768
Views & Citations10
Likes & Shares
A childhood infection, in conjunction with RA-related genetic factors, can trigger the development of RA [5], with estrogen playing a key role in the final occurrence of the disease. The incidence of RA in men is less than 20% of that in women [6]. Male hormones, unlike female hormones, do not change rapidly around the age of 50 but rather decline gradually over time, which may reduce their involvement in the development of RA. However, men may also experience a decrease in estrogen levels around the same age, although without any corresponding feminine characteristics.
There are relatively few reports on arthropathy that manifests during menopause [7]. Joint pain or arthritis occurring in the fingers makes it difficult to differentiate it from RA. Previous studies have reported that HRT is effective against menopausal joint symptoms and may prevent the onset of RA [8]. In this case, we report that while HRT suppresses menopausal symptoms including arthropathy, it is less effective in treating RA itself.
DEFINITION OF MENOPAUSE
Clinically, the patient’s menstrual periods had been absent for one year, and her Simplified Menopausal Index (SMI) score exceeded 51/100. Serological tests revealed that her serum estradiol (E2) level was at the lower limit of 20 pg/mL, while her follicle-stimulating hormone (FSH) level was above 40 mIU/mL. Surgical menopause is also considered a factor when defining menopause.
THERAPY
For the treatment of menopausal symptoms, HRT was administered [9]. The estrogen component was a 17β-E2 patch applied every 2 days for 26 days. Progestin therapy consisted of 10 mg of dydrogesterone for 12 days, followed by a 5-day break.
For the treatment of RA, MTX was orally administered three times at 16 mg/day every 12 hours, and 5 mg of folic acid was orally administered 48 hours after the MTX dose to mitigate any side effects.
RESULTS
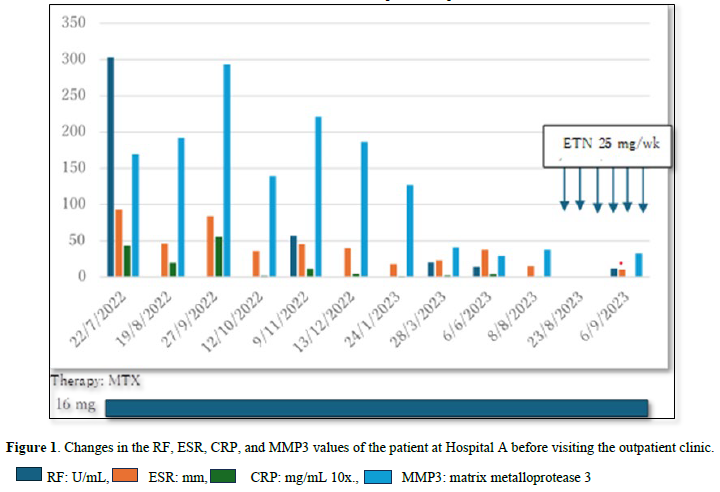
One year before menopause, the patient started experiencing bilateral shoulder joint pain and entered menopause in February 2019. Over time, the pain progressed to the joints of her wrists, ankles, and neck, and eventually to her hands and fingers. In July 2022, she visited the hospital, where blood tests showed elevated RF at 303 units and CRP at 4.33. An echogram presented moderate positive findings (Figure 1), leading to a diagnosis of RA. MTX was prescribed at a dose of 16 mg/week. Although she sometimes missed MTX doses, her CRP levels remained generally low. However, by August 2023, her joint symptoms had not improved, prompting the addition of ETN 25 mg/week, for which she received seven doses. Despite this, her joint symptoms failed to improve, and menopausal symptoms such as hot flashes worsened, leading her to visit a private outpatient clinic.
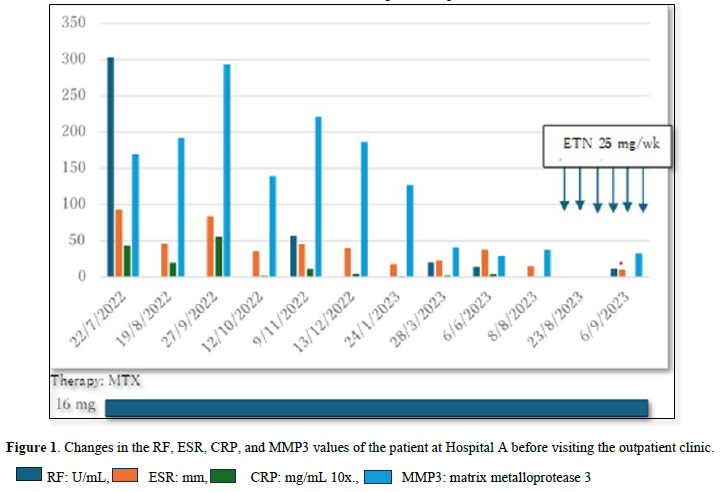
After a year of taking MTX 16mg orally once a week, inflammatory markers had almost completely disappeared. However, non-inflammatory joint pain appeared, so weekly intramuscular injections of the biological agent Etanercept 25mg were started. After six injections, there was no relief, so menopausal arthropathy was suspected.
The patient first visited the clinic in October 2023 presenting with pain in the neck, both shoulders, both wrists, both knees, both ankle joints, and the right toe, with swelling in both wrists. However, her blood tests surprisingly showed a CRP level of 0.03 and an RF level of 8. Her E2 was below the measurement limit (< 24.0), and FSH was high at 96.9. Based on these hormone levels, she was diagnosed with menopause. The Simplified Menopause Index, which determines the severity of menopausal symptoms, was high at 68/100.
MTX was continued, and cyclic HRT was initiated on the same day. At the patient’s follow-up visit in December 2023, her morning stiffness (MS) had reduced to 0 minutes, and her pain on movement had improved from 14 regions at the first visit to 6 regions. The swelling had disappeared, and the pain visual analog scale (p-VAS) score had decreased from 100 to 77. Subsequently, HRT was continued, and the MTX dose was reduced from 16 mg to 8 mg per week. However, two months later, in February 2024, the patient’s MS returned for 60 minutes, and pain during movement pain worsened to nine areas. By March, it was determined that RA activity had increased, prompting an increase in MTX to 14 mg/week, and the addition of 5 mg of oral prednisolone (PSL). In April, the patient experienced movement-related pain in only two areas, and her p-VAS score improved to 17 (Table 1).
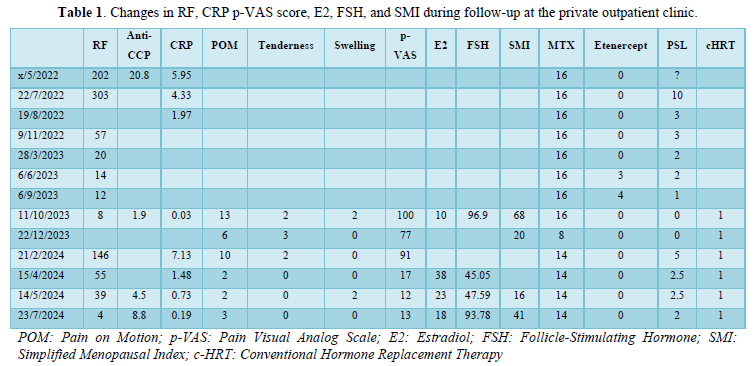
The patient was first seen at our hospital on November 10, 2023. Since the previous doctor did not record the p-VAS, the pain at the time of the first visit was set at 100. The CRP was negative at 0.03, but there was pain on motion in 13 places and tenderness and swelling in 2 places. 17βestradiol E2 was below the limit of measurement and FSH was high at 96.9. As it had been one year since menopause, regular HRT was started.
DISCUSSION
As observed from the course of this case and the treatment details, it is clear that MTX was appropriately administered for RA. However, despite adequate treatment, the RA joint symptoms of the patient gradually worsened, although her CRP and MMP3 levels increased after she missed her MTX doses. Menopausal joint symptoms also emerged, but the exact timing of their onset remains unclear.
Our previously encountered cases showed early development of RA, around the age of 40 years, which remained in complete remission, and joint symptoms emerged about five years later with the onset of menopause. HRT successfully alleviated these symptoms in all cases. However, in this case, the distinction between RA and menopausal joint symptoms was unclear. Many of these joint symptoms are due to tendonitis, which often progresses to trigger finger or hand osteoarthritis [10], and these conditions frequently overlap. However, the increase in CRP was minimal. The levels of CRP, ESR, and MMP3 indicated that the RA was almost in remission, leading to a reduction in the MTX dose from 16 mg to 8 mg. Unfortunately, this reduction caused an exacerbation of RA. The joint symptoms related to menopause were masked by the worsening of RA, making it difficult to assess the impact of HRT. However, after increasing the MTX dose to 14 mg and adding 5 mg of oral PSL, the patient’s symptoms improved, and by July 2024, she had movement pain in only two areas, with no swelling, and both her RA and menopausal arthropathy had subsided.
In summary, menopausal arthropathy seems to have appeared shortly after the onset of RA in this case. While RA was in serological remission owing to adequate administration of MTX, menopausal arthropathy persisted. Although it improved with HRT, the symptoms worsened as treatment for RA was tapered. Thus, HRT alone was unable to control RA. Both menopausal arthropathy and RA symptoms improved only after increasing the dose of MTX and continuing conventional HRT.
CONSENT
Informed consent was obtained from the patient for the publication of this case report.
ACKNOWLEDGMENTS
We thank Dr Sasse Belinda (Monash Health, Australia) for her suggestions.
CONFLICT OF INTEREST
None
FUNDING
None
- Rigante D, Bosco A, Esposito S (2015) The Etiology of Juvenile Idiopathic Arthritis. Clin Rev Allergy Immunol 49(2): 253-261.
- Gunthri KA, Dugowson JF, Voigt LF, Koepsell TD, Nelson JL (2010) Does pregnancy provide vaccine-like protection against rheumatoid arthritis? Arthritis Rheum 62(7): 1842-1848.
- Goemaere S, Ackerman C, Goethals F, De Keyser F, Van der Straeten C, et al. (1990) Onset of symptoms of rheumatoid arthritis in relation to age, sex and menopausal transition. J Rheumatol 17(12): 1620-1622.
- Orellana C, Saevarsdottir S, Klareskog L, Karlson EW, Alfredsson L, et al. (2015) Postmenopausal hormone therapy and the risk of rheumatoid arthritis: Results from the Swedish EIRA population-based case-control study. Eur J Epidemiol 30(5): 449-457.
- Oka S, Furukawa H, Shimada K, Hashimoto A, Komiya A, et al. (2019) Association of HLA-DRB1 genotype with younger age onset and elder age onset rheumatoid arthritis in Japanese populations. Medicine (Baltimore) 98(48): e18218.
- Nakajima A, Sakai R, Inoue E, Harigai M (2020) Prevalence of patients with rheumatoid arthritis and age-stratified trends in clinical characteristics and treatment, based on the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Int J Rheum Dis 23(12): 1676-1684.
- Magliano M (2010) Menopausal arthralgia: Fact or fiction. Maturitas 67(1): 29-33.
- Miyachi K, Sasse B, Ihara A (2018) THU0695 Does hormone replacement therapy prevent undifferentiated arthritis progressing to rheumatoid arthritis? Ann Rheum Dis 77(2): 540-541.
- Zaw JJT, Howe PRC, Wong RHC (2018) Postmenopausal health interventions: Time to move on from the Women's Health Initiative? Ageing Res Rev 48: 79-86.
- Burkard T, Rauch M, Spoendlin J, Prieto-Alhambra D, Jick SS, et al. (2020) Risk of hand osteoarthritis in new users of hormone replacement therapy: A nested case-control analysis. Maturitas 132: 17-23.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Allergy Research (ISSN:2642-326X)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Pathology and Toxicology Research
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)