3698
Views & Citations2698
Likes & Shares
Granulocytic sarcoma (GS) or what are called chloroma, myeloblastoma and myeloid sarcoma isan uncommon extramedullary solid tumor of immature myeloid cells. It occurs primarily in acute myelogenous leukemia (AML) but also may arise in patients with other myeloproliferative disorders.
It could occur at any part of the body mostly in the bone, soft tissue or lymph node, rarely involving the central nervous system (CNS) and causing spinal cord compression, it could occur during the course of disease, at relapsed or as isolated granulocytic sarcoma (IGS) without bone marrow involvement.
We report a 17-year-oldboy withIGS of the vertebral body causing spinal cord compression and bilateral lower limb weakness treated with surgical decompression, laminectomy and biopsy followed by chemo-irradiation and currently the he is on regular follow up.
Keywords:Granulocytic Sarcoma, Chloroma, Cord Compression, Acute Myeloid Leukemia
Abbreviations: T: Thoracic; L: Lumbar; MRI: Magnetic Resonance Imaging; CD: Cluster of Differentiation; IV: Intravenously
INTRODUCTION
Granulocytic Sarcoma is a rare extramedullary mass composed of immature myeloid cells most commonly found in association with acute myeloid leukemia (AML) [1]. The chloroma may be the initial manifestation of leukemia and can occur in different anatomic sites. MS is most commonly found in the orbit or periorbital and the diagnosis can be difficult especially when they precede the bone marrow involvement [2]. About 47% of MS are initially misdiagnosed mostly as malignant lymphoma but also as Ewing’s sarcoma, rhabdomyosarcoma and neuroblastoma.
It is a rare form (<1%) of extramedullary acute myeloid leukemia (AML) presenting without marrow involvement [3].We reported a case of isolated spinal GS which was successfully treated with decompression surgery, irradiation, and chemotherapywith intrathecal injection.
CASE REPORT
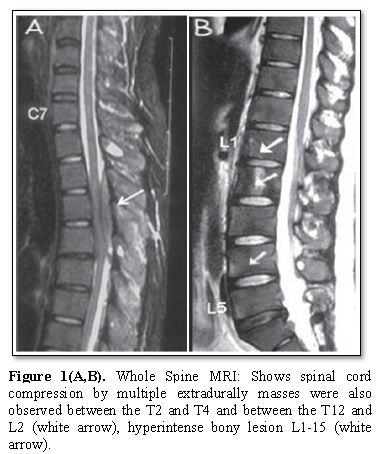
A 17 yearold adolescent boy was referred to us byneurosurgeon for further assessment and treatment.He was presented with localized severe back pain,asthenia in the legs and inability to walk for 12 days associated with numbness andparesthesia, no history of trauma to back. There is no consanguinity of parents, neither family history of malignancy nor similar condition, and high socioeconomic status, neither previous medical nor surgical problems. At presentation neurological examination revealed a 1/5 power in both legs, loss of pain and sensory perceptionbelow the T4 level, hyperactive deep tendon reflexes and positive Babinski reflex. There were neither other neurological abnormalities nor organomegaly. At causality MRI of the whole spine revealed hyperintense bonylesions on the L1-L5 vertebral bodies, spinal cord compression by multiple extradurallymasses were also observedbetween the T2 and T4, and between the T12 and L2 vertebral levels (Figure 1).
After starting him on Dexamethasone 8 mg intravenously four time daily, he was undergoing surgical decompression and open biopsy.
Post-operatively the patient was stable, oriented, afebrile, and well looking with normal vital signs.
Complete blood count revealedhemoglobin content was 12.7 g/dl, the platelet count was 350,000/ml, and a leukocyte count of 8,000/ml with 55% neutrophils, 44% lymphocytes, 1% monocytes, 0% eosinophils, and 0% basophils with normal blood film.
Bone marrow aspirate and biopsy werecellular without any other abnormalities;Cerebrospinal fluid cytology was negative, with normal Chest X-ray.
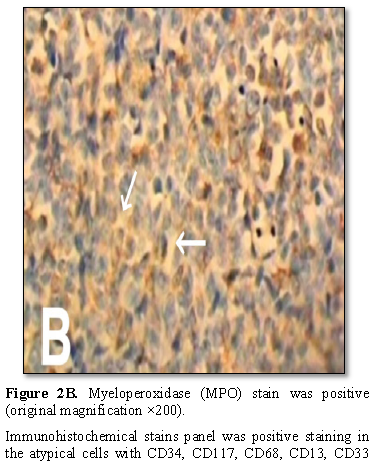
The histopathology evaluation of the mass revealed malignant cell infiltration with oval nuclei, eosinophilic cytoplasm by Hematoxylin‐eosin–stain. Tumor cells with eosinophilic cytoplasm are diffusely infiltrating the bone tissue (original magnification ×100) myeloperoxidase (MPO) stain was positive (Figures 2A and 2B).
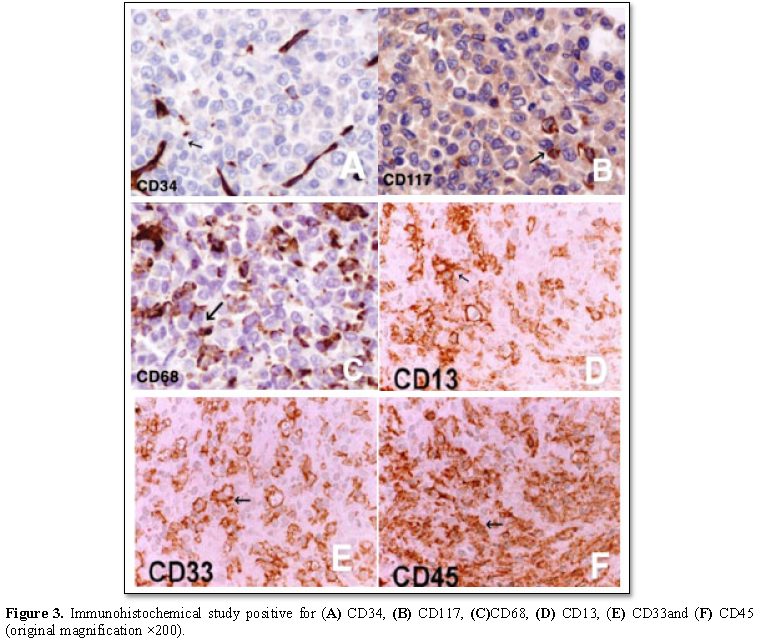
Immunohistochemical stains panel was positive staining in the atypical cells with CD34, CD117, CD68, CD13, CD33 and CD45 tested positive(Figure 3)and negative for CD20, CD79a, CD138, CD15, CD3 and CD5.
Based on normal bone marrow finding and Immunohistochemistry stains the diagnosis was isolated Granulocytic sarcoma of the spinal cord.
PET scan was not done because it was locally not available and radiotherapy was started urgently at a dose of 20 Gy, administered in 1.5-3.5 Gy fractions with systemic induction chemotherapy according to the MRC AML protocol consisted of daunorubicin 60 mg/day intravenous (i.v.) on days 1, 2 and 3and cytarabine (200 mg/day continuous i.v. on days 1-10 for 1 course, followed by daunorubicin 60 mg/day intravenous (i.v.) on days 1, 2 and 3 and Ara-C (200 mg/day continuous i.v. on days 1-8). The patient also received 2 intrathecal injections containing 15 mg hydrocortisone, 30 mg Ara-C and 15 mg methotrexate each time.
Clinically, the patient’s lower limbs motor power gradually improved with aggressive physiotherapy and was became 5/5; the patient started walking and sensory deficits disappeared. After finishing of radiotherapy and the induction chemotherapy, MRI of the spine showed no evidence of the masses intraspinallybut regressing bony lesions persist (Figures 4A and 4B).
According to the chemotherapy protocol the patient receives two additional consolidation courses of high dose cytarabine (1.5 g/day IV over 3 hours on days 1,3 and 5) without further intrathecal chemotherapy,the treatment course was uneventful.
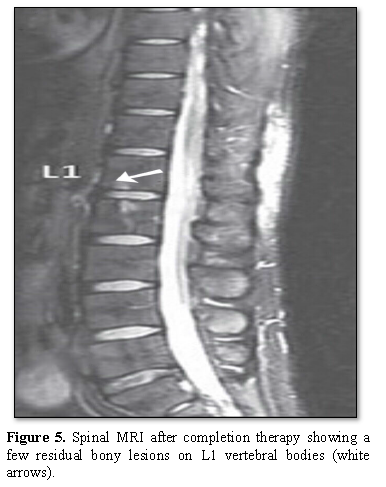
Spinal MRI was done 1 month After completion of the consolidation chemotherapy, showed that the all bony lesions on vertebral body disappeared with few residual bony lesions on the L1 and L2 (Figure 5).
Figure 5.Spinal MRI after completion therapy showing a few residual bony lesions on L1 vertebral bodies (white arrows).
The family refused to do neither new biopsy nor additional investigations, so the patient kept on regular follow up and he is now 6 years after finished his chemo-irradiation without any complications or disease recurrence.
DISCUSSION
Myeloid sarcoma was first described in 1811 and later named chloroma by King because of the green color caused by the presence of myeloperoxidase granules in the malignant myeloid cells [4-7]. Overall, myeloid sarcoma represents a rare hematologic phenomenon with an incidence of 2.5 to 9.1% in patients with AML more frequently in those with myelomonocytic and monocytic morphology (M4 and M5 French American-British subtypes) [8-11]. It could occur concomitantly, following, or, rarely, before the onset of systemic bone marrow leukemia [4,9,10]. The prevalence of myeloid sarcoma in the spine is estimated to be less than 1% among all patients with acute and chronic myeloid leukemia [7].
Granulocytic sarcomas have approximately the same rate of occurrence in both sexes. Children are more often affected than adults: 60% of patients are younger than 15 years old [12].
In this case report, we presented an isolated Granulocytic sarcoma which initially manifested as inability to walk, bilateral legs weakness and sensory deficit. Spinal MRI of our patient revealed hyperintense bony lesions on the L1-L5 vertebral bodies. Extradurallymasses were also observed between the T2 and T4, and between the T12 and L2 vertebral levels causing bilateral lower extremity weakness that quickly progressed to paraplegia. Patient underwent surgical decompression of tumor and biopsy revealed isolated granulocytic sarcoma for which he putted immediately on chemo-irradiation and high dose steroid, he responds well to the treatment and the time this manuscript was prepared the patient was undergoing regular follow up for the last uneventful 6 year.
CONCLUSION
Isolated Granulocytic sarcoma (IGS) should be considered in the differential diagnosis of patient experiences localized severe backache with motor and sensory deficit and. When Granulocytic sarcoma located in spinal column was suspected radiologically, an urgent MRI of the spine should be done with high dose steroid for those with evidence of cord compression diagnosed, surgical decompression, irradiation with chemotherapy that used for acute myeloid leukemia postoperatively constituted the treatment of choice for this tumor.Notably, treating GS in the same manner as AML may benefit patients with isolated spinal GS but large studies and new agents are needed for the treatment of isolated AML patients.
CONSENT
Written informed consent was obtained from patient’s parent for this case report.
ACKNOWLEDGMENT
We gratefully acknowledge both patient and his family for allowing us to publish their case report.
AUTHORS’CONTRIBUTIONS
Consultant Dr. Basil Kadhim Abdallah Al odda has been involved in clinical diagnostic evaluations and management.
CONFLICT OF INTERESTS
The authors declare that they have no conflict of interests.
ETHICAL CONSIDERATION
Ethical approval for this case report was obtained from NCI ethical committee. Because of the retrospective nature of this case report, the ethical committee waived the requirement of informed consent.
- Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, et al. (2009) The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: Rationale and important changes. Blood 114 : 937-951.
- Brown LM, Daeschner C, Timms J, Crow W (1989) Granulocytic sarcoma in childhood acute myelogenous leukemia. Pediatr Neurol 5 : 173-178.
- Dore GM, Devesa SS, Curtis RE, Linet MS, Morton LM (2012) Acute leukemia incidence and patient survival among children and adults in the United States, 2001-2007. Blood 119 : 34-43.
- Burns A (1811) Observations of surgical anatomy: Head and neck. Edinburgh, Scotland : Thomas Royce 1811 : 364-366.
- King A (1853) A case of chloroma. Monthly J Med Soc 17 : 97.
- Reardon G, Moloney WC (1961) Chloroma and related myeloblastic neoplasms. Arch Intern Med 108 : 864-871.
- Seok JH, Park J, Kim SK, Choi JE, Kim CC (2010). Granulocytic sarcoma of the spine: MRI and Clinical Review. AJR Am J Roentgenol 194 : 485-489.
- Bakst R, Wolden S, Yahalom J (2012) Radiation therapy for chloroma (granulocytic sarcoma) Int J Radiat Oncol Biol Phys 82 : 1816-1822.
- Bakst RL, Tallman MS, Douer D, Yahalom J (2011) How I treat extramedullary acute myeloid leukemia. Blood 118 : 3785-3793.
- Kalayci M, Sümer M, Yenidünya S, Ozdolap S, Açikgöz B (2005) Spinal granulocytic sarcoma (chloroma) presenting as acute cord compression in a nonleukemic patient. Neurol India 53 : 221-223.
- Pacilli L, Coco LF, Ramadan SM, Giannì L, Pingi A, et al. (2010) Promyelocytic Sarcoma of the Spine: A case report and review of the literature. Adv Hematol 1: 1-1.
- Pui MH, Fletcher BD, Langston JW (1994) Granulocytic sarcoma in childhood leukemia: Imaging features. Radiology 190 : 698-702.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)