Review Article
Accuracy of Khine Formula in Prediction of Cuffed Tracheal Tube Size in Turkish Children
3425
Views & Citations2425
Likes & Shares
Background: There exists various physical indices formulas to select the appropriate size of endotracheal tube (ETT) for pediatric patients. To our knowledge, no study exists examining the accuracy of any of these formulas in Turkish children. This study aimed to investigate the homogeneity and accordance of commonly used Khine formula for size with the applied Turkish pediatric population.
Methods: One hundred and twenty-five patients from 2 to 12 years of age, undergoing general anesthesia were enrolled into the study. We recorded demographic data. The used endotracheal tube sizes together with the calculated ones were noted. Air leak test was performed for validation of the size of the used tube.
Results: In this study, we examined a total of 125 children, with a mean age of 6,6 ± 3,1 (min: 2 - max: 12) years and a mean body mass index (BMI) of 17,1 ±2,9 kg.m-2. The size of the tube calculated by Khine formula was compatible with Turkish children’s tracheal size in %96 crudely. A strong intraclass correlation (0.992) was found between Khine formula-based tube diameter and the used ones.
Conclusion: Our findings support the practice of routinely selecting a cuffed endotracheal tube size based on Khine formula for Turkish children.
Keywords: Khine formula, Cuffed endotracheal tube, Turkish
The clinical study's registration number is: 23.12.2015-250 received from the Ethics Committee of Yıldırım Beyazıt University Medical Faculty.
INTRODUCTION
Selection of an appropriate endotracheal tube (ETT) is very important in intraoperative settings and critical care. Increased risk of airway trauma caused by either under or oversized ETT’s makes tube size selection quite crucial, especially in pediatric anesthesia procedures [1]. In the estimation of the appropriate size ETT, there exists various formulas based on factors, such as the patient’s age, sex, body mass index (BMI), and the purpose and duration of intubation. However, there are some conflicts about the compatibility of these formulas especially in young ages, as obvious variations in physical development and tracheal dimensions exist.
In 1997, Khine [2] reported the favorable advantages of their formula against Cole et al. for selecting cuffed ETT (cETT) [2]. Recently, cETTs have been popular again, as a result of acceptance of changes in the pediatric airway from conical or circular to elliptical shape [3]. Despite these developments, the role of ethnicity in these measurements, is still unknown. Mostly, methods developed according to the observations and experiences in Caucasian populations guide the selection of the tubes [4]. In one of the recent studies, however, the authors couldn’t support the perception of requirement of a smaller sized ETT in Chinese adults, in contrary to what is expected [4,5]. Nevertheless, there has been no comprehensive study interpreting accuracy of any of the formulas in the aspect of ethnicity in pediatric patients.
Thus, we aimed to evaluate the accordance of age-based Khine formula in a small Turkish pediatric population for cETT size estimation.
MATERIALS AND METHODS
After obtaining institutional ethical committee approval, and written informed consent of parents, children (ASA I-II) aged between 2-12 years who received general anesthesia at Atatürk Training and Research Hospital were enrolled in this study. Based on a study by Duracher [6], a sample size of 109 patients was calculated to achieve 80% power [6]. Thus, we selected a sample size of 125 participants in this study.
The patients with an ASA score >3, requirement of prolonged mechanical ventilation, anticipated difficult airway, growth retardation, or preexisting laryngeal/pharyngeal pathology were excluded.
All patients were premedicated with oral midazolam of 0.5 mg.kg-1, and standard monitoring (EKG, SpO2, noninvasive arterial pressure) was applied. General anesthesia was induced by intravenous propofol 2-3 mg.kg-1, and remifentanil 1µg.kg-1, and rocuronium bromide 0.6 mg.kg-1 was administered to facilitate mask ventilation and intubation. The maintenance of anesthesia was provided by inhalation of sevoflurane at 2-2.5% in O2/N2O (50/50%) mixture.
The trachea was intubated by a cETT (Bıçakcılar®, Türkiye), whose size was calculated based on the Khine formula (size of cETT: Age/4 + 3). The calculated size was rounded to the nearest 0.5 mm. Following intubation, cuff pressure was monitored by cuff pressure manometer (Mallinckrodt, Germany). If an airway pressure >25 cmH20 was required to detect an audible leak, the endotracheal tube was replaced by another tube with a 0.5 mm smaller size. If there was an audible leak at airway pressure 2O, the tube was changed by 0.5 mm larger one. The need for endotracheal tube replacement and peak airway pressures were recorded.
Mechanical ventilation was initiated with 10 mL. kg-1 tidal volume and a frequency to keep ETCO2 between 34 and 38 mmHg. The need for ETT replacement was recorded. For standardization, air leak test was done in the supine position with the head in the neutral position, in each patient. At the end of the operation, the patients were extubated with atropine 0.5 mg and neostigmine 0.03 mg.kg-1 injected intravenously to reverse the muscle relaxation. Afterwards, they were transported to post anesthesia care unit for further observation.
STATISTICAL ANALYSIS
Data analysis was performed using IBM SPSS Statistics version 17.0 software (IBM Corporation, Armonk, NY, USA). Descriptive statistics for continuous variables were expressed as mean ± SD. Categorical data were shown as number of cases with (%). Bland-Altman plot analysis was applied for determining the agreement levels between expected and observed endotracheal tube sizes. Mean differences (bias), lower and upper limits of agreement were also calculated. Whether the mean bias levels differ from reference value of zero was evaluated One-sample t-test. Intraclass correlation coefficients (ICC) and 95% confidence intervals (CI) was also calculated to determine the agreement levels between expected and used endotracheal tube sizes. p
RESULTS
Demographic data and surgical interventions performed in 125 children are presented in Table 1. Among the children aged 2-12 years (mean 6,6 ± 3,1 years), 65 were male and 60 were female. The mean weight and height of the children were 24,9 ± 10,9 kg, and 118,4 ± 19,8 respectively. Originally inserted tube size was the same as calculated by Khine formula in 96 % of children. According to the current results, the intraclass correlation coefficient (ICC) level for the calculated and used endotracheal tube sizes is 0.992 (95% CI: 0.988 – 0.994), and it can be noted that these measurements are almost one-on-one compatible.
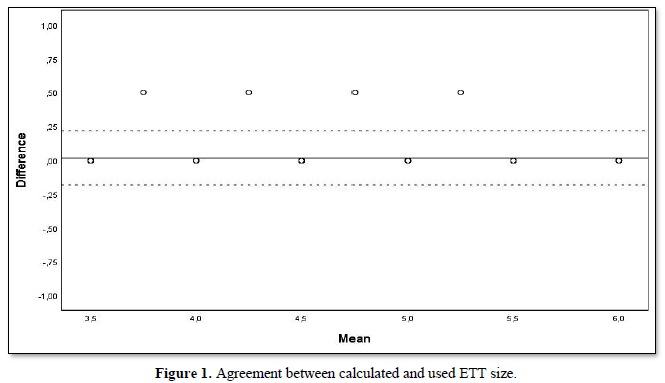
In 5 children where the size of the tube used was not compatible with the size calculated, the tube was replaced to a 0.5 mm larger tube (Figure 1). In three of these children, stridor was observed at 0-2 h postoperatively. Among the rest, only two children experienced throat pain.
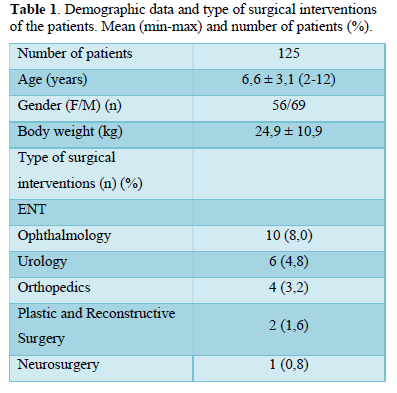
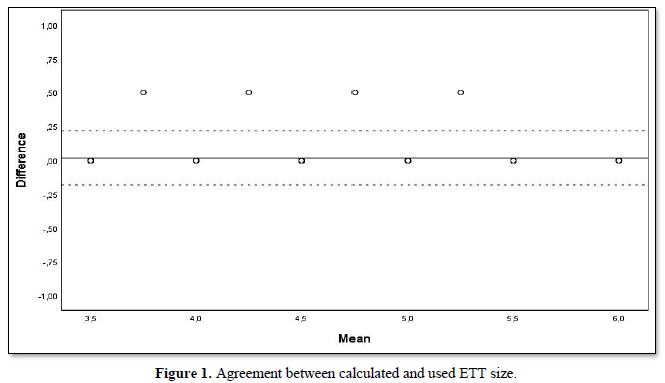
Figure 1 is a Bland-Altman diagram showing the magnitude of the difference between expected endotracheal tube (ETT) size and observed (surgical) tube sizes [n=125, mean bias=0.020 mm (solid line); SD=0.0984]. The dashed lines represent the lower and, upper limits of agreement: LoA=-0.173 mm and, UoA=0.213 mm; respectively.
DISCUSSION
In the present study, for the first time to our knowledge, we lightened the accuracy of Khine formula in selection of appropriately-sized cETT in Turkish children. This age-based formula for cETT was an adequate guide for prediction of optimal size in this population. Our goal in conducting this study was to investigate the role of racial differences in anesthesia applications and draw attention to this issue.
Recently, ETTs with a thin, high-volume, low-pressure polyurethane cuff increased the popular use of cETTs in children. Khine formula is frequently used for determining the correct tube size. However; many factors such as structural variations, disproportionate spread of age and body weight in children, lead to discrepancy in predicting the optimum ETT diameter [7-9]. Thus, different factors influencing the recommendations have been investigated. Naina [10] emphasized the importance of collection of data from different populations to support the absence of racial variations in tracheal dimensions, since the role of ethnic phenotype in correct choice of ETT remains unknown [10]. Tai [11] reported that most of the results were obtained from the Western populations [11]. The author mentioned about the perception of requirement of smaller diameter ETT in Chinese patients, due to altered body build and also systematic craniofacial differences detected in patients with sleep apnea. However, he showed that tracheal diameters of adult Chinese and Caucasian populations weren’t clinically different from each other. According to Tai [11], age wasn’t a predictive factor in tracheal diameter in adults S15). Both Coordes [12] and Brodsky [13] also reported that, age in adults didn’t influence tracheal diameter, in two different studies S15-10,16). In a small, healthy Japanese population, Sakai [14] couldn’t report a significant effect of age in tracheal sizes analyzed by computed tomography (CT) after adjusting the other factors [14]. However, in another study, CT detected changes were shown in cross-sectional areas of tracheas in 0-20 years of age range [15].
Actually; gender and body surface area (BSA) have been suggested to influence the sizes in body build. Namely, height showed a good correlation with ETT size, in Asian infants and children [16].
Unfortunately, the number of studies conducted in Turkish children is very limited. Gollu [17], demonstrated a significant difference between ultrasound measured tracheal diameter and anesthesiologist predicted tube size and age-based formulas. They advised to confirm the ETT size by ultrasound as an objective technique [17]. In another Turkish study, the authors compared cETT sizes selected by age-based formulas or with ultrasound measurements. Similar to Gollu [17], they demonstrated a significant difference in favor of ultrasound [18]. A study comparing age and height-based formulas with ultrasound, demonstrated high predictive effect of ultrasound in different age groups of children [19]. Both Altun [18] and Shibasaki [1], demonstrated that age-based formulas resulted in larger diameter tubes. Gupta [20] suggested that the size of ETT predetermined by ultrasound showed high correlation to clinically used ETT in comparison to ETT predicted by age-based formula, but in their study, the ETT used wasn’t specified in the aspect of cuff. Stugatti [21], showed a comparable correlation by Khine’s formula and ultrasound for cuffed ETT [21]. Furthermore, other studies derive an appropriate tube size by ultrasound at rates ranging between 47% and 77% [22]. This wide range of appropriateness might be due to different age groups and either cuffed or uncuffed tubes used in the studies. Ultrasound, MRI or CT aren’t always easily applicable methods and all require training and skill of the physician [23]. That’s why most of the anesthesiologists commonly use age-based formulas, as it is considered as an objective solution [20,22]. This requires well experience, as in our study, all intubations were performed by an anesthesiologist with at least 5 years of experience. Thus, originally inserted tube sizes were fit with Khine formula in 96 % of children in our population. Also, we didn’t experience a significant intraoperative or early postoperative airway complication. Apparently, there are several reports describing complications related to inappropriately chosen ETT [1,19,20,24].
The study had limitations. We didn’t include newborn and infants in the study. The results might have been evaluated by stratification of age groups. Secondly, all the patients were from one hospital in Ankara. For more accurate opinions about ethnicity, data from different centers and cities should have been collected. Also sample size was small to interpret the results to all population.
Nevertheless, our final report supports that Khine formula is accurate for Turkish children, when performed by an experienced clinician. However, ethnic influence in this area must be resolved by further studies.
- Shibasaki M, Nakajima Y, Ishii S, Shimizu F, Shime N, et al. (2010) Prediction of pediatric endotracheal tube size by Ultrasonography. Anesthesiology 113: 819-824.
- Khine HH, Corddry DH, Kettrick RG (1997) Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia. Anesthesiology 86: 627-631.
- Tobias JD (2015) Pediatric airway anatomy may not be what we thought: implications for clinical practice and the use of cuffed endotracheal tubes. Paediatr Anaesth 25: 9-19.
- Lee RW, Vasudavan S, Hui DS, Prvan T, Petocz P, et al. (2010) Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep 33: 1075-1080.
- Sutherland K, Lee RW, Cistulli PA (2012) Obesity and craniofacial structure as risk factors for obstructive sleep apnea: Impact of ethnicity. Respirology 17: 213-222.
- Duracher C, Schmautz E, Martinon C, Faivre J, Carli P, et al. (2008) Evaluation of cuffed tracheal tube size predicted using the Khine formula in children. Paediatr Anaesth 18: 113-118.
- Furuya A, Nomura H, Kuroiwa G, Tamaki F, Suzuki S, et al. (2009) Endotracheal tube selection in children: Which is the better predictor for the selection, tracheal internal diameter in X-ray photograph or age-based formula? Masui 58: 724-727.
- Al-Mazrou KA, Abdullah KM, Ansari RA, Abdelmeguid ME, Turkistani A (2009) Comparison of the outer diameter of the 'best-fit' endotracheal tube with MRI-measured airway diameter at the cricoid level. Eur J Anaesthesiol 26: 736-739.
- De Orange FA, Andrade RG, Lemos A, Borges PS, Figueiroa JN, et al. (2017) Cuffed versus uncuffed endotracheal tubes for general anesthesia in children aged eight years and under. Cochrane Database Syst Rev 11: CD011954.
- Naina P, Syed KA, Irodi A, John M, Varghese AM (2020) Pediatric tracheal dimensions on computed tomography and its correlation with tracheostomy tube sizes. Laryngoscope 130: 1316-1321.
- Tai A, Corke C, Joynt GM, Griffith J, Lunn D, et al. (2016) A comparative study of tracheal diameter in Caucasian and Chinese patients. Anaesth Intensive Care 44: 719-723.
- Coordes A, Rademacher G, Knopke S, Todt I, Ernst A, et al. (2011) Selection and placement of oral ventilation tubes based on tracheal morphometry. Laryngoscope 121: 1225-1230.
- Brodsky JB, Macario A, Mark JB (1996) Tracheal diameter predicts double-lumen tube size: a method for selecting left double lumen tubes. Anesth Analg 82: 861-864.
- Sakai H, Nakano Y, Muro S, Hirai T, Takubo Y, et al. (2010) Age related changes in the trachea in healthy adults. Adv Exp Med Biol 662: 115-120.
- Effmann EL, Fram EK, Vock P, Kirks DR (1983) Tracheal cross-sectional area in children: CT determination. Radiology 149: 137-140.
- Wang TK, Wu RS, Chen C, Chang TC, Hseih FS, et al. (1997) Endotracheal tube size selection guidelines for Chinese children: Prospective study of 533 cases. J Formos Med Assoc 96: 325-329.
- Gollu G, Bermede OA, Khanmammadov F, Ates U, Genc S, et al. (2018) Use of ultrasonography as a noninvasive decisive tool to determine the accurate endotracheal tube size in anesthetized children. Arch Argent Pediatr 116: 172-178.
- Altun D, Sungur MO, Ali A, Seyhan TO, Sivrikoz N, et al. (2017) The role of ultrasound in appropriate endotracheal tube size selection in pediatric patients. Paediatr Anaesth 27: 1015-1020.
- Bae JY, Byon HJ, Han SS, Kim S, Kim JT (2011) Usefulness of ultrasound for selecting a correctly sized uncuffed tracheal tube for pediatric patients. Anaesthesia 66: 994-998.
- Gupta K, Gupta PK, Rastogi B, Krishan A, Jain M, et al. (2012) Assessment of the subglottic region by ultrasonography for estimation of appropriate size endotracheal tube: A clinical prospective study. Anesth Essays Res 6: 157-160.
- Stugatti JG, Raja R, Kurdi MS (2017) Ultrasonographic estimation of endotracheal tube size in pediatric patients and its comparison with physical indices-based formulae: A prospective study. J Clin Diagn Res 11: UC05-UC08.
- Schramm C, Knop J, Jensen K, Plaschke K (2012) Role of ultrasound compared to age- related formulas for uncuffed endotracheal intubation in a pediatric population. Paediatr Anaesth 22: 781-786.
- Lakhal K, Delplace X, Cottier JP (2007) The feasibility of ultrasound to assess subglottic diameter. Anesth Analg 104: 611-614.
- Murat I (2001) Cuffed tubes in children: A 3-year experience in a single institution. Paediatr Anaesth 11: 748-749.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Alcoholism Clinical Research
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- International Journal of AIDS (ISSN: 2644-3023)