2673
Views & Citations1673
Likes & Shares
Central serous retinopathy is one of the
relatively common clinical conditions, it is an idiopathic disorder
characterized by a localized serous detachment of the sensory retina at the
macula due to leakage from the choriocapillaris through focal or diffuse
retinal pigment epithelial defects. It usually affects the middle age group.
Risk factors include type A personality, use of systemic steroids, stress,
pregnancy and autoimmune diseases. The acute course of the disease (ACSR)
usually spontaneously resolves within 3-6 months in 80% of cases,while the
chronic course(CSCR) lasts more than 12months. Multimodal new imaging
techniques like Swept Source OCT (SS-OCT), FAF (fundus auto fluorescence), FA
(fluorescein angiography) & ICG (indocyanine green) are necessary to
diagnose atypical cases of CSCR that may be misdiagnosed as inflammatory
sensory detachments leading to inappropriate treatment and visual loss.
Keywords:
Central serous retinopathy,
Multimodal imaging, Choroiditis, Posterior uveitis
INTRODUCTION
Central serous
chorioretinopathy (CSR) is the fourth most common vision threatening retinopathy
after age related macular degeneration, diabetic retinopathy and retinal
vascular diseases [1]. It is defined as serous retinal detachment most often in
the macula, with or without pigment epithelial detachment (PED) [2]. The
clinical presentation includes blurring of vision, metamorphopsia, reduced
contrast sensitivity and dyschromatopsia [3].
Atypical and
chronic CSCR may be misdiagnosed as chorio-retinal inflammatory conditions
leading to inappropriate treatment. This usually leads to worsening of CSCR
with irreversible retinal damage and visual impairment.
In our case, we
use multimodal retinal imaging for the diagnosis of a case of atypical
bilateral CSCR which was treated previously as posterior uveitis.
CASE REPORT
A 45-year old male, medically free, presented with decreased vision
in both eyes of 8-month duration starting in the right eye (RE) and later
involving the left eye (LE) in the following six months.
The patient was diagnosed initially as a case of idiopathic
bilateral posterior uveitis (multifocal choroditis, harada, serpiginous
choroiditis, etc) based on negative work up for infectious and non-infectious
uveitis and on OCT (optical coherence tomography) which showed bilateral
multifocal areas of neurosensory detachment with sub-foveal turbid fluid and
thick choroid.
The patient was treated with several courses of oral steroids and
one intravitreal triamcinolone injection in the right eye with no improvement.
On examination, his best corrected visual acuity (BCVA) was 20/100
in the right eye (RE) and 20/40 in the left eye (LE). Anterior segment
examination was negative with no signs of anterior uveitis.
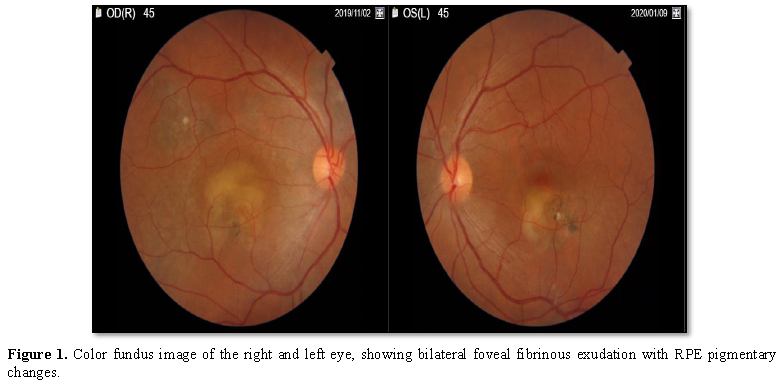
Dilated fundus exam of both eyes showed bilateral normal optic
discs, bilateral sub-foveal yellowish fibrin deposition with areas of retinal
pigmentary epithelial changes. The vitreous in both eyes was clear with no
signs of vitritis (Figure 1). DRI
Triton (TOPCON, Tokyo, Japan) multimodal imaging camera was used to evaluate
the case.
The Triton Swept Source OCT technology using 1050 nm light enables
better tissue penetration and clear image of the vitreous, retina and choroid
in a single capture.
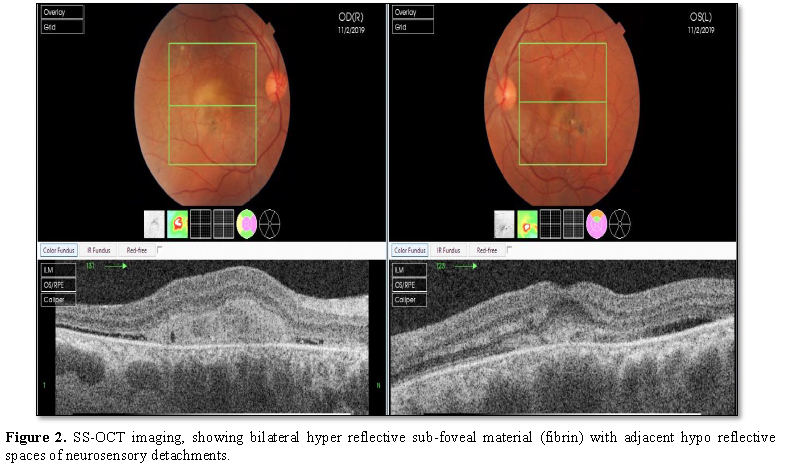
Swept Source Optical Coherence Tomography (SS-OCT) images showed bilateral sub-foveal hyperreflective fibrin deposition with adjacent areas of shallow hypo reflective sub retinal fluid and foci of (RPE) retinal pigment epithelial detachment (Figure 2).
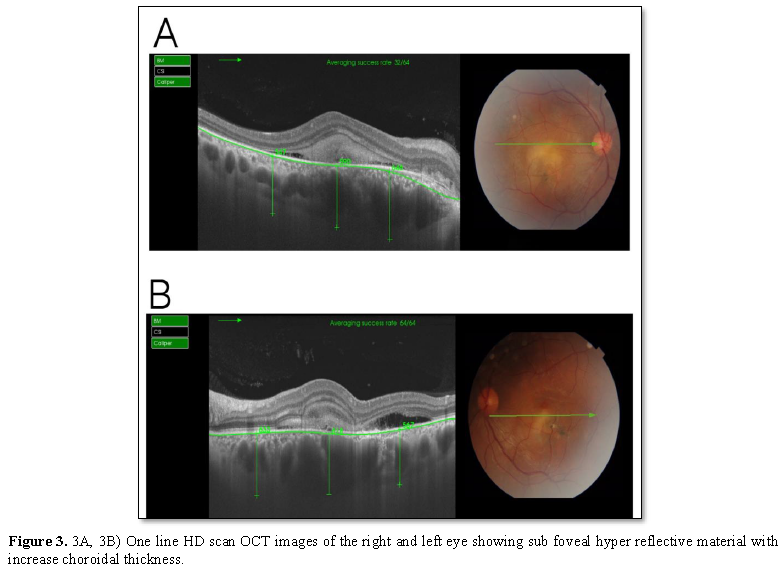
We evaluated the choroidal thickness by using a line scan mode in
DRI SS-OCT that generates a B scan image computed from 96 scans for the same
line to give a high definition image of the vitreous, retina and choroid.
One-line SS-OCT B scan images showed an increase in the choroidal
thickness in both eyes, which was [590 μm ± 50] (Figure 3A) in the right eye and [618 μm ± 50] in the left eye (Figure 3B).
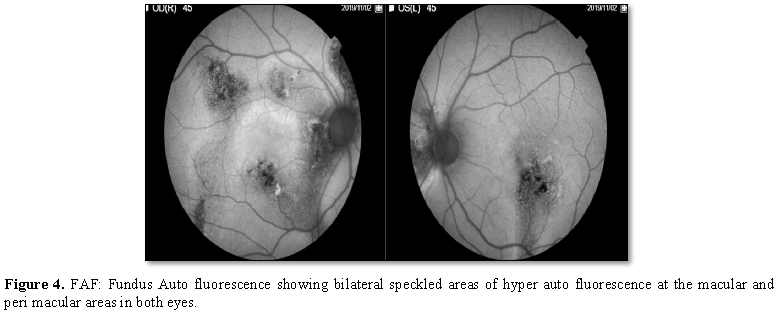
Fundus
Auto fluorescence (FAF)
showed bilateral speckled areas of hyper auto fluorescence as shown in Figure 4.
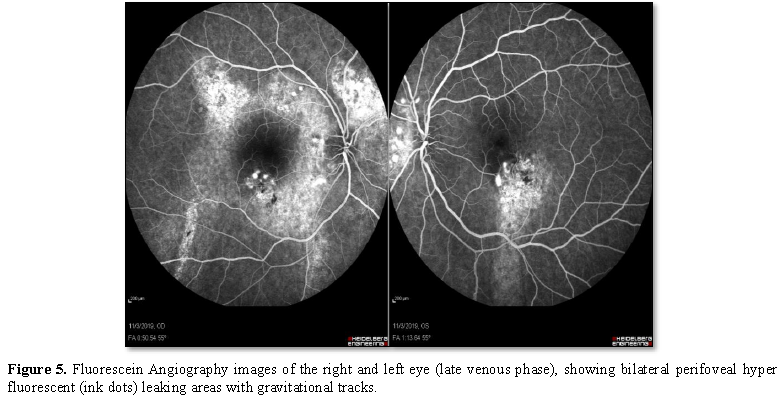
Fluorescein angiography (FA)
revealed bilateral perifoveal multifocal pinpoint hyperfluorescent leakage
areas with a classical “gravitational tract” (Figure 5).
Indocyanine green angiography was not included, because the dye is
not registered in Jordan. Based on FAF and FA findings, the case was diagnosed
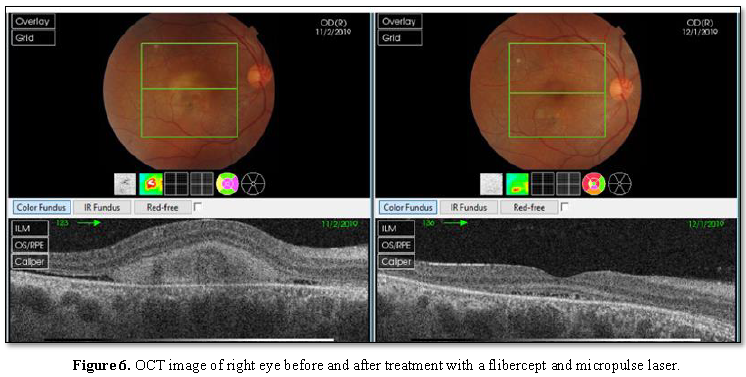
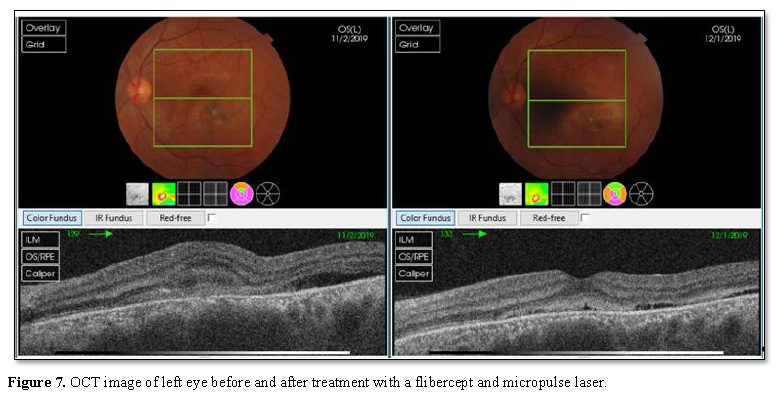
as chronic CSR, the corticosteroids were stopped. As photodynamic therapy was
not available in our clinic, a single intravitreal injection of aflibercept was
performed in the both eyes [4] followed 4 weeks later by 577 nm yellow
micropulse laser treatment which was applied to the active focal RPE leaking
areas on FA [5]. One month later, BCVA in the right eye improved from 20/100 to
20/30 and in the left eye from 20/40
to 20/25 with improvement in the foveal anatomy on OCT (Figure 6 and 7).
DISCUSSION
Atypical cases of CSCR may represent a
diagnostic challenge. Such cases may be misdiagnosed as posterior uveitis like
multifocal choroiditis, Vogt Koyanagi Harada, posterior scleritis---etc. The
dependence on one image modality like (OCT) to diagnose such cases is
inappropriate.
The use of systemic or intraocular steroids
in these cases is not only ineffective, but it may lead to worsening of CSCR
and severe drop of vision [6].
A transient increase in choroidal thickness
is associated with acute posterior uveitis like multifocal choroiditis, VKH and
white dot syndrome, this entity often occurs in eyes with CSCR and is called
pachychoroid [7,8].
The increase in the choroidal thickness in
our case of CSCR is a part of the pathophysiology of this disease which
includes choroidal congestion and hyperpermeability as well [9] and this
sometimes represents a diagnostic dilemma especially with the other cases of
posterior uveitis which manifest similarly with increase in choroidal
thickness.
The use of multimodal imaging OCT, FA, FAF
can provide us clues for correct approach and diagnosis, the speckled hyper
auto fluorescence on FAF and gravitational zones on FA were helpful for us to
reach to the correct diagnosis and treatment.
CONCLUSION
Atypical cases of CSCR need a careful
approach and good analysis. The use of multimodal imaging is the best way to
differentiate CSCR from other chorioretinal inflammatory cases to avoid visual
loss resulting from misdiagnosis or mismanagement.
1. Wang M, Munch IC, Hasler PW, Prunte C,
Larsen M (2008) Central serous retinopathy. Acta Ophthalmol 86: 126-145.
2. Liegl R, Ulbig MW (2014) Central serous retinopathy.
Ophthalmologica 232: 65-76.
3. Schachat AP (2018) Ryan’s Retina.
Elsevier.
4. Padrón-Pérez N, Arias L, Rubio M,
Lorenzo D, García-Bru P, et al. (2018) Changes in the choroidal thickness after
intravitreal injection of Anti-vascular endothelial growth factor in
Pachychoroid Neovasculopathy. Invest Ophthalmol Vis Sci 59: 1119-1124.
5. Yadav NK, Jayadev C, Mohan A, Vijayan P,
Battu R, et al. (2015) Subthreshold micro pulse yellow laser (577 nm) in
chronic central serous chorioretinopathy: Safety profile and treatment outcome.
Eye (Lond) 29: 258-264.
6. Khairallah M, Kahloun R, Tugal-Tutkun I
(2012) Central serous chorioretinopathy, corticosteroids and uveitis. Ocul
Immunol Inflamm 20: 76-85.
7. Maruko I, Lida T, Sugano Y, Oyamada H,
Sekiryu T, et al. (2011) Subfoveal choroidal thickness after treatment of
Vogt-Koyanagi-Harada disease. Retina 31: 510-517.
8. Lehmann M, Bousquet E, Beydoun T, Behar-Cohen
F (2014) PACHYCHOROID: An Inherited condition? Retina 35: 10-16.
9. Gass JD (1967) Pathogenesis of disciform
detachment of neuroepithelium. Am J Ophthalmol 63: 1-139.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Spine Diseases
- Journal of Renal Transplantation Science (ISSN:2640-0847)