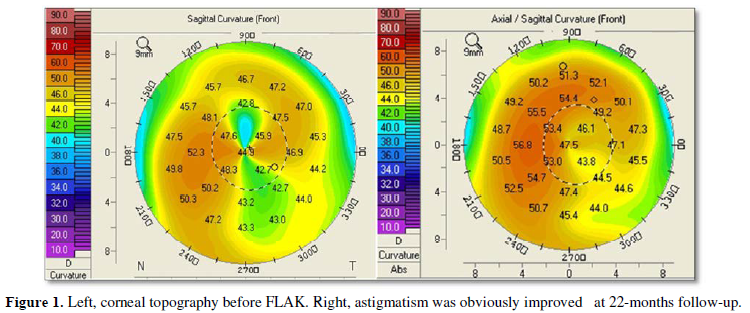
(120 degree) and anterior side cut spot separation (3μm). The astigmatism was obviously reduced (Figure 1), but with high residual
myopia astigmatism remained (Table 1)
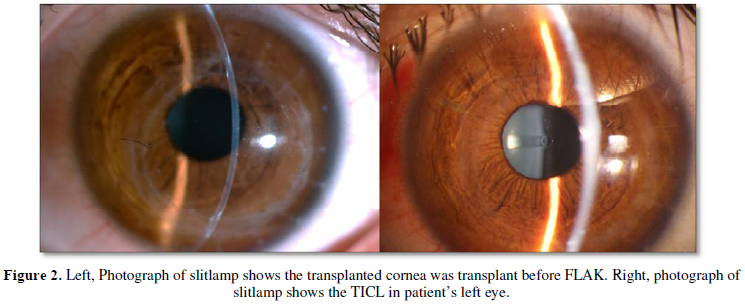
22 months after FLAK. Therefore, a TICL was implanted after another informed
consent was signed. Preoperative examinations established the following
parameters: corneal topography (50.7@25/47.0@115), anterior
chamber depth (3.69 mm), white-to-white distance (11.5 mm), manifest refraction
(-8.00 -3.75×110), IOP (11 mmHg) and endothelial cells density (ECD, 2196/mm2).
A final
TICL (VTICMO 13.2 mm, -13.5 +4.0×023, STAAR surgical) was determined by the
software provided
by manufacturer
and it was implanted into the left eye of the patient under topical anesthesia
(Figure 2).
The
manifest refraction, UCVA and CDVA showed obvious improvements 3 months after
TICL implantation compared with those before the procedure (Table 1). These significant
improvements of his vision and refractive error were sustained at the 6-month
follow-up. In addition, the ECD was 2106/mm2 with a loss rate of
4.1% at 3-month follow-up and 2055/mm2 with a loss rate of 6.4% at
6-month follow-up. No intraoperative or postoperative complications were
observed at the follow-ups.
DISCUSSION
AK was considered as an effective way to reduce the high level of
astigmatism after PKP [1,2]. In this study, we observed a reduction of
refractive cylinder of 55.9%, which was consistent with previous reports
[1,7-9]. The reduction of keratometric cylinder was 57%, which was also similar
to those seen in other studies [7,8]. However, neither the UDVA nor the CDVA
improved evidently (Table 1). It is
worth noting that we observed an obvious myopia shift of spherical equivalent
(SE) at 3-month follow-up. This trend of myopic shift development after AK was
probably associated with the increase in central corneal curvature, which
occurred due to the release of axial tension within the graft and a concomitant
increase in the corneal vault. Another possible reason of this process was two
large arcuate incisions (70 degree and 90 degree) performed on graft, which
dramatically weakened the mechanical strength of graft and resulted in ectasia.
Fortunately, this process stopped, and the topography and refraction were
stable at the subsequent follow-ups.
Although there was a significant reduction in astigmatism after FLAK,
the residual myopia astigmatism (-8.00 -3.75×110) was so high that the
patient’s vision was still unsatisfactory, which was too high for refractive
surgery to be safe. Severe anisometropia rendered spectacle correction
infeasible, and the patient was intolerant of long-term use of contact lenses.
We therefore performed TICL implantation to improve the results of FLAK. TICL
implantation has been reported as a potential procedure for correcting myopia
and astigmatism after PKP and anterior lamellar keratoplasty [10-12]. However,
to our knowledge, the management of TICL implantation to correct high residual
refractive errors after FLAK has not been reported.
The manifest refraction and visual acuity showed significant
improvements and reached satisfactory levels after the surgery (Table 1). A low rate of ECD loss (6.4%
at 6 months) similar to that reported by a previous study (5.11% at 6 months)
[7] was observed in our case. No cataract, opacification and IOP elevation were
observed during 6-month follow-up. However, Fernandes et al. [13]
reported that 5.2% of eyes developed cataract after ICL implantation during at
least 3-year follow-up. So we need to perform longer follow-ups to estimate the
long-term safety of this treatment.
Although AK can effectively reduce severe astigmatism after PKP, the
predictability of AK remains unsatisfactory and secondary treatments are
usually inevitable. TICL implantation not only can accurately correct residual
myopia astigmatism, especially high residual myopia astigmatism after AK, which
is unsuitable to perform LASIK or PRK. It may also be a safer option than LASIK
and PRK, which might be responsible for complications such as iatrogenic
corneal ectasia [14] and the increased risk of graft rejection. Therefore, in
our opinion, combining TICL implantation with FLAK is a candidate for the
correction of high residual myopia astigmatism after PKP. The effectiveness,
safety and predictability of this procedure are worthy of further studies.
ACKNOWLEDGEMENTS
Disclosure: Neither author has a financial or proprietary interest in
any material or method mentioned.
Funding: No funding
Additional contributions: No additional contribution.
- Nubile M, Carpineto P,
Lanzini M, et al. (2009) Femtosecond laser arcuate keratotomy for the
correction of high astigmatism after keratoplasty. Ophthalmol 116: 1083-1092.
- Viswanathan D, Kumar NL
(2013) Bilateral femtosecond laser-enabled intrastromal astigmatic keratotomy
to correct high post-penetrating keratoplasty astigmatism. J Cataract Refract Surg 39:
1916-1920.
- Buzzonetti L, Petrocelli G,
Laborante A, et al. (2009) Arcuate keratotomy for high postoperative
keratoplasty astigmatism performed with the intralase femtosecond laser. J Refract Surg 25: 709-714.
- Bayramlar H, Karadag R,
Cakici O, et al. (2016) Arcuate keratotomy on post-keratoplasty
astigmatism is unpredictable and frequently needs repeat procedures to
increase its success rate. Br J Ophthalmol 100: 757-761.
- Fadlallah A, Mehanna C,
Saragoussi JJ, et al. (2015) Safety and efficacy of femtosecond
laser-assisted arcuate keratotomy to treat irregular astigmatism after
penetrating keratoplasty. J Cataract Refract Surg 41: 1168-1175.
- Loriaut P, Borderie VM, Laroche
L (2015) Femtosecond-Assisted Arcuate Keratotomy for the Correction of
Postkeratoplasty Astigmatism: Vector Analysis and Accuracy of Laser
Incisions. Cornea 34: 1063-1066.
- Cleary C, Tang M, Ahmed H, et
al. (2013) Beveled femtosecond laser astigmatic keratotomy for the
treatment of high astigmatism post-penetrating keratoplasty. Cornea 32: 54-62.
- Hoffart L, Proust H, Matonti
F, et al. (2009) Correction of postkeratoplasty astigmatism by femtosecond
laser compared with mechanized astigmatic keratotomy. Am J Ophthalmol 147: 779-787.
- Wetterstrand O, Holopainen
JM, Krootila K (2013) Treatment of postoperative keratoplasty astigmatism
using femtosecond laser-assisted intrastromal relaxing incisions. J Refract Surg 29: 378-382.
- Akcay L, Kaplan AT, Kandemir B,
et al. (2009) Toric intraocular Collamer lens for high myopic astigmatism
after penetrating keratoplasty. J
Cataract Refract Surg 35: 2161-2163.
- Alfonso JF, Lisa C,
Abdelhamid A, et al. (2009) Posterior chamber phakic intraocular lenses
after penetrating keratoplasty. J
Cataract Refract Surg 35: 1166-1173.
- Qin Q, Yang L, He Z, et al.
(2017) Clinical application of TICL implantation for ametropia following
deep anterior lamellar keratoplasty for keratoconus: A CONSORT-compliant
article. Medicine 96: e6118.
- Fernandes P, Gonzalez-Meijome
JM, Madrid-Costa D, et al. (2011) Implantable collamer posterior chamber
intraocular lenses: a review of potential
complications. J Refract
Surg 27: 765-776.
- Ghanem RC, Ghanem MA, Bogoni
A, Ghanem VC (2013) Corneal ectasia secondary to LASIK after arcuate
keratotomy. J Refract Surg
29: 426-429.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Oncology Clinics and Research (ISSN: 2643-055X)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- International Journal of AIDS (ISSN: 2644-3023)