751
Views & Citations10
Likes & Shares
Reversible Posterior Encephalopathy Syndrome (PRES) is a clinical entity characterized by neurological symptoms, visual disturbances and behavioral changes.
Among the etiological factors are the hypertensive states of pregnancy, an entity more and more frequent in the immediate puerperium.
Early diagnosis is fundamental, based on clinical and neuroimaging, for an adequate resolution of the clinical picture with a minimization of neurological sequelae.
The present clinical case summarizes the clinical, diagnosis, treatment and evolution of a PRES in the immediate puerperium.
Keywords: Reversible posterior encephalopathy syndrome (PRES), Headache, Puerperium, Eclampsia, Hypertension
INTRODUCTION
Posterior reversible encephalopathy syndrome (PRES), also known as reversible posterior cerebral edema syndrome[1], is a clinical entity characterized by a group of temporary neurological symptoms such as non-localized headaches, alteration of level of consciousness, seizures (originally, localized, escalating into generalized convulsive crisis) and visual alterations (photophobia, hemianopia, blurred vision, scotomas and cortical blindness) [2].
The following Etiological factors can be highlighted: hypertensive states, renal failure, cytotoxic/immunosuppressant medications, idiopathic thrombocytopenic purpura, hemolytic uremic syndrome, high doses of corticosteroid treatments, endocrine disorders, electrolyte disturbances, porphyria and blood transfusions [3]. Well established clinical associations are hypertensive disorders of pregnancy (preeclampsia, eclampsia, HELLP syndrome – haemolysis, elevated liver enzymes and low platelets) and hypertensive encephalopathy [4].
Prompt and adequate management is essential to restore basal state and minimize the risk of neurological sequelae. The aim of the treatment is preserve the patient’s hemodynamic balance with intravenous hydration and colloids administration, normal blood pressure range stabilisation and avoidance of hyper coagulable states [5].
CASE REPORT
A 35 year old primigravida at 39 weeks of gestation, admitted during labor. Past medical history of anxiety depressive syndrome being treated with escitalopram and lorazepam during pregnancy, psychiatrically monitored hypochondria and hypothyroidism.
After monitoring blood pressure (120/79 mm Hg), heart rate (73 bpm) and normal results in standard blood tests, epidural analgesia is applied successfully between L4-L5. After 4 h gives birth a 3680 g in weight, male newborn is eutocic delivered.
The second puerperium day the patient starts showing intense adaptive anxiety disorder with feelings of guilt and insecurity. Our patient presents blood pressure of 128/87 mm Hg with heart rate of 89 bpm; no neurological symptoms noted and blood results showing normal values. The patient is reviewed by the psychiatric team, being oral paroxetine prescribed and acute depressive pathology ruled out. Discharge is agreed due to
After six days, the patient is admitted to accident and emergency department due to hypertension (148/101 mm Hg), headache without vomiting, blurred vision with photopsias and increased level of anxiety with feelings of fear of imminent death.
Proteinuria test in urine is negative and oral labetalol 100 mg is administered. Psychiatric assessment refers her to the acute inpatient psychiatry unit as a postpartum depression is suspected. During her stay in the acute unit, the blood pressure reading does not show less than 150/100 mm Hg. And she experiences one minute long generalized convulsive crisis without losing sphincter control and with no post critical state. Hemodynamically stable, eupnoeic, very nervous and with a Glasgow coma scale score of 14/15, reactive mydriatic pupils, preserved cranial pairs, fasciculation of facial muscles (masseter muscles), generalized muscle spasticity with over responsive osteotendinous reflexes, the rest of the neurological and cardiopulmonary examinations are normal.
Treatment is started with intravenous magnesium sulphate and levetirazepam 500 mg every 12 h as eclampsia suspected.
Among the tests carried out (hemogram, biochemistry, sediment, CT scan), the outstanding results are the discrete proteinuria and lactate 5 mmol/L. The CT scan with endovenous contrast shows hypodensity affecting the subcortical white matter: some areas in the parietal and occipital lobes near the midline and in convexity in frontal lobes.
Especially in left frontal convexity, hyper density can be observed in some of the cortical grooves, without being able to establish diagnostic certainty.
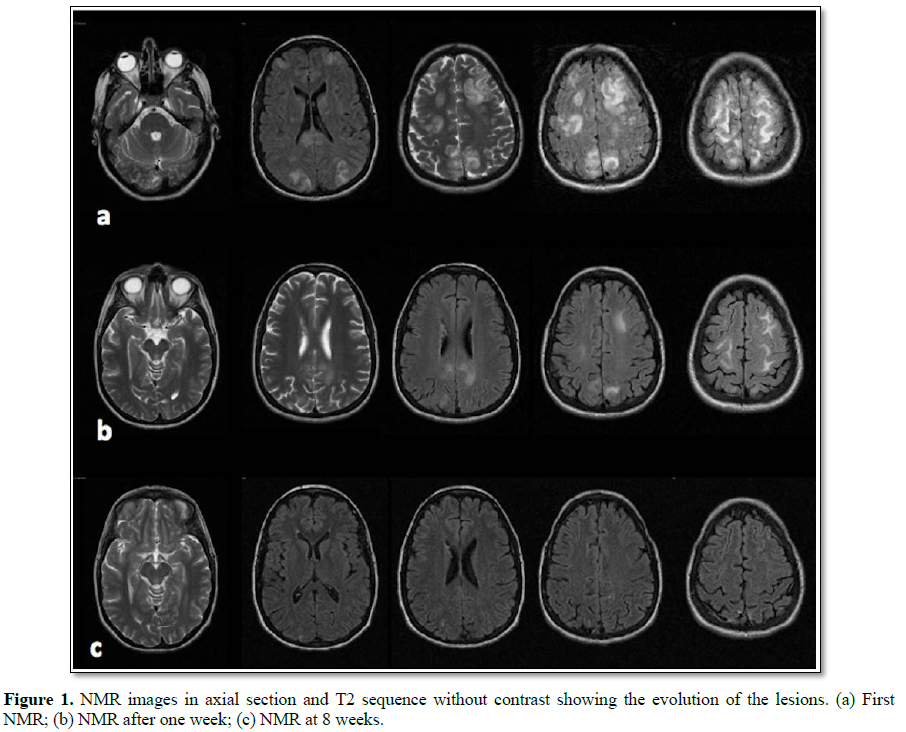
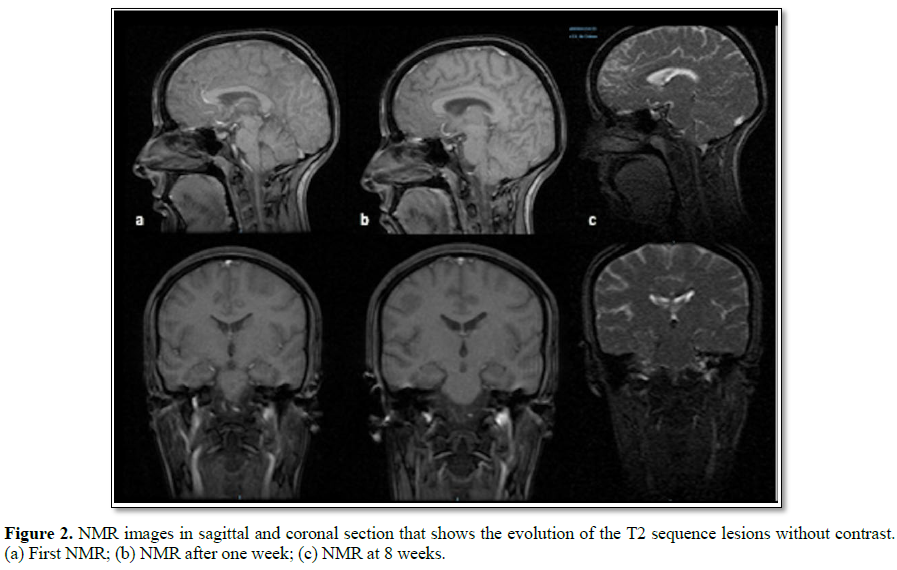
The patient is transferred to Intensive Care Unit for neurological and blood pressure monitoring. The study is completed with MRI and angiography MR, which allows discarding of aneurysmal lesions and shows a slight cerebral vasoconstriction component, being this findings compatible with PRES and with reversible cerebral vasoconstriction syndrome (RCVS) (Figures 1 and 2).
During her stay in ICU no seizures occurred, blood pressure is controlled using several intravenous treatments (labetalol, hydralazine and captopril) resulting in cessation of cephalalgia and visual alterations within the following 72 h. A week after admission, a control MRI is carried out, being the results consistent with PRES resolution stage.
The patient is discharged with antihypertensive as well as antidepressant treatments. The control MRI carried out a month later shows signs of regression of most of the alterations present in previous investigations, with only residual changes remaining.
Currently, the patient is in complete remission of the lesions as per MRI investigation and blood pressure of 106/70 mm Hg without further treatment as per hypertension clinic monitoring.
DISCUSSION
Posterior reversible encephalopathy syndrome (PRES) is a clinical-radiological entity associated with different clinical conditions, highlighting puerperium, where it appears more frequently. It’s partially known etiology will not allow establishing neither cause nor pathogeny [6].
Both preeclampsia and eclampsia are associated with arterial hypertension, and neurological alterations (eclampsia can present with seizures, even coma), both can develop with or without proteinuria. The incidence of preeclampsia is 5%, eclampsia occurs on 3% of most severe cases with an associated maternity death rate between1.8%-14% [7]. The absence of excessively high tensional figures and proteinuria as well as the psychiatric symptoms can mislead towards preeclampsia/eclampsia in the puerperium, with symptoms as headache, convulsions and behavioral changes as in this case.
During preeclampsia systemic endothelial dysfunction occurs with an increase of the peripheral vascular response and platelet aggregation, potentially, provoking multiple organ damage including central nervous system (hypertensive encephalopathy), generating the neurological signs and symptoms described above common to both eclampsia and PRES.
Cerebral edema in PRES has been explained by two different, nonexclusive, pathogenic theories: The hypo perfusion theory or “vasogenic theory” and the ischemia theory or “cytotoxic theory”.
Vasogenic theory is most accepted and most likely cause of PRES. When systemic arterial pressure’s increase exceeds cerebral auto regulatory mechanisms, a sympathetic innervation failure occurs in the branches of the basilar and cerebral arteries, originating an increase on cerebral blood flow. Histologically, the over dilation of distal arterioles with opening of the endothelial bindings in small vessels will determine the rupture of the hematoencephalic barrier, allowing extravasation into the interstitium: vasogenic cerebral edema. Subsequent vasoconstriction and cerebral ischemia occurs [8].
Patients with chronic arterial hypertension have an adaptive hypertrophy in their vessels’ walls, including the cerebral vascularization, which reduces the permeability of the blood-brain barrier. Preeclampsia is an acute clinical condition in which small elevations of blood pressure can alter the hematoencephalic barrier [9]. This theory can explain our case, where the patient had normal blood pressure during pregnancy and delivery, only reaching 160/110 mm Hg in puerperium.
The “cytotoxic theory” in PRES is based in the reduction of cerebral blood flow consequent to an acute elevation of the blood pressure, producing arterial spasm, ischemia and cytotoxic edema in the brain [5].
Within the clinical manifestations, headaches are one of the most nonspecific and frequent symptoms in PRES in the immediate puerperium with an incidence of up to 39%. Depending on its characteristics and associated symptoms, headaches can be associated with PRES o with other clinical entities, being a prompt and accurate differential diagnosis essential as it will determine treatment and prognosis [4,10].
Appropriate imaging technique that supports the PRES diagnosis is the T2 weighted MRI images, showing images compatible with bilateral, symmetrical, vasogenic edema, localized, 98% of the cases, in the subcortical white matter in parietal and occipital lobes. In specific cases, localized lesions may appear in the upper frontal area, temporal lobes, cerebellum, brainstem and basal ganglia which require a more exhaustive differential diagnosis. Sequences of T1 MRI imaging or the use of CT scan images could help to rule out other lesions (tumors, encephalitis, subarachnoid hemorrhage, venous thrombosis, etc.).
MRI observed Lesions, in our case, are hyper intense, symmetrical, parietal-occipital, compromising mainly white matter consistent with vasogenic edema and confirming PRES diagnosis. Diffusion weighted images ruled out presence of cytotoxic edema.
Early diagnosis and treatment improves prognosis with reversibility of the whole clinical picture. Treatment is formed of appropriate control of blood pressure readings with intensive monitoring. Beta-blockers (labetalol) are indicated as a first line of antihypertensive therapy. Nimodipino can be added for its effect on brain perfusion pressure, not nitroglycerine which is contraindicated as it promotes edema). Magnesium sulphate can have a beneficial effect as proved in eclampsia.
1. Ural UM, Balik G, Sentürk S, Ustüner l, Cobanoglu U, et al. (2014) Posterior reversible encephalopathy syndrome in a postpartum pre-eclamptic woman without seizure. Case Rep Obstet Gynecol 3.
2. Erbai M, Dost B, Öztürk Ö, Iskender A, Demiraran Y (2012) Twin pregnancy with posterior reversible encephalopathy syndrome and anesthesia management. J Anesth 20: 237-240.
3. Stevens CJ, Heran MKS (2012) The many faces of posterior reversible encephalopathy syndrome. Br J Radiol 85: 1566-1575.
4. Ruiz López N, Cano Hernández B, Balbás Álvarez S (2016) Posterior reversible encephalopathy syndrome and cerebrovascular constriction syndrome in the differential diagnosis of post-partum headaches. Rev Esp Anestesiol Reanim 63: 116-121.
5. Ural UM, Balik G, Sentürk S, Ustüner I, Cobanoğlu U, et al. (2014) Posterior reversible encephalopathy syndrome in a postpartum pre-eclamptic woman without seizure. Case Rep Obstet Gynecol.
6. Hasbún J, Rodríguez M, Miranda G (2012) Síndrome de encefalopatía posterior reversible (PRES) en dos casos de eclampsia. Rev Chil Neuro-psiquiatr 50: 35-41.
7. Nielsen LH, Gron BS, Ovesen PG (2015) Posterior reversible encephalopathy syndrome postpartum. Clin Case Rep 3: 266-270.
8. Pedraza R, Marik PE, Varon J (2009) Posterior reversible encephalopathy syndrome: A review. Crit Care Shock 12:135-143.
9. Cipolla MJ (2007) Cerebrovascular function in pregnancy and eclampsia. Hypertension 50: 14-24.
10. Lim SY, Evangelou N, Jürens S (2014) Postpartum headache: Diagnostic considerations. Pract Neurol 14: 92-99.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)