15136
Views & Citations14136
Likes & Shares
HIV related skin disease is one important case of HIV-associated complications, cause poor quality of life and even to mortality. In order to understand features of AIDS-associated skin complications in clinical. Blood items, microbe characterization and pathology of 9 patients derived from Nanyang Medical College hospitals with AIDS-associated skin diseases were measured by corresponding techniques. Of the 9 cases infected by different virus, fungus and bacteria showed different features of body surface and pathology. AIDS-associated skin complications show various clinical characterizations, combination different fields contribute to elucidate features of AIDS-associated skin complications.
Keywords: AIDS, AIDS-associated skin complications, Pathology
INTRODUCTION
In the world, patients of human immunodeficiency virus (HIV) infections have been reached to 35 million (31.8 million adults and 3.2 million children
As to AIDS patients, HIV-associated skin complications shows a number of complex characterizations with respect of occurrence of novel pathogens. Therefore, it brings about great challenge for clinical treatment. Combination of different ways is an important to further elucidate characterizations and under mechanisms of HIV-related complication. Take into consideration extensive emergence of skin diseases of AIDS patients, in the current study, 9 cases of HIV-related skin diseases are analyzed by pathology, microbiology and image.
MATERIALS AND METHODS
Patient selection
Study design
Quantity of CD4+ T cell was measured using flow cytometry instrument (BD, USA) according to kit instructions. Histological analysis was performed by HE staining. Morphological observations of pathogens were fulfilled by microbe culture. Results of X-ray and computed tomography (CT) were used in imaging analysis, respectively.
RESULTS AND DISCUSSION
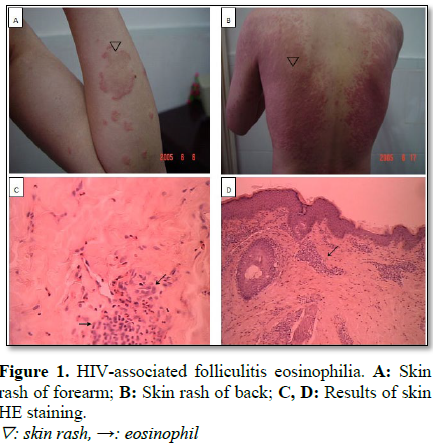
HIV-associated skin folliculitis eosinophilia
Case 1, a male had 34 years and was definitely diagnosed as AID by CDC. Quantity of CD4+ T cell was 9 μl. Erythema and papules accompanied itching were fund in face, neck, arms and legs. Invasived erythema and papules, fusion of partial papules without ulceration, erosion, scaling rash, desquamation were observed in neck, trunk and limbs (Figures 1A and 1B). Pathological results showed a large number of eosinophil infiltration were occurred in the dermal layer (Figures 1C and 1D). The patient was in the acute phase of HIV-associated skin folliculitis eosinophilia.
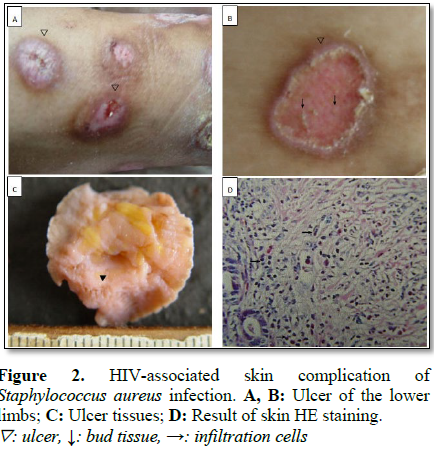
HIV-associated skin complication of Staphylococcus aureus infection
Case 2, a female, 39 years, was definitely diagnosed as AID by CDC. Quantity of CD4+ T cell was 13 μl. Multiple round ulcers formed pink granulation tissue on the surface were observed in lower segments of left and right legs by stereology examination (Figures 2A and 2B). Local tissues showed an obvious complication characterized by ulceration and erosion of skin mucus, inflammatory leaching of surface, necrosis of epidermides and submucosal granulation tissue and scar formation (Figure 2B). Sebaceous glands and sweat gland showed normal appearances, but inflammatory infiltration could be fund in the stroma of neutrophils, eosinophils and lymphocyte (Figures 2C and 2D). The patient was in the acute phase of HIV-associated skin infection of S. aureus.
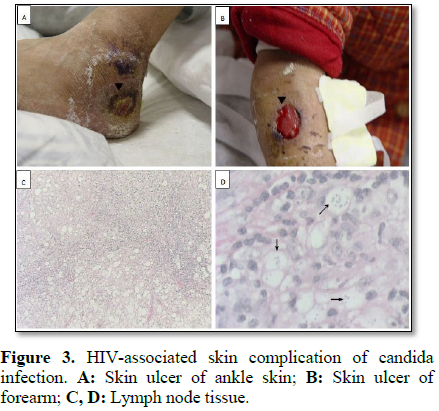
HIV-associated skin superficial complication of fungal infection
Case 3, a female, 32 years, was definitely diagnosed as AID by CDC. Quantity of CD4+ T cell was 98 μl. Body temperature sustain at 38.9℃. Diverse symptoms including inflation of superficial lymph nodes, multiple-sites skin ulcers, membrane formed by white deposition in the tonsils of mouth were observed. Multiple ulcers with dark red color and epithelium drop of ulcerated tissue were widely observed (Figures 3A and 3B). Lymph node of biopsy showed fungal infection in which the mild spreading mycelium of yeast was detected (Figures 3Cand 3D). Patient was in the period of remission of HIV-associated skin complication of candida infection.
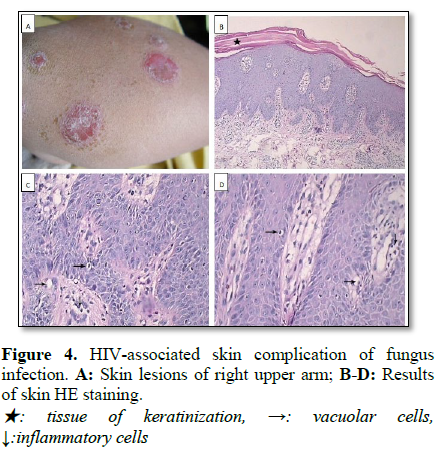
Case 4, a female, 42 years, was definitely diagnosed as AID by CDC. Quantity of CD4+ T cell was 28 μl. Mild granulation tissue appeared in the surface of skin was observed by stereology check (Figure 4A). Local keratinization or hyperkeratosis of epithelium, enlarged keratinization of skin surface, thickened epithelium was observed by tissue biopsy (Figure 4B). In the dermis, some vacuolar degeneration, scattered infiltration of lymphocytes, some squamous epithelium with a mild to moderate atypical hyperplasia were fund, although integrital hair roots and survived sebaceous were observed (Figures 4C and 4D). Patient was the acute phase of HIV-associated skin superficial infection of fungus.
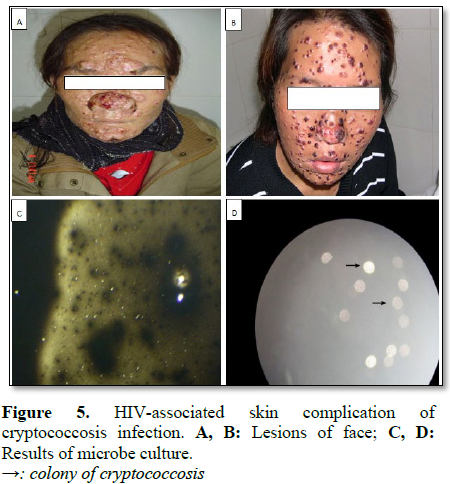
HIV-associated skin complication of cryptococcosis infection
Case 5, a female, 30 years, was definitely diagnosed as AID by CDC. Quantity of CD4+ T cell count was 28 μl. Multiple furuncles and partial ulcer were fund on the face (Figures 5A and 5B). Cryptococcus was isolated from the medium by microbial culture (Figures 5C and 5D). The patient was the acute phase of HIV-associated skin complication of cryptococcosis infection.
HIV-associated skin complication of Penicillinosis marneffei infection
Case 6, a female, 31 years, was definitely diagnosed as AID by CDC and showed fever at 38~39℃, fatigue, poor appetite, maransis, weight loss, cough, white phlegm and sore throat. Quantity of CD4+ T cell was 150 μl. Multiple complications were detected. In addition, red and dark red pimples were scatted in skin of all body at a diameter from 3 to 8 mm and caved ones was mainly occurred in the head face and trunk. Several white plaques could be observed in the mouth (Figures 6A and 6B). Pathological tissue biopsy showed an obvious fibrosis was fund in lesion tissue (Figure 6C). Under high power microscopic view, mycelium of P. marneffei was detected in medium of microbiological culture (Figure 6D). The patient was the period of remission of HIV-associated skin complication of P. marneffei infection.
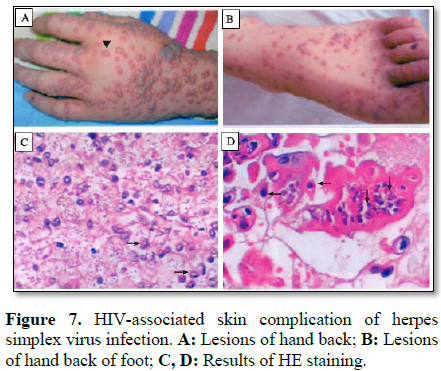
HIV-associated skin complication of herpes simplex virus infection
Case 7, a boy, 5 years, was definitely diagnosed as AID by CDC. Quantity of CD4+ T cell was 102 μl. Fresh water vacuole was fund in hand back and feet, some ones were ulcerated and fused (Figures 7A and 7B). HE staining results showed that particles of inclusion virus were presented in lymphocytes and monocytes (Figures 7C and 7D). Patients was in the period of remission of HIV-associated skin complication of herpes simplex virus infection.
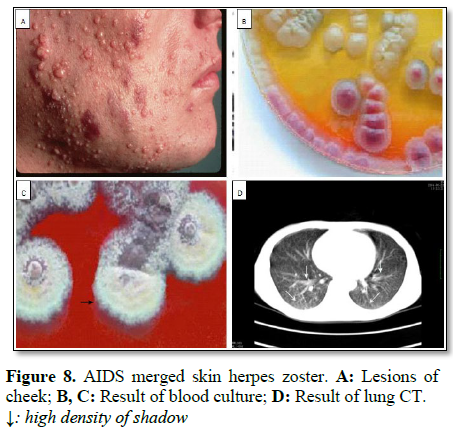
HIV-associated skin complication of herpes zoster virus infection
Case 1, a male, 42 years, was definitely diagnosed as AID by CDC and showed intermittent fever and limb weakness. Quantity of CD4+ T cell was 25 μl. Zoster virus was observed in low part of xiphoid as well as face (Figures 8A and 8B). Growth of pathogenic microbes was observed by serum culture (Figure 8C). Intermittent fever and cough were repeatedly occurred in the night. In advanced stage of AID, multiple infections and diffuse high-density shadow in middle and lower regions of right and left lungs were fund in patient (Figure 8D). Patients was in the acute phase of HIV-associated skin complication of herpes zoster virus infection.
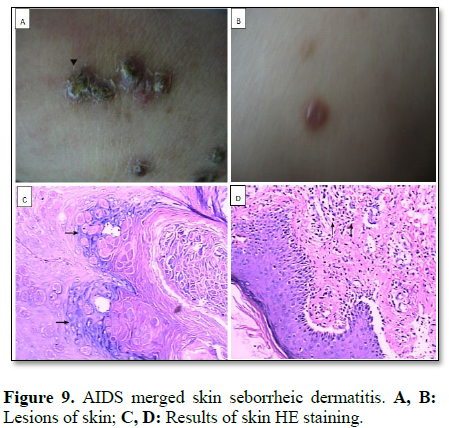
HIV-associated seborrheic dermatitis
Case 1, a female, 28 years, was definitely diagnosed as AID by CDC. Quantity of CD4+ T cell was 35 μl. Multiple nodular swellings were fund in back, forearm and ankle (Figures 9A and 9B). Large of swelling cells were extensively located around of sebaceous by histopathologic analysis (Figures 9C and 9D). Patients were in the acute phase of HIV-associated seborrheic dermatitis.
DISCUSSION
Occurrences of HIV-related skin folliculitis eosinophilia are close related with HIV infection characterized by obvious increase of blood eosinophils, large number of eosinophil infiltration in hair follicles of skin [4]. As an autoimmune disease, fungal infections can result in an inhibitory role on antigen exposure of body that may cause a severe hypersensitive effect. So, hidden antigen exposure of sebaceous glands can cause acidophilic granulocyte infiltration [5]. Noteworthy, only symptom analysis of skin without pathology, HIV-related skin folliculitis eosinophilia is often regarded as damp pestilence, allergic dermatitis, neurodermatitis that is often cause an event of misdiagnosis. In addition, it is necessary to distinguish HIV-related skin folliculitis eosinophilia from drug eruption. Drug eruption is generally divided into non anti-ADIS drug eruption and anti-ADIS drug eruption. Widely distributed rash in the skin is one of obvious features of non-anti-ADIS drug eruption. Anti-ADIS drug eruption can be further divided into mild type and severe type, former is often occurred in the trunk and limb that mainly show features of measles, later one exhibits features of Steven-Johnson syndrome as well as liver injury [6,7].
Infection of S. aureus can result in folliculitis, abscess and pustular sore of skin. Incidence of these complications is significantly increased in AIDS patients compared with that of normal people, mainly caused by S. aureus infection in AIDS patients. S. aureus has a higher opportunity of colonization than that of normal group with respect of serious impairment of skin mucous barrier and neutrophil function defect caused by HIV infection [8]. In the early stage of HIV infection, no special characterizations are observed. Along with advancing of HIV infection, except of S. aureus infection, streptococcus, S. epidermidis, Pseudomonas spp. and Escherichia coli can also enter into body and bring about a threat on immunity. Therefore, serious skin lesions, multiple site complications, high-degree of recurrence and drug resistance can be detected [9].
Superficial fungal infections of AIDS often show ringworm of body, tinea cruris, tinea manuum, Athlete’s foot, tinea capitis and onychomycosis [10,11]. Superficial fungal infection is a very common phenomenon in AIDS patients. Characterizations of most patients are similar with that of non-HIV-infected population. If two and/or more pathogens simultaneity invade into body, some special features such as skin ulcers, abscesses and skin necrosis and skin lesions are observed that should cause a difficult for treatment [12]. Deep skin infection of cryptococcus may cause mortality of normal population, also be one of the common reasons of death of AIDS patients [13]. Infection of cryptococcosis can result an in injury of central nervous system, lungs, skin and bone. In addition, cryptococcus can spread into all the tissues and organs of body by blood circulation [13]. Skin lesions are mainly occurred in face, head, trunk and limbs. Noteworthy, contagious soft wart pimples, such as skin lesions, nodules, plaques, pustules, abscess and ulcer are mainly fund in trunk and limbs [14,15].
In the AIDS patients, infection of P. marneffei can cause a damage on mono-nuclear macrophage that in turn lead to a widely dissemination of body and high mortality. HIV-related complication of P. marneffei infection is one of the most common opportunistic infections in AIDS patients in Southeast Asia and southern region of our country, such as Guangxi and Yunnan [16]. Patients show fever, anemia, swelling of liver and enlargement of spleen lymph node, weight loss and pulmonary symptoms, 71% of them should undergo skin complication [17]. Skin lesions are mainly occurred in the face, upper trunk and limbs, and characterized by necrotic papules, infected papules, nodules, acne-like lesions, abscesses and ulcers [18]. Nevertheless, necrotizing papules are regard as marker of HIV-related skin disease of P. marneffei infection. As to skin complication, it is important to pay attention to other organ damage derived from P. marneffei infection in the process of treatment.
Herpes simplex virus (HSV) is divided into two groups including HSV-1 and HSV-2. In the HSV-1, lesions are occurred in mouth, nose and other parts of body, HSV-2 in reproductive organs [19]. Clinical studies have demonstrated that early onset of herpes simplex has a 2~12 days of latency, which is emerged in the mouth and fund in skin mucosa junction of mouse and nose. In where, serious symptoms including of appearance of stigmata, generation of cluster small bubbles, formation of erosion and blister of broken bubbles, deposition of pigment and itching or burning are observed [20]. In the recurrent herpes simplex, cluster small bubbles can be repeatedly occurred in the same region derived from some stimulate factors such as cold and menstrual period [21]. Genital herpes is occurred in the genital organs that is associated with transmit by sexual contact. During whole course of AIDS, herpes simplex virus has a rich opportunity to induce an injury on cells. In the early stages of HIV infection, manifestations of herpes simplex virus infected patients are similar with that of non-HIV infected ones [20,21]. In advanced process of AIDS, herpes simplex infection often shows a high-frequent recurrence, a long course of ill, a wide range of lesions, a high occurrence of ulcers and necrosis and obvious drug resistance. Meanwhile, infection of genital herpes can result in a significant increase of HIV dissemination.
Incidence of herpes zoster virus infection is the highest among of HIV-associated complications, 26.4% of them is occurred in the stage of HIV infection, 73.6% of them in the AIDS stage [22]. A rapid progression of ill course is observed, it only experience 2 or 3 days from onset of obvious pain occurrence derived from a small amount of erythema and papules to complications of whole nervous system. Meanwhile, clustered blister, bulla, blood blister, necrosis are fund in the surface of erythema. Obvious scars are formed on healing. Patients have other symptoms of all body, such as fever, tiredness, and so on [23].
Seborrheic dermatitis is a chronic spilled sebum that is associated with the overgrowth of M. furfur. Skin lesions are occurred in the regions of spilled sebum of head, forehead and nasolabial. Greasy scales are formed on the surface of erythema with itching [24]. As to seborrheic dermatitis of AIDS patients, skin lesions are often detected in the face, chest, back and limbs, even whole body. Generally, seborrheic dermatitis is regard as the first HIV-related complication of AIDS patients [25].
Diagnose of HIV-associated skin complications is one challenge work with respect of complex etiology and diverse symptoms. In the current study, combination of pathology and microbiology is contribute to elucidate HIV-related skin complications at early stage and take measure preventing occurrence of these complication. Noteworthy, pathogenic infections can cause a threat on other organs because of low immunity of AIDS patients. Therefore, multiple strategies should be applied in the clinical to understand characterizations of HIV-associated skin complication.
ACKNOWLEDGEMENT
We gratefully acknowledge the many contributions of Pro Liu Rongzhi to this research program. This research was funded by the National Natural Science Foundation (No.31271285), National Natural Science Foundation of Henan (No. 12B310010, NO.142102310211).
1. Xiang Y, Guo W, Liang K (2015) An unusual appearing skin lesion from Penicillium marneffei infection in an AIDS patient in central China. Am J Trop Med Hyg 93: 3-7.
2. Pires CA, JucáNeto FO, de Albuquerque NC, Macedo GM, Batista Kde N, et al. (2015) Leprosy reactions in patients coinfected with HIV: Clinical aspects and outcomes in two comparative cohorts in the Amazon region, Brazil. PLoS Negl Trop Dis 9: e0003818.
3. Bentubo HD, Mantovani A, Yamashita JT, Gambale W, Fischman O, et al. (2015) Yeasts of the genital region of patients attending the dermatology service at Hospital São Paulo, Brazil. Rev Iberoam Mycol 32: 229-234.
4. Rane SR, Agrawal PB, Kadgi NV, Jadhav MV, Puranik SC, et al. (2014) Histopathological study of cutaneous manifestations in HIV and AIDS patients. Int J Dermatol 53: 746-751.
5. Matsumura Y, Miyachi Y (2012) Atypical clinical appearance of eosinophilic pustular folliculitis of seborrheic areas of the face. Eur J Dermatol 22: 658-662.
6. Nara T, Katoh N, Inoue K, Yamada M, Arizono N, et al. (2009) Eosinophilic folliculitis with a Demodex folliculorum infestation successfully treated with ivermectin in a man infected with human immunodeficiency virus. Clin Exp Dermatol 34: e981-983.
7. Parker SR, Parker DC, McCall CO (2006) Eosinophilic folliculitis in HIV-infected women: Case series and review. Am J Clin Dermatol 7: 193-200.
8. Farley JE, Hayat MJ, Sacamano PL, Ross T, Carroll K, et al. (2015) Prevalence and risk factors for methicillin-resistant Staphylococcus aureus in an HIV-positive cohort. Am J Infect Control 43: 329-333.
9. Hemmige V, McNulty M, Silverman E, David MZ (2015) Predictors of skin and soft tissue infections in HIV-infected outpatients in the community-associated methicillin-resistant Staphylococcus aureus era. Eur J Clin Microbiol Infect Dis 34: 339-347.
10. Moreno-Coutiño G, Hernández-Castro R, Toussaint-Caire S, Montiel-Robles M, Sánchez-Pérez FS, et al. (2015) Histoplasmosis and skin lesions in HIV: A safe and accurate diagnosis. Mycoses 58: 413-415.
11. Liu GN, Huang JS, Zhong XN, Zhang JQ, Zou ZX, et al. (2014) Penicillium marneffei infection within an osteolytic lesion in an HIV-negative patient. Int J Infect Dis 23: 1-3.
12. Demiraslan H, Alabay S, Kilic AU, Borlu M, Doganay M, et al. (2013) Cutaneous candidiasis caused by Candida glabrata in a HIV/AIDS patient. Int J STD AIDS 24: 753-755.
13. Khuraijam R, Lungran P, Yoihenba K, Laishram RS, Pukhrambam P, et al. (2015). Pancytopenia and cutaneous cryptococcosis as an indicator disease of acquired immune deficiency syndrome. Indian J Med Microbiol 33: 439-442.
14. Zacharia A, Khan MF, Hull AE, Sasapu A, Leroy MA, et al. (2013) A case of disseminated cryptococcosis with skin manifestations in a patient with newly diagnosed HIV. J La State Med Soc 165: 171-174.
15. Patel D, Desai GM, Frases S, Cordero RJ, DeLeon-Rodriguez CM, et al. (2013) Methamphetamine enhances Cryptococcus neoformans pulmonary infection and dissemination to the brain. MBio 4: e00400-00413.
16. Liu GN, Huang JS, Zhong XN, Zhang JQ, Zou ZX, et al. (2014) Penicillium marneffei infection within an osteolytic lesion in an HIV-negative patient. Int J Infect Dis 23: 1-3.
17. Nor-Hayati S, Sahlawati M, Suresh-Kumar C, Lee KC (2012) A retrospective review on successful management of Penicillium marneffei infections in patients with advanced HIV in Hospital Sungai Buloh. Med J Malay 67: 66-70.
18. Santiso G, Chediak V, Maiolo E, Mujica MT, San Juan J, et al. (2011). Disseminated infection due to Penicillium marneffei related to HIV infection: First observation in Argentina. Rev Argent Microbiol 43: 268-272.
19. Giani G, Quirino T, Sacrini F, Carbone A, Vaccher E, et al. (1996). Destructive mucocutaneous phagedenic herpes simplex virus infection in an HIV-infected patient who had a partial response to interferon and ultraviolet rays. Clin Infect Dis 22: 381-382.
20. Padovese V, Racalbuto V, Barnabas GA, Morrone A (2015) Operational research on the correlation between skin diseases and HIV infection in Tigray region, Ethiopia. Int J Dermatol 54: 1169-1174.
21. AltuntaşAydin Ö, KumbasarKaraosmanoğlu H, Korkusuz R, Özeren M, Özcan N, et al. (2015) Mucocutaneous manifestations and the relationship to CD4 lymphocyte counts among Turkish HIV/AIDS patients in Istanbul, Turkey. Turk J Med Sci 45: 89-92.
22. Katibi OS, Dlova NC, Mosam A (2015) Cutaneous cytomegalovirus infection on multi dermatomal herpes zoster scars: An isotopic immune response. Clin Exp Dermatol 40: 42-44.
23. Akinboro AO, Onayemi O, Mejiuni AD (2014) Frequency, pattern and extent of skin diseases in relation to CD4+ cell count among adults with human immunodeficiency virus infection or acquired immunodeficiency syndrome in Osogbo, south-western Nigeria. Int J Dermatol 53: 416-424.
24. Amado Y, Patiño-Uzcátegui A, Cepero de García MC, Tabima J, Motta A, et al. (2013) Seborrheic dermatitis: Predisposing factors and ITS2 secondary structure for Malassezia phylogenic analysis. Med Mycol 51: 868-875.
25. Motswaledi MH, Visser W (2014) The spectrum of HIV-associated infective and inflammatory dermatoses in pigmented skin. Dermatol Clin 32: 211-225.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Alcoholism Clinical Research
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)