2268
Views & Citations1268
Likes & Shares
Demodex is a permanent ectoparasite, living on pilo-sebaceous units and mainly on the faces; two species are specific for humans (Demodex folliculorum and Demodex brevis).
Demodex infestation produces allergic and inflammatory reactions to the skin, such as redness, hair loss and scarring; it gives rise to a variety of skin conditions collectively termed as demodicosis.
Parasitic infestation of the skin is a common presentation to dermatologists as well as to primary care physicians. The disease burden can cause a debilitating itch or complications from secondary infection. Accurate diagnosis can be facilitated by microscopic examination of skin scrapings, microscopic examination of hair or in some cases biopsy.
The present review summarizes the epidemiological aspects, the eclectic role of the Demodex in skin disorders, and the treatment challenges. It is important to consider Demodex mites in the etiology of unexplained cases of skin diseases.
Keywords: Demodex, Ectoparasite, Demodicosis, Epidemiology, Clinical forms
INTRODUCTION
The mites Demodex folliculorum and Demodex brevis are ubiquitous and obligatory ectoparasites typically found on man, they asymptomatically inhabit the pilo-sebaceous units of most adults (80%-100%) [1].
The two detritivore species mainly involve the face and the head, but Demodex brevis has a wider distribution on body [2], these mites are affecting most commonly the perioral, periorbital areas of the face, the lids and lashes [1,3], occurring in 10% of skin biopsies and 12% of follicles [4].
With regard to the terminology of the disease, both “demodicosis” and “demodicidosis” have been used with the latter being more commonly used in the older dermatologic literature. “Demodicidosis” with the suffix “id” is analogous to “tuberculid” or “bacterid” and implies a state of hypersensitivity or allergic reaction to substances of the pathogen. Therefore, “demodicidosis” does not reflect the current view on the pathogenesis of this dermatosis and “demodicosis” would be a preferred term [5,6].
The term demodicosis represents all the cutaneous diseases caused by Demodex mites, the infection usually remains asymptomatic and may have a pathogenic role only with high densities of mites, their extra-follicular location and also because of immune imbalance [1].
Demodex can also exacerbate pre-existing skin conditions [1,3]. Demodex proliferation can result in a number of cutaneous disorders including pustular folliculitis, pityriasis folliculorum, papulopustular and granulomatous rosacea, among others [7,8].
Demodicosis can be classified as primary, in the absence of other inflammatory dermatoses, having a sudden onset, or secondary when associated with other cutaneous or systemic diseases, developing gradually over existing dermatoses [9].
CLASSIFICATION
Phylum: Arthropoda
Subphylum: Chelicerata
Class: Arachnida
Order: Trombidiformes
Family: Demodicidae
PATHOGENESIS
Increased mite density has been correlated with increase readiness of lymphocyte to undergo apoptosis and with increased number of NK cells with Fc receptors [12], significant decrease in absolute numbers of lymphocytes and T-cell subsets and significant increase in IgM levels have also been found in patients presenting with Demodex proliferation and facial skin lesions [13], colonization of the skin with Demodex could be a reflection of the immune response of the host to the organism [12].
Penetration of Demodex into the dermis or, more commonly, an increase in the number of mites in the pilo-sebaceous unit of >5/cm2, is thought to cause infestation, which triggers inflammation [4], demodex mites consume epithelial cells and induce micro-abrasions, which can result in epithelial hyperplasia and reactive hypekeratinization around the base of the lashes, forming cylindrical dandruff [14].
Several pathogenic mechanisms have been proposed for demodicosis, including:
(1) Blockage of hair follicles and sebaceous ducts by the mites or the reactive hyperkeratosis;
(2) Stimulation of the host’s humoral and cell-mediated immune reactions by the mites and their waste products;
(3) A foreign body granulomatous reaction to the mite’s chitinous skeleton;
(4) A vector role for bacteria [15-17].
SEX AND AGE CONSIDERATION OF INFESTATION
Males are more heavily infested than females with both species [2]. Demodex mites can be found in any age groups except the new-borns who are presumably infested soon after birth by direct contact [10]; it is more commonly encountered in young adult when the sebum secretion rate is at its highest [1].
Sengbusch and Hauswrith found a pronounced increase in the prevalence of Demodex brevis with increasing age. Whereas the prevalence of Demodex folliculorum tended to remain more constant [18].
PREDISPOSING FACTORS
Though Demodex folliculorum isn’t an uncommon occurrence, a weakened immune system, dermatitis, skin affection, alopecia, Acne (especially inflammatory types), HIV, malignant neoplasia, chronic use of topical steroids and lymphosarcoma can predispose to demodicosis [1,3,7].
The relationship with the presence of the mite Demodex folliculorum and rosacea is one of the most intriguing; It has been suggest that the presence of Demodex folliculorum in the affected skin could be related to the development of rosacea [19,20].
MODE OF TRANSMISSION
Demodex infection can be transmitted directly by close contact with the infected people. The mites are transferred between hosts through contact of hair, eyebrows and sebaceous glands [1].
Infection can be transmitted indirectly through household items, as it was shown that the mites can long enough to remain viable outside the host, Demodex can be transferred by contaminated towels, combs, blankets, bath sponge and night clothes.
In addition, practitioners often advise patients to start washing their bed sheets and pillowcases regularly in hopes of preventing re-inoculation.
In severe cases, patients may even need to consider replacing their pillows altogether.
DESCRIPTION OF THE PARASITE
SITES OF INVOLVEMENT
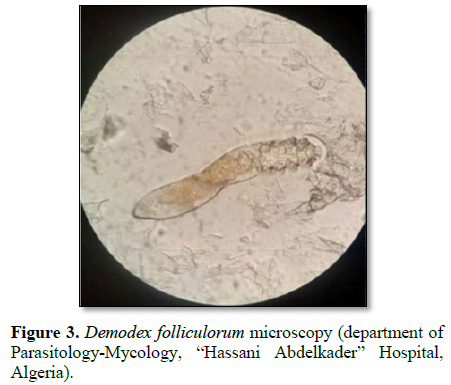
Mites have been retrieved from almost every area of human skin but have a predilection for face. Demodex is typically found on cheeks, nose, chin, forehead, temples, eyelashes, brows, the balding scalp, ear, neck and less commonly upper and medial region of chest and back are also infested [4,17,21] (Figures 2 and 3).
CLINICAL DESCRIPTION
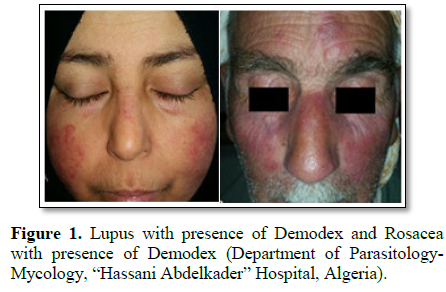
Demodex infection usually remains asymptomatic and may have a pathogenic role only with high densities of mites and also because of immune imbalance [1].
Human demodicosis is clinically characterized (Table 1) by erythema or slight skin redness (Figure 1) that strongly suggest demodicosis [4,23], followed by scaly skin mostly across the forehead [4], characteristic dry follicular scale unsheathing the base of the lanugo hair or plugging the follicular opening [23], dryness or skin that feels rough like sandpaper [4,23], presence of papules or pustules [4,3], itchy skin [4] and burning sensation [23].
Ocular demodicosis, is including chronic blepharitis, chalazia or less commonly, kerato-conjunctivitis; and auricular demodicosis is including external otitis or myringitis [3,24]. Cylindrical dandruff, which are lipid and keratin accumulations that form distinct cuffs surrounding lash roots, are characteristic of demodectic blepharitis [25].
Other atypical clinical presentations leading to misdiagnosis, are summarizes in Table 2.
Skin lesions associated with abnormal increase of Demodex mites in patients with other known skin or systemic diseases can be classified as secondary demodicosis [3].
It is important to consider Demodex mites in the etiology of unexplained cases of skin diseases. A study by Emre et al. [35] in turkey in 2009 demonstrated that Demodex folliculorum infestation was higher in Behcet disease and mite elimination may be useful, even in patients without any complaint, for the treatment of ocular and eyelid discomforts of these patients.
Karincaoglu et al. [31] in Turkey in 2009 demonstrated that the prevalence of Demodex folliculorum was higher in patients with seborrheic dermatitis.
The Demodex folliculorum mites are more often detected in patients with acne of III and IV degrees and with papular and pustular rosacea; Demodex folliculorum provokes more severe clinical forms of acne [11].
It seems that Demodex folliculorum is more often associated with erythema and epithelial desquamation, whereas Demodex brevis is linked with papulo-pustular eruption, symmetrical rashes and conditions arising on the background of a pre-existing disease [9].
DIAGNOSIS
Infestation with Demodex is common, and mites are present in 23% of healthy adults and may have a pathogenic role only when present in high densities or in immunosuppression [1,4,36].
Therefore, a high index of clinical suspicion about the etiological role of demodex in various dermatoses is necessary.
Identification methods used in assessing the presence of mites include, invasive methods (skin scraping, follicular scales, epilation) or non-invasive in vivo detection and quantification of Demodex mites by confocal laser scanning microscopy [1,5,11] (Table 3).
The density of Demodex mites can be studied by KOH preparations of follicular plugs, skin scrapings and standardized skin surface biopsy specimens [6].
It has been suggested that an increasing density of mites correlates with an increasing perifollicular inflammation and clinical manifestation. A density of more than 5 mites/follicle or 5 mites/cm2 of standardized skin surface biopsy specimen has been considered to be pathogenic [1,36]. Symptoms may develop when the follicles become heavily infested, or when the mites penetrate into the dermal tissue [6].
Confocal laser scanning microscope makes it possible to visualize mites that are both found in the deeper layers of the skin and inaccessible to scarification [11], this method has a high potential to be a diagnostic means for demodecosis, which makes it possible to scan various layers of the skin that allows the determination of the depth of mite detection (≈46.63 µ), number of mites and also their size. The lack of epithelium trauma and painful procedures are other additional advantages of this method.
COMPLICATIONS
Demodicosis is often diagnosed in patients with severe clinical forms of acne and rosacea, it may worsen acne outbreaks, rosacea rashes, and dermatitis patches [1,3]. This fact suggests that the mites complicate the course of the diseases, and thus promoting the development of inflammatory elements [11]. Demodicosis should be considered in the differential diagnosis of recurrent or recalcitrant rosacea-like, granulomatous rosacea-like and perioral dermatitis-like eruptions of the face [6].
Demodex may act as a vector of transmission of various infections from area of body to another or between individuals by its potential to ingest and transport various microorganisms (Microsporum canis, Bacillus sp., Streptococcus sp.) [14,37].
TREATMENT
Because Demodex are nocturnal, it is important to limit their ability to reproduce and migrate when they are most active.
Demodicosis remains a diagnostic and therapeutic challenge, anti-parasitic therapies used against lice or scabies may fail in control of Demodex folliculorum mites [34].
The symptoms of some skin diseases are clearly reduced when this parasite is correctly treated [23,34,38], on the other hand, some symptoms persist when only anti-bacterial therapeutic agents are used [38].
Various regimens have been used to treat demodicosis (Table 4), including systemic metronidazole and ivermectin as well as topical metronidazole, salicylic acid, gamma benzene hexachloride, sublimed sulfur, permethrin, crotamiton, benzyl benzoate and tea tree oil [6,24,25,39]. In severe cases, such as those with HIV infection, oral ivermectin may be recommended [1].
A study, have reported complete recovery, with the disappearance of facial mites in treatment with combinations of oral and topical metronidazole in a case of fulminant rosacea-like eruption with multiples Demodex folliculorum mites [40]. Furthermore, oral anti-parasitic drug such as ivermectin is used alone or in combination with metronidazole [39].
Grossmann et al. [41] used 750 mg/day metronidazole for 3 weeks in conjunction with 100 mg/day prednisolone, topical 2% metronidazole and 0.15% lindane emulsion [41]. Baima and Sticherling used oral ivermectin for skin lesions caused by Demodex, in combination with 4% pilocarpine gel in blepharitis [15].
CONCLUSION
Demodex are permanent ectoparasite of dermatological importance and it has been shown that these mites are playing an important role in the occurrence of a series of skin diseases, but further clarification of these associations is required.
A high index of clinical suspicion about Demodex in various dermatoses can help in early diagnosis and appropriate, timely, and cost effective management.
We strongly recommend including laboratory examination and an acaicide for the treatment to improve the quality of life of some patients.
We conclude that Demodex mites are common but overlooked.
MAJOR HIGHLIGHTS
• Demodex is a permanent ectoparasite, living mainly on the face.
• It asymptomatically inhabits the pilo-sebaceous units of most adults.
• Mites are affecting most commonly the perioral, periorbital areas of the face, the lids and lashes.
• Atypical clinical presentations are possible (acne, tinea versicolor, Folliculitis of the scalp, unilateral rosacea).
• It is important to consider Demodex mites in the etiology of unexplained or severe cases of skin diseases.
• Correct skin identification with routine microscopy or confocal laser scanning microscopy is necessary.
• Oral anti-parasitic drug such as ivermectin alone or in combination with metronidazole is required.
• Washing patient bed sheets and pillowcases regularly is recommended in hopes of preventing re-inoculation.
ACKNOWLEDGEMENT
The authors declared no potential conflict of interest with respect to the research, authorship and/or publication of this article.
1. Rather PA, Hassan I (2014) Human demodex mite: The versatile mite of dermatological importance. Indian J Dermatol 59: 60-66.
2. Aylesworth R, Vance JC (1982) Demodex folliculorum and Demodex brevis in cutaneous biopsies. J Am Acad Dermatol 7: 583-589.
3. Chen W, Plewig G (2014) Human demodicosis: Revisit and a proposed classification. Br J Dermatol 170: 1219-1225.
4. Bikowski JB, Del Rosso JQ (2009) Demodex dermatitis: A retrospective analysis of clinical diagnosis and successful treatment with topical crotamiton. J Clin Aesthet Dermatol 2: 20-25.
5. Forton F, Seys B (1993) Density of Demodex folliculorum in rosacea: A case-control study using standardized skin-surface biopsy. Br J Dermatol 128: 650-659.
6. Hsu CK, Hsu MM, Lee JY (2009) Demodicosis: A clinicopathological study. J Am Acad Dermatol 60: 453 462.
7. Guerrero-González GA, Herz-Ruelas ME, Gómez-Flores M, Ocampo-Candiani J (2014) Crusted demodicosis in an immunocompetent pediatric patient. Case Rep Dermatol Med 2014: 458046.
8. Vu JR, English JC 3rd (2011) Demodex folliculitis. J Pediatr Adolesc Gynecol 24: 320-321.
9. Akilov OE, Butov YS, Mumcuoglu KY (2005) A clinicopathological approach to the classification of human demodicosis. J Dtsch Dermatol Ges 3: 607-614.
10. Moravvej H, Dehghan-Mangabadi M, Abbasian MR, Meshkat-Razavi G (2007) Association of Rosacea with Demodicosis. Arch Iranian Med 10: 199-203.
11. Kubanov A, Yulia G, Grevtseva A (2016) Important aspects of Demodex diagnostics. J Surg Dermatol 1.
12. Akilov OE, Mumcuoglu KY (2004) Immune response in demodicosis. J Eur Acad Dermatol Venereol 18: 440-444.
13. El-Bassiouni SO, Ahmed JA, Younis AI, Ismail MA, Saadawi AN, et al. (2005) A study on Demodex folliculorum mite density and immune response in patients with facial dermatoses. J Egypt Soc Parasitol 35: 899-910.
14. Liu J, Sheba H, Tseng SCG (2010) Pathogenic role of Demodex mites in blepharitis. Curr Opin Allerg Clin Immunol 10: 505-510.
15. Baima B, Sticherling M (2002) Demodicidosis revisited. Acta Derm Venereol 82: 3-6.
16. Bonnar E, Eustace P, Powell FC (1993) The Demodex mite population in rosacea. J Am Acad Dermatol 28: 443-448.
17. Rufli T, Mumcuoglu Y (1981) The hair follicle mites Demodex folliculorum and Demodex brevis: Biology and medical importance: A review. Dermatologica 162: 1-11.
18. [18] Sengbusch HG, Hauswrith JW (1986) Prevalence of hair follicle mites: Demodex folliculorum and Demodex brevis (Acari: Demodicidae). In: A selected human population in western New York, USA. J Med Entomol 23: 384-388.
19. Chang YS, Huang YC (2017) Role of Demodex mite infestation in rosacea: A systematic review and meta-analysis. J Am Acad Dermatol 77: 441-447.
20. Rios-Yuil JM, Mercadillo-Perez P (2013) Evaluation of Demodex folliculorum as risk factor for the diagnosis of rosacea in skin biopsies. Mexico’s General Hospital (1975-2010). Indian J Dermatol 58: 157.
21. Basta-Juzbasic A, Subic JS, Ljubojevic S (2002) Demodex folliculorum in development of dermatitis rosaceiformis steroidica and rosacea-related diseases. Clin Dermatol 20: 135-140.
22. Spickett SG (1942) Studies on Demodex folliculorum Simon (1842). I. Life history. Parasitology 51: 181-192.
23. Ayres S, Anderson NP (1932) Demodex folliculorum: Its role in the etiology of acne rosacea. Arch Derm Syphilol 25: 89-98.
24. Liang L, Safran S, Gao Y, Sheha H, Raju VK, et al. (2010) Ocular demodicosis as a potential cause of pediatric blepharoconjunctivitis. Cornea 29: 1386-1391.
25. Tiuseco KAL, Siong RLB, MD, Reyes JM, Iguban EB. (2012) Petroleum jelly versus tea tree oil and tea tree facial wash lid scrub in patients with blepharitis associated with above-normal Demodex. Philipp J Ophthalmol 37: 73-82.
26. Brown M, Hernandez-Martin A, Clement A, Colmenero I, Torrelo A (2014) Severe Demodex folliculorum-associated oculocutaneous rosacea in a girl successfully treated with ivermectin. JAMA Dermatol 150: 61-63.
27. Fernandez-Flores A, Alija A (2009) Scalp folliculitis with Demodex: Innocent observer or pathogen? Braz J Infect Dis 13.
28. Merad Y, Lansari T, Adjmi-Hamoudi H (2018) Demodex folliculorum mimicking fungal infection: A case report. J Dermatitis 3: 1.
29. Vashisht D, Singh J, Baveja S, Tiwari R, Bhatnagar A (2016) Unilateral demodicidosis of face mimicking Hansens disease. Dermatol Rep 8: 6891
30. Helou W, Avitan-Hersh E, Bergman R (2016) Demodex folliculitis of the scalp: Clinicopathological study of an uncommon entity. Am J Dermatopathol 38: 658-663.
31. Karincaoglu Y, Tepe B, Kalayci B, Atambay M, Seyhan M (2009) Is Demodex folliculorum an aetiological factor in seborrhoeic dermatitis? Clin Exp Dermatol 34: e516-e520.
32. Garcia-Vargas A, Mayorga-Rodriguez JA, Sandoval-Tress C (2007) Scalp demodicidosis mimicking favus in a 6 year old boy. J Am Acad Dermatol 57: S19-S21.
33. Mehta V, Balachandran C, Mathew M (2007) Skin-colored papules on the face. Indian J Dermatol Venerol Leprol 73: 368.
34. Schaller M, Sander CA, Plewig G (2003) Demodex abscesses: Clinical and therapeutic challenges. J Am Acad Dermatol 49: S272-274.
35. Emre S, Aycan OM, Atambay M, Bilak S, Daldal N, et al. (2009) What is the importance of Demodex folliculorum in Behçet’s disease? Turkiye Parazitol Derg 33: 158-161.
36. Erbagci Z, Ozgoztasi O (1998) The significance of Demodex folliculorum density in rosacea. Int J Dermatol 37: 421-425.
37. Wolf R, Ophir J, Avigad J, Lengy J, Krakowski A (1988) The hair follicle mites (Demodex spp.): Could they be vectors of pathogenic microorganisms? Acta Derm Venereol 68: 535-537.
38. Sanfilippo AM, English III JC (2005) Resistant scalp folliculitis secondary to Demodex infestation. Cutis 76: 321-324.
39. Salem DA, El-Shazly A, Nabih N, El-Bayoumy Y, Saleh S, et al. (2013) Evaluation of the efficacy of oral ivermectin in comparison with ivermectin-metronidazole combined therapy in the treatment of ocular and skin lesions of Demodex folliculorum. Int J Infect Dis 17: e343-e347.
40. Hoekzema R, Hulsebosch HJ, Bos JD (1995) Demodicidocis or rosacea: What we did treat? Br J Dermatol 133: 294-299.
41. Grossmann B, Jung K, Linse R (1999) Tubero-pustular demodicosis. Hautarzt 50: 491-494.
42. Holzchuh FG, Hida RY, Moscovici BK, Villa Albers MB, Santo RM (2011) Clinical treatment of ocular Demodex folliculorum by systemic ivermectin. Am J Ophtalmol 151: 1030-1034.
43. Abbelaar CCF, Venema AW, Van Djik MR (2018) Topical ivermectin in the treatment of papulopustular rosacea: A systematic review of evidence and clinical guideline recommendations. Dermatol Ther (Heidelb) 8: 379-387.
44. Fulk GW, Murphy B, Robins MD (1996) Pilocarpine gel for the treatment of demodicosis - A case series. Optom Vis Sci 73: 742-745.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Chemotherapy Research Journal (ISSN:2642-0236)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)