3934
Views & Citations2934
Likes & Shares
These lesions like in this infant are often mistaken for other common soft tissue tumors like dermoid cyst and hemangiomas as birthmarks. While some lesions remain indolent or grow slowly, others exhibit aggressive growth patterns during adolescence. The precise course of these lesions remains uncertain, highlighting the need for further research in this area.
Management strategies may include careful watch, surgical intervention, endovascular embolization, or a combination of both depending on various factors such as lesion size, location, and associated symptoms [2]. Being present superficially against hard bony surface makes them prone to severe bleeding following blunt head trauma.
In this case report, we present an infant with a scalp AVM, emphasizing the clinical presentation and highlight the challenges associated with their diagnosis. Increased awareness of these vascular anomalies and their potential complications is essential for prompt and effective management in pediatric patients.
CASE PRESENTATION
A two-and-a-half-month-old male infant presented with a small scalp swelling located on the right side above the right ear, in the prominent parietal region. The swelling was noticed by the parents twenty days after birth and was characterized by a slight increase in size without pain or tenderness on palpation. There was no history of trauma during delivery or afterward, and the infant had an unremarkable perinatal course following regular antenatal care. He was born via normal vaginal delivery, first order, with a birth weight of 2.58 kg and was exclusively breastfed, achieving normal growth and development. Family history was negative for significant diseases. The parents were concerned about the potential impact of the swelling on the underlying brain, its nature, future course, and its impact on the infant's future well-being (Figure 1).
On examination, the swelling was well-demarcated, approximately 24mm × 8mm in size, slightly raised and globular shape. The overlying skin appeared normal in color, with no signs of ulceration. The swelling was soft, mobile, not adherent to underlying structure, non-tender and pulsatile, without audible bruits. Vital signs were within normal limits, and systemic examination revealed no abnormalities.
INVESTIGATIONS
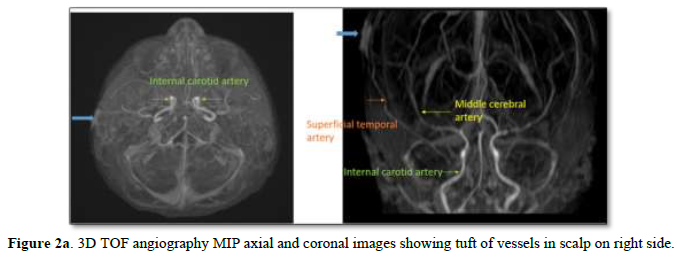
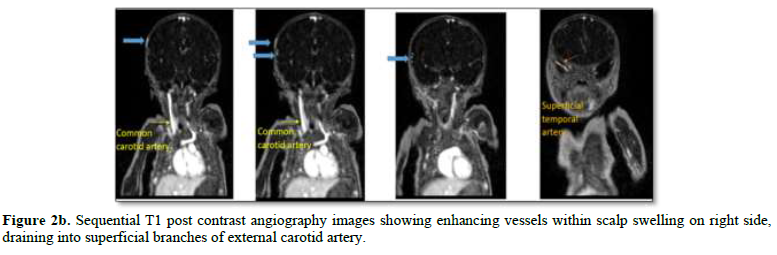
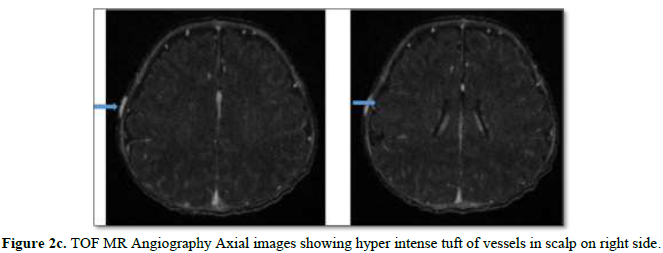
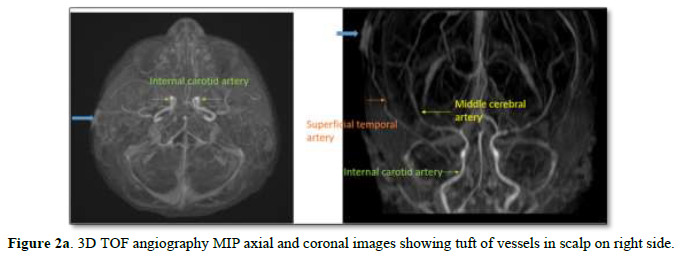
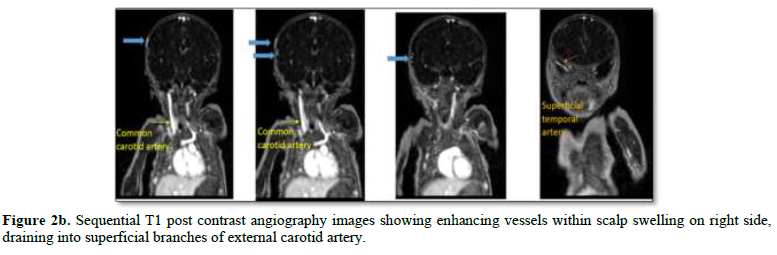
Further evaluation was pursued to address concerns of intracranial extension/association, prompting scheduling of an MR Angiogram. Results revealed a prominent extracranial enhancing curvilinear vascular structure in the right parietal region, fed by the superficial temporal artery, with no intracranial extension (Figures 2a-2c).
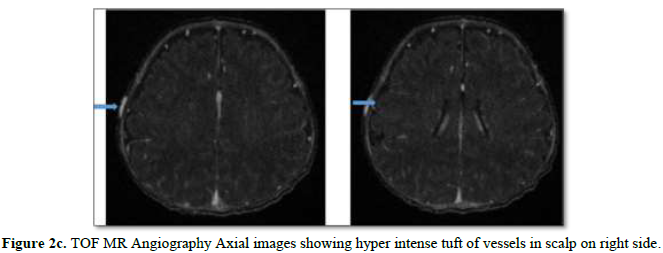
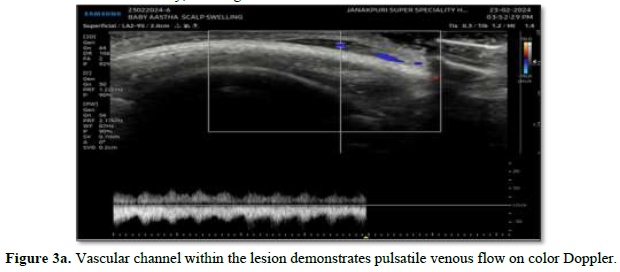
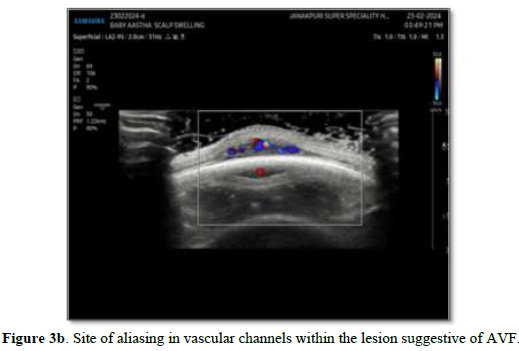
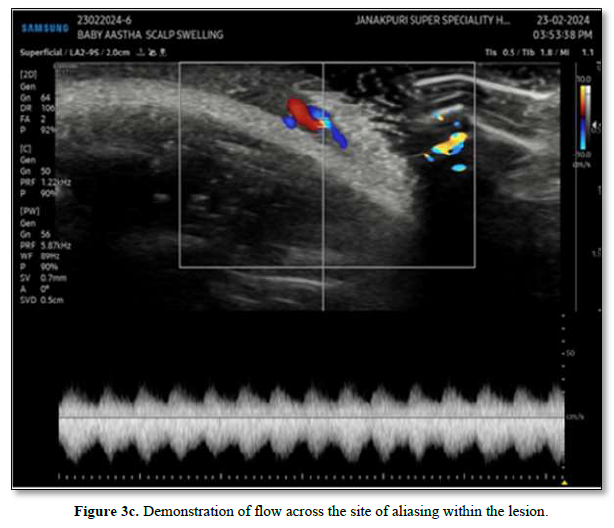
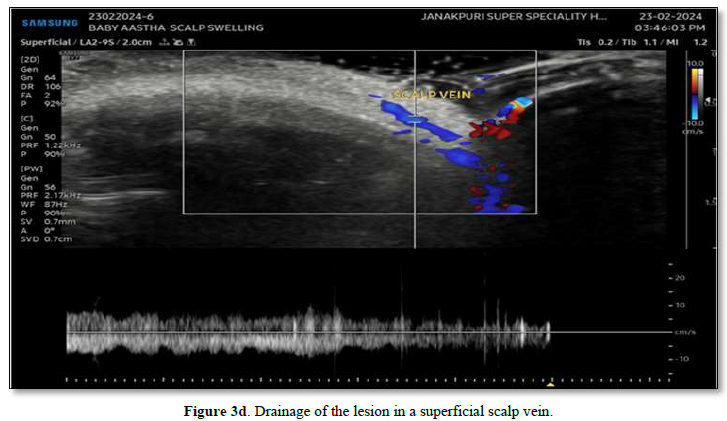
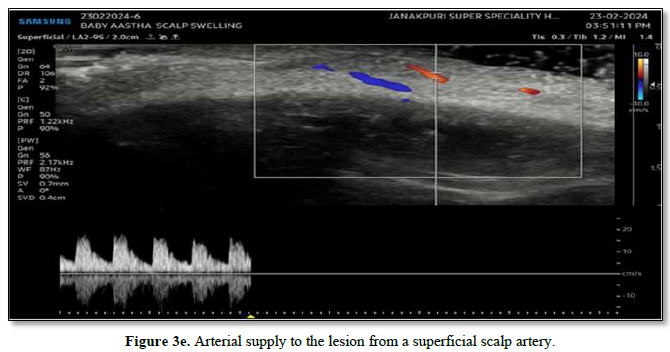
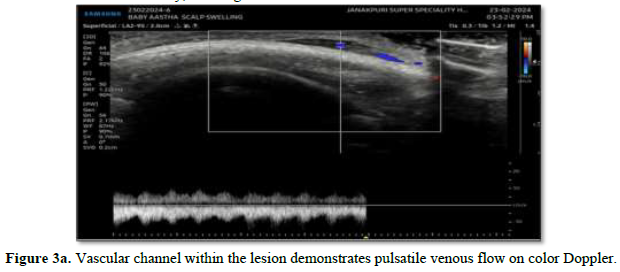
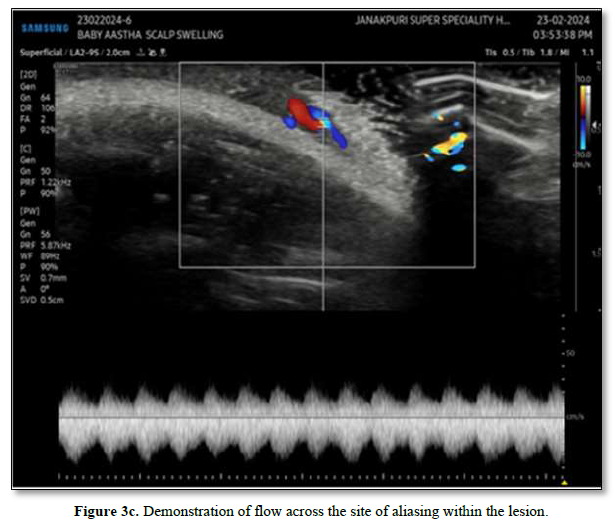
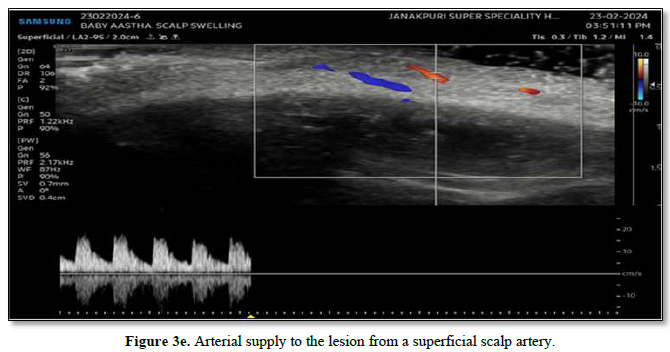
To confirm its arterial origin, Doppler Ultrasound was conducted. The imaging revealed a hypoechoic lesion measuring 8*3 mm, with Doppler imaging indicating prominent arterial and venous channels within the lesion, along with demonstrable flow. Notably, aliasing between arterial and venous channels within the lesion suggested an AVM. Additionally, the arterial and venous channels appeared to drain into the scalp vein, confirming the diagnosis of a scalp AVM (Figure 3a-3e).


Given these findings, a decision was made for careful watch and vigilant monitoring, with instructions to avoid trauma. Subsequent follow-up assessments showed no increase in the size of the swelling, leading to the decision to continue with careful watch and vigilant monitoring.
DISCUSSION
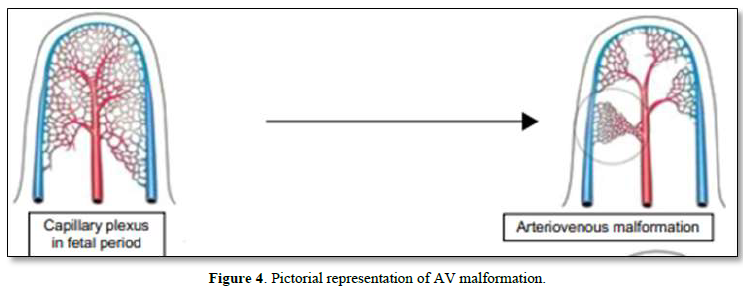
Congenital Scalp Arteriovenous malformations (AVMs) are characterized by absent capillary beds, resulting in direct shunting of blood from arteries to veins through a fistula or nidus [3-5] (Figure 4).

Scalp arteriovenous fistulas (AVMs) present unique challenges in both diagnosis and management due to their rarity and varied clinical presentations. Clinical manifestations may include small innocuous soft tissue swelling as in this infant. Progressive lesion may present with disfigurement, tissue destruction, pain, and bleeding.
Scalp arteriovenous fistulas (AVMs) and related vascular anomalies must be distinguished from other conditions presenting with scalp lesions. A few important differential diagnoses to consider include [6].
Dermoid Cyst
Dermoid cysts are benign inclusion cysts resulting from trapped skin elements beneath the scalp. They typically present as painless, firm, non-mobile lumps and may grow slowly over time. Dermoid cysts can be differentiated from AVFs based on imaging characteristics and absence of pulsations or hemodynamic changes (Figure 5).
Hemangioma
Small hemangiomas are common vascular growths in infants and may involve the scalp. They often present as rapidly growing lesions in the first few weeks of life and then resolve spontaneously. Unlike AVMs, hemangiomas do not typically present with pulsatile masses or significant shunting of blood flow. Imaging studies and clinical evaluation can aid in distinguishing between hemangiomas and AVFs (Figure 6).

Another important consideration in the differential diagnosis of scalp lesions is the possibility of a delayed subaponeurotic fluid collection. This condition typically occurs following trauma to the scalp, such as during childbirth, and involves the accumulation of blood and fluid beneath the scalp's aponeurosis layer (Figure 7).

Indeed, careful palpation of soft tissue swellings on the scalp is crucial in narrowing down the differential diagnosis, particularly when considering arteriovenous malformations (AVMs). While pulsations may be present in AVMs, they can sometimes be subtle and easily missed if not thoroughly evaluated. It is essential to note that pulsations may be absent or difficult to appreciate in certain cases, emphasizing the need for a comprehensive evaluation that includes other clinical findings and diagnostic modalities. Identifying pulsations on palpation can be challenging, particularly in cases where the lesion is small or deep-seated. In such instances, additional diagnostic tools such as imaging studies (ultrasound, MRI, Angiography) may be supportive; however, Angiography (CT/MR Angiography) and DSA is essential if there is plan for intervention in terms of surgery / embolization.
Imaging modalities such as ultrasound and MRI are pivotal in confirming the diagnosis, delineating vascular anatomy, and assessing the extent of involvement. In our case, the absence of intracranial communication signifies an isolated extracranial AVF, reducing the risk of intracranial hemorrhage. Doppler examination and MRI are crucial for diagnosis and assessment, while cerebral angiography remains the gold standard [7]. Angiography is essential for diagnosis, while management involves a multidisciplinary approach, considering cosmetic concerns, prevention of bleeding, and symptom relief. Surgical excision remains the mainstay treatment, with careful attention to complete ligation of feeding arteries to prevent recurrence.
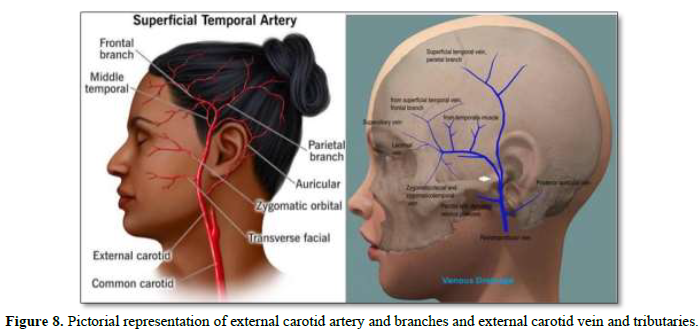
Diagnosis and management of Scalp Arteriovenous Fistulas (AVMs) require careful consideration of differential diagnoses and an understanding of the anatomical and functional aspects of the superficial temporal artery (STA) and its associated venous drainage.
The STA and STV are common vessels involved in scalp AVMs, STA, a major external carotid artery branch, supplies blood to the scalp via various branches, including the middle temporal artery [8]. Venous drainage occurs through superficial veins, including the superficial temporal vein (STV), draining into the external jugular vein. In scalp AVFs, abnormal arteriovenous connections lead to increased blood flow and venous pressure, causing vein dilatation and visible pulsations (Figure 8).
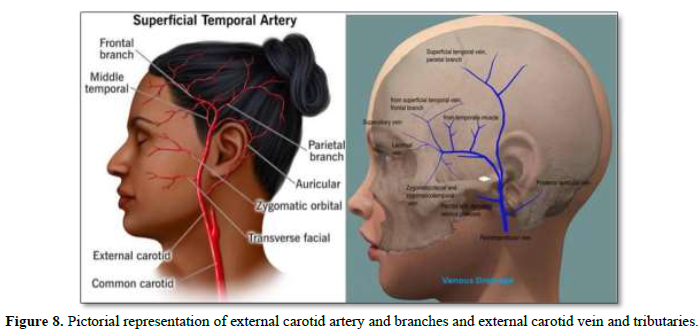
In scalp AVFs, careful evaluation of STA and venous drainage is pivotal. Imaging modalities aid in delineating anatomy, guiding interventions targeting feeder arteries, including STA branches. Surgical or endovascular interventions aim to disrupt abnormal connections while preserving surrounding vasculature. Management strategies vary based on lesion characteristics and interdisciplinary collaboration, emphasizing the importance of tailored approaches for optimal outcomes.
The STA is indeed a major arterial supply to the scalp and may contribute to the blood flow in many scalp AVMs [8]. Its branches, including the frontal and parietal branches, can be implicated in feeding these lesions. Similarly, the STV is a significant vein in the scalp and is often involved in draining blood from these malformations.
However, scalp AVMs can also receive blood supply from other arteries, such as the occipital artery, posterior auricular artery, or branches of the internal carotid artery. Additionally, venous drainage can occur through various routes, including other superficial scalp veins and sometimes communicating veins connecting with deeper venous structures.
Therefore, while the STA and STV play crucial roles in many cases of scalp AVMs, it's essential to recognize that the arterial feeders and venous drainage patterns can vary widely among different patients and lesions. A comprehensive evaluation, including imaging studies like angiography, is necessary to assess the specific vascular anatomy of each individual case and guide appropriate management strategies. Congenital AVMs can have diverse arterial feeders and venous drainage patterns depending on individual variations and anatomical factors.
While the STA and STV are frequently implicated in scalp AVMs, it's crucial to recognize the potential variability in the vascular anatomy of these lesions. A comprehensive evaluation, often including imaging studies such as angiography, is necessary to assess the specific arterial feeders and venous drainage patterns in each case. This individualized approach ensures accurate diagnosis and guides appropriate treatment strategies tailored to the patient's unique vascular anatomy.
Surgical or endovascular interventions targeting the feeder arteries, including branches of the STA, aim to disrupt the abnormal arteriovenous connections and restore normal vascular dynamics. Preservation of the surrounding vasculature, including the STA and its branches, is crucial to prevent ischemic complications and ensure adequate perfusion of the scalp tissues.
In summary, the STA and its venous drainage play a pivotal role in the pathophysiology and management of scalp AVFs. Understanding their anatomy and function is essential in diagnosing, evaluating, and treating vascular abnormalities in this region, ultimately optimizing patient outcomes and minimizing complications.
Management strategies for scalp AVMs are multifaceted and dependent on factors such as lesion size, location, symptoms, and associated complications. Conservative management with close monitoring may suffice for small lesions without significant symptoms. However, intervention, including embolization or surgical excision, should be considered based on clinical judgment and interdisciplinary collaboration.
CONCLUSION
This case report underscores the significance of early detection, precise diagnosis, and vigilant monitoring in enhancing patient outcomes and addressing parental concerns. Through the utilization of imaging techniques such as MR Angiogram and Doppler Ultrasound, the diagnosis of Congenital scalp AVM was confirmed; excluded intracranial extension, and initiated a plan of careful observation and vigilant monitoring.
Given the potential for mimicry with conditions like dermoid cysts and hemangiomas, accurate differential diagnosis of scalp lesions is paramount. Understanding the anatomical and functional aspects of arterial feeders, notably the superficial temporal artery (STA), and venous drainage patterns is crucial for guiding treatment strategies, whether through surgical excision or endovascular interventions.
While the trajectory of scalp AVMs remains uncertain, proactive monitoring and timely intervention, if necessary, are imperative in averting complications such as bleeding and tissue damage.
In summary, this case report adds to the existing literature on rare congenital scalp AVMs, highlighting the intricacies of diagnosis and management. By sharing our experience, we aim to foster comprehension, facilitate early intervention, and ultimately optimize care for pediatric patients grappling with rare vascular anomalies of the scalp.
- Jennifer JM, John BM (2005) Current management of hemangiomas and vascular malformation. Clin Plasti Surg32: 99-116.
- Richling B, Killer M, Al-Schameri AR, Ritter L, Agic R, et al. (2006) Therapy of brain arteriovenous malformations: Multimodality treatment from a balanced standpoint. Neurosurgery 59(suppl 3): S148-S157.
- Halim AX, Johnston SC, Singh V, McCulloch CE, Bennett JP, et al. (2004) Longitudinal risk of intracranial hemorrhage in patients with arteriovenous malformation of the brain within a defined population. Stroke 35: 1697-1702.
- Shovlin CL, Jackson JE, Bamford KB, Jenkins IH, Benjamin AR, et al. (2008) Primary determinants of ischemic stroke/brain abscess risks are independent of severity of pulmonary arteriovenous malformations in hereditary hemorrhagic telangiectasia. Thorax 63: 259-266.
- Fleetwood IG, Steinberg GK (2002) Arteriovenous malformations. Lancet 359: 863-873.
- https://www.jaypeedigital.com/eReader/chapter/9789350909829/ch1
- Gaillard F, Ghannouchi H, Machang'a K (2024) Brain arteriovenous malformation. Accessed on: April 08, 2024. Reference article: Radiopaedia.org
- Yonenaga K, Tohnai I, Mitsudo K, Mori Y, Saijo H, et al. (2011) Anatomical study of the external carotid artery and its branches for administration of super selective intra-arterial chemotherapy via the superficial temporal artery. Int J Clin Oncol 16: 654-659.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Spine Diseases
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- International Journal of AIDS (ISSN: 2644-3023)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)