1061
Views & Citations61
Likes & Shares
Background: The utilization of Computed tomography (CT)
has exponentially increased since its inception, providing faster and more
reliable results. However, there are several downsides which include: increased
radiation exposure to patient, increased health care cost and increased output
times at a radiology department. In the acute setting for example, the
Emergency Department (ED), the increase use of this modality therefore has
widespread ramifications. Therefore, more selective use of CT in the ED can
reduce the number of unnecessary scans done, resulting in a reduction in
healthcare cost. Clinical decision guidelines to assist physicians in ordering
head CT for these patients are therefore needed. The objective of this study
was to determine the clinical predictors of abnormal imaging findings among
those patients in the ED with non-traumatic history who underwent head CT at
the EWMSC. Currently, such data does not exist locally and this study can serve
as a foundation for creation of protocols and guidelines. The results can also
be compared to international findings.
Method: Ethical approval was obtained and a
retrospective analysis of the non-contrast head CT examinations done for
patients who presented to the ED from June 1st to August 31st, 2016, analyzed.
The patients were adult patients with non-traumatic history or no known
intracranial pathology. A multivariable logistic regression was performed with
correlation of each of the variables with predicting abnormal findings
expressed as an adjusted odd ratio (OR) and confidence interval of 95% (CI).
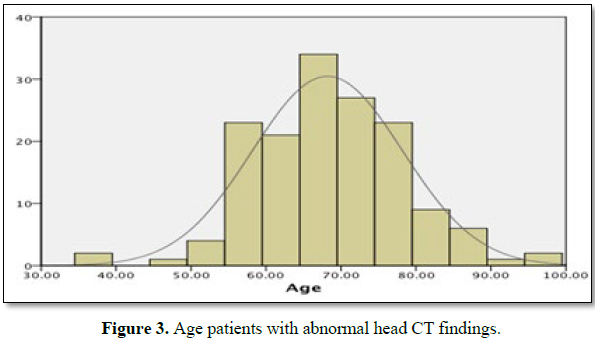
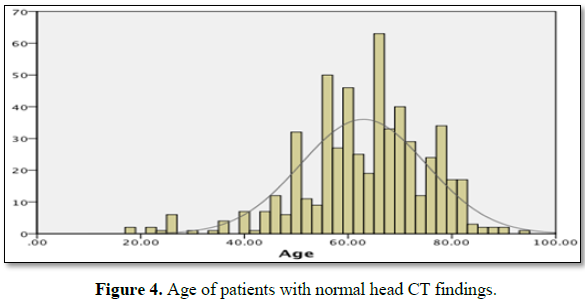
Results: Of 2090 unenhanced Head CT images done at
the EWMSC between June 1st to August 31st, 2016, 701 were eligible for this
study. Only 153 (21.8%) revealed any abnormalities. Five predictors of abnormal
findings were identified and they included age (adjusted OR 1.18; 95% CI: 1.09,
1.29), elevated blood pressure (OR: 2.23: 95% CI 1.15, 4.34), posterior fossa
symptoms (OR: 4.12; 95% CI: 2.29, 7.43) focal neurologic deficit (OR: 5.40; 95%
CI: 3.91, 7.48) and altered mental status (OR: 2.33; 95% CI: 1.67, 3.26).
Conclusion: Five variables were independent predictors
of abnormal findings among ED patients who were referred for head CT for
non-trauma related indications: age>65, elevated blood pressure, altered
mental status, posterior fossa symptoms and focal neurological deficits.
Levels of evidence: III
Study type: Retrospective study, economic and value
based evaluation.
Keywords: Non-contrast
head CT, Emergency department
INTRODUCTION
Since the development of the first generation
CT in 1972, the use of CT has demonstrated an exponential increase. It was been
estimated that in the United States of America about 70 million CT examinations
are done annually [1,2]. Research has shown a six fold increase in CT utilization
was demonstrated from the period 1995 to 2007 [3]. It has been postulated that
this is due by increased frequency of CT scanning with a smaller fraction being
attributable to increased patient load [3]. Faster and more accurate diagnosis with an increased awareness of malpractice
CT scans are non-invasive and can proved
faster and more accurate results and can be protective in cases of medicolegal
litigation [9-11]. However, there are several downsides such as the exposure to
radiation, increased output times leading to an increase cost and burden to an
already limited health care system. In the acute setting, the increase use of
this modality therefore has widespread ramifications.
Around 60-70% of all CT requests from our
Radiology Department are from the Emergency Department. In 2005, it was
estimated that the average cost of a non-enhancement Head CT to the institution
(EWMSC) was $1,200 TTD (equivalent to $176 USD) in comparison to a typical
hospital in the United States which ranges from $400-$800 USD [12,13].
A recent study performed at the EWMSC by
Rampersad et al., analyzed Head CT studies in patients with head trauma.
However, there has been no study to analyze the referral patterns and outcomes
of CT Brain in patients without trauma.
Few studies have postulated scans in patients
with no trauma are of low diagnostic yield; however it was limited to the
characteristics [14-22]. It was seen that, almost all non-trauma patients with
abnormal findings demonstrated a positive neurologic examinations and most of
who were over the age of 65 [20-22].
More robust data in identifying clinical predictors of finding an
abnormality in head CT findings is therefore lacking.
The creation of guidelines to aid the
Emergency doctors to more efficiently and accurately refers patients for CT
scanning and therefore has the potential to reduce the burden and reduce the
cost of health care.
There are several decision aids that exist
which provide guidelines to reduce the utilization of radiation in low-risk
patients and include the National Emergency X-Radiography Utilization Study,
the Canadian Cervical Spine Rule and the Ottawa Foot and Ankle Rules [23-25].
There are even less aids for the use of CT, one example of which is the
Canadian Head CT Rule [12]. The importance of more selective importance in
today’s medical practice where the threshold for the use of CT has decreased
and often it is increasingly used among healthy individuals in whom the
potential harmful effects and cost/burden to health care resources may outweigh
the benefits of the study.
The main objective of our research was to pin
point those symptoms that are mostly like to predict an abnormality in an
unenhanced CT Brain among those patients without trauma who presented to the
EWMSC.
Local data regarding these referral patterns
does not exist in the literature and this study provides a starting ground for
further revision of protocols and comparison across other radiology departments
both locally and regionally.
METHODS
Study population
Data was collected after approval from the
ethics board and was done at the EWMSC Radiology Department, a tertiary health
care facility and subspecialty referral center.
The department also provided the advantage of
a picture archiving and communications system and Radiology information system
that made data collection more efficient. Consecutive Head CT examinations
performed on patients from the Emergency Department from June 1st to August 31st,
2016 were collected.
Patients that were excluded from this study
include those who:
·
were not referred by the EWMSC ED
·
were less than 18 years old
·
had an history of trauma
·
had known current intracranial pathology
·
had a known history of brain
tumor/lesion- either primary or metastatic in nature
Those requisitions that did not state any of
the clinical predictors of interest were also excluded.
The CT studies were interpreted by radiology
residents and certified by local board-certified radiologists.
Data collection
Data was categorized based on demographic and
clinical symptoms into the following variables:
·
Age
·
Sex- Male/Female
·
Presence of headache or signs of
meningism
·
Vomiting and/or nausea
·
Altered mental status
·
Focal neurologic deficits
·
Posterior fossa symptoms
·
Seizures
·
Presence of seizure disorder such as
epilepsy
·
Presence of a malignancy
·
Illicit drug use, including alcohol
·
Fever or elevated leukocytes
·
Altered blood pressure
·
Altered coagulation profile
·
Weakness and/or fatigue
Primary outcome
The main outcome was abnormal finding on an unenhanced
head CT image and includes the following:
·
Acute intra or extra cranial hemorrhage
·
Ischemic infarction, either acute or
sub-acute
·
Mass lesion
Information was obtained using the official
reports on head CT examinations accessed on the PACS.
Sample size
determination
About 10 outcomes were required for each of
the variable used in logistic regression model in order to avoid over-fitting
[26,27].
We aimed to examine 15 candidate independent
variables with abnormal findings on head CT scans. Therefore, at least 150 CT
findings with abnormal findings were required.
DATA ANALYSIS
The total data set was collected between June
1st to August 31st, 2016. August 31st, 2016,
was chosen as a cut-off date because this provided a data set that had the
minimum requirement of 150 head CT images showing an abnormality.
Standard descriptive and multivariate
logistic regression analyses were performed using the 15 candidate variables.
The strength of each association of each variable with the primary outcome was
expressed as an adjusted odds ratio and 95% confidence interval. A P value of
0.05 suggested statistical significance. SPSS version 23.0 (IBM, San Jose,
Calif) was used in analysis.
RESULTS
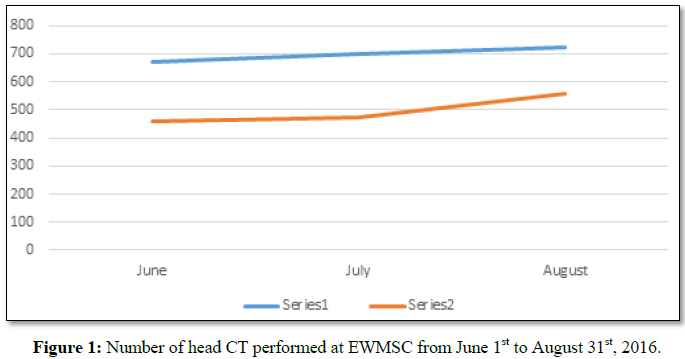
From June 1st and August 31st,
2016, 2090 CT examinations were identified on our PACS. Of these, 599 (28.7%)
were not from the ED and 103 were pediatric patients (4.9%). Patients who had
insufficient data or incomplete request forms amounted to 108 patients or 5.2%.
470 patients (22.4%) had a history of trauma and 109 patients (5.2%) had a
known intracranial pathology. Only 701 CT (33.5%) of the total met our
eligibility criteria (Figure 1 and Table
1).
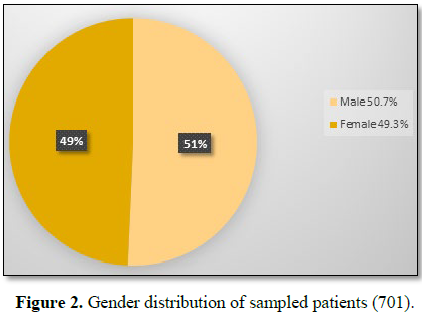
Apart from age 9 (over 18) and gender/sex, 13
variables were assessed in our study population (Figures 2-5 and Table 2).
The following 5 variables were identified as
independent variables (Tables 3 and 4):
Abnormal
findings were less apparent (8 of 98 [8.1%]) in patients who presented with a
seizure (145 of 603 [24%]). Furthermore, there were no abnormal findings in
those who had a known seizure disorder such as epilepsy.
If patients had been scanned only if they had
one or more of the five independent clinical predictors regardless of age a
sensitivity of 94.2% (144 of 153 images with positive findings). The number of
examinations to would be reduced by 69.9% o (490 of 701). A small increase in
sensitivity to 96.0% (147 of 275) would have been achieved if patients over the
age of 70 were scanned.
DISCUSSION
In our research, the following independent
clinical predictors of abnormal CT findings were found after analyzing the
images and reports of 701 patients: age older than 65 years, altered/elevated
blood pressure at presentation, focal neurologic deficit, altered mental status
and the presence of posterior fossa symptoms.
To determine to true effect of this
prediction rule there will be a prospectively study will be needed; however
this preliminary analysis suggested that the number of CT examinations
performed could have been reduced by almost 20% of the original number.
These results are comparable to the Canadian
Assessment of Tomography for Childhood Head injury (CATCH) [28]. It also
compares favorably with the Canadian CT head rule developed by Papa et al.
[29].
This study does not did not provide any
correlation between an abnormal Head CT finding with the following variables as
the only presenting symptom: headaches, fever and/or elevated white blood
cells, nausea or vomiting, vertigo, dizziness, seizure, seizure disorder, drug
use and/or alcohol use, history of malignancy or generalized constitutional
symptoms in patients under the age of 65 years.
In the literature, there are few studies
examine that examine non-trauma patients. These studies are typically smaller
but demonstrate that head CT examinations in this population are of low
diagnostic yield. Moreover, nearly all patients with abnormal CT findings also
had abnormal neurologic examination findings. Naughton et al. [17] determined
that only 15% had positive findings on CT.
Another study of 200 patients who presented
with acute dizziness or vertigo found no findings that could be the primary
cause [18].
Lai et al. [30] examined 300 elderly patients
with delirium and concluded that new neurologic deficits, deterioration in
consciousness, and recent history of a fall predicted abnormal CT. Several
other studies mirrored similar predictor variables (14-19, 31-32).
In our study population, several patients who
presented with headache would not have met the criteria for a Head CT. However,
one of these patients did have a non-aneurysmal subarachnoid hemorrhage (SAH).
The remainder of patients with SAH had either one or more of the 5 predictor
variables and would have qualified for a head CT. Due to the retrospective
nature of our study, all headaches were grouped into a single category as no
distinction could be made between sudden onset headaches versus those that had been
present for several days or has been increasing in severity.
Time for a headache to peak is one feature
that has echoed few studies and could be a preliminary predictor of SAH [33].
The American College of Emergency Physicians recommends that patients with
headache and demonstrable neurological deficit and those who present with new
sudden-onset severe headache should undergo urgent unenhanced head CT [34].
Such policies present a challenge. Currently Perry et al. [35] are conducting a
prospective study regarding the referral of patients with new sudden-onset
severe headache.
There was no preliminary evidence from our
study to routinely refer patients who presents solely with seizure or seizure
disorder. It was deduced in several reviews that patients who have seizures
will also have other symptoms or variable which greatly increases the
likelihood of an abnormal CT finding [36,37].
The Therapeutics and Technology Assessment
Subcommittee of the American Academy of Neurology is responsible for developing
clinical practice guidelines for the use of diagnostic test various
presentations such as seizures and aims to employ improved methodology [38]. In
their assessment in 1999, the authors investigated the probability that imaging
would lead to an acute or urgent change in management
Our work can add to this field locally
because, to our knowledge, it is the first study locally and regionally to
examine a comprehensive set of clinical features that are associated with
abnormal head CT in our patient population.
LIMITATIONS
There were several limitations in our
research. Firstly, there were no standardization in assessment and
documentation due to the retrospective nature of the study. There were some
limitations as the CT request form or requisition did not clearly state the
presence or absence of the clinical variables that were investigated. It was
assumed that a feature was not present if there were no mention of it.
Furthermore, there were no communication between the referring physician so
there was no understanding of the day to day functioning and justification of
the requisition.
There was also no standard terminology within
the CT requisitions. An example of this was seen in those referral forms that
stated “LOC” which made it unclear whether it meant “loss of consciousness” or
“altered consciousness.” To avoid such limitations categorized the requisition
under broad definitions for some predictors, such as “altered mental status”
(which could include loss of consciousness, dizziness, syncope, delirium and
amnesia). However, this had likely lowered the specificity.
Finally, our results are from a busy tertiary
academic level hospital which provides services to a large fraction of the
population and the results of our study might not be appropriate in another
clinical setting such as local health centers or non-academic urban centers.
CONCLUSION
Five variables were independent predictors of
abnormal findings among ED patients who were referred for head CT for
non-trauma-related indications: age over 65, elevated blood pressure, altered
mental status, posterior fossa symptoms and focal neurological deficits.
FURTHER
RECOMMENDATIONS
To further validate our findings, a
prospective research or validation in our population is warranted and can
reduce the number of referrals to radiology departments which can lead to a
more efficient and optimized service and potentially reduce the burden on our
limited health care resources.
1. IMV
Medical Information Division (2007) Benchmark report CT 2007. Des Plaines, Ill:
IMV Medical Information Division.
2. National
Centre for Health Statistics (2010) Health, United States, 2009 with special
feature on medical technology. U.S. Department of Health and Human Services
Website. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf.
Updated February 24, 2010.
3. Larson
DB, Johnson LW, Schnell BM, Salisbury SR, Forman HP (2011) National trends in
CT use in the emergency department: 1995-2007. Radiology 258: 164-173.
4. Boone
JM, Brunberg JA (2008) Computed tomography utilization in a tertiary care
university hospital. J Am Coll Radiol 5: 132-138.
5. Broder
J, Warshauer DM (2006) Increasing utilization of computed tomography in the
adult emergency department, 2000-2005. Emerg Radiol l3: 25-30.
6. Broder
J, Fordham LA (2007) Increasing utilization of computed tomography in the
pediatric emergency department, 2000-2006. Emerg Radiol 14: 227-232.
7. Broder
JS (2008) CT utilization: The emergency department perspective. Pediatr Radiol
38: S664-S669.
8. Sosna
J, Slasky S, Bar-ziv J (1997) Computed tomography in the emergency department.
Am J Emerg Med 15: 244-247.
9. Brenner
DJ, Hall EJ (2007) Computed tomography - An increasing source of radiation
exposure. N Engl J Med 357: 2277-2284.
10. Chen
JL, Dorfman GS, Li MC, Cronan JJ (1996) Use of computed tomography scanning
before and after sitting in an emergency department. Acad Radiol 3: 678-682.
11. Romano
S, Romano L (2010) Utilization patterns of multidetector computed tomography in
elective and emergency conditions: indications, exposure risk and diagnostic
gain. Semin Ultrasound CT MR 31: 53-56.
12. Stiell
IG, Lesiuk H, Wells GA, McKnight RD, Brison R, et al. (2001) The Canadian CT
head rule study for patients with minor head injury: Rationale, objectives and
methodology for phase I (derivation). Ann Emerg Med 38: 160-169.
13. Stein
SC, Fabbri A, Servadei F (2008) Routine serial computed tomographic scans in
mild traumatic brain injury: When are they cost-effective? J Trauma 65: 66-72.
14. Brown
G, Warren M, Williams JE, Adam EJ, Coles JA (1993) Cranial computed tomography
of elderly patients: An evaluation of its use in acute neurological
presentations. Age Ageing 22: 240-243.
15. Hirano
LA, Bogardus ST Jr, Saluja S, Leo-Summers L, Inouye SK (2006) Clinical yield of
computed tomography brain scans in older general medical patients. J Am Geriatr
Soc 54: 587-592.
16. Hardy
JE, Brennan N (2008) Computerized tomography of the brain for elderly patients
presenting to the emergency department with acute confusion. Emerg Med
Australas 20: 420-424.
17. Colledge
N, Lewis S, Mead G, Sellar R, Wardlaw J, et al. (2002) Magnetic resonance brain
imaging in people with dizziness: A comparison with non-dizzy people. J Neurol
Neurosurg Psychiatry 72: 587-589.
18. Giglio
P, Bednarczyk EM, Weiss K, Bakshi R (2005) Syncope and head CT scans in the
emergency department. Emerg Radiol 12: 44-46.
19. Kapoor
WN (1990) Evaluation and outcome of patients with syncope. Medicine (Baltimore)
69: 160-175.
20. Naughton
BJ, Moran M, Ghaly Y, Michalakes C (1997) Computed tomography scanning and delirium
in elder patients. Acad Emerg Med 4: 1107-1110.
21. Wasay
M, Dubey N, Bakshi R (2005) Dizziness and yield of emergency head CT scan: Is
it cost effective? Emerg Med J 22: 312.
22. Grossman
SA, Fischer C, Bar JL, Lipsitz LA, Mottley L, et al. (2007) The yield of head
CT in syncope: A pilot study. Intern Emerg Med 2: 46-49.
23. Hoffman
JR, Wolfson AB, Todd K, Mower WR (1998) Selective cervical spine radiography in
blunt trauma: Methodology of the National Emergency X-Radiography Utilization
Study (NEXUS). Ann Emerg Med 32: 461-469.
24. Stiell
IG, Wells GA, Vandemheen K, Clement CM, Lesiuk H, et al. (2001) The Canadian
C-spine rule for radiography in alert and stable trauma patients. JAMA 286:
1841-1848.
25. Steill
IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, et al. (1992) A study to
develop clinical decision rules for the use of radiography in acute ankle
injuries. Ann Emerg Med 21: 384-390.
26. Harrell
FE Jr, Lee KL, Califf RM, Pryor DB, Rosati RA (1984) Regression modeling
strategies for improved prognostic prediction. Stat Med 3: 143-152.
27. Laupacis
A, Sekar N, Stiell IG (1997) Clinical prediction rules. A review and suggested
modifications of methodological standards. JAMA 277: 488-494.
28. Osmond
MH, Klassen TP, Wells GA, Correll R, Jarvis A, et al. (2010) CATCH: A clinical
decision rule for the use of computed tomography in children with minor head
injury. CMAJ 182: 341-348.
29. Papa
L, Stiell IG, Clement CM, Pawlowicz A, Wolfram A, et al. (2012) Performance of
the Canadian CT head rule and the New Orleans criteria for predicting any
traumatic intracranial injury on computed tomography in a United States Level I
trauma center. Acad Emerg Med 19: 2-10.
30. Lai
MM, Wong Tin Niam DM (2012) Intracranial cause of delirium: Computed tomography
yield and predictive factors. Intern Med J 42: 422-427.
31. Lim
BL, Lim GH, Heng WJ, Seow E (2009) Clinical predictors of abnormal computed
tomography findings in patients with altered mental status. Singapore Med J 50:
885-888.
32. Al-Nsoor
NM, Mhearat AS (2010) Brain computed tomography in patients with syncope.
Neurosciences (Riyadh) 15: 105-109.
33. Breen
DP, Duncan CW, Pope AE, Gray AJ, Al-Shahi Salman R (2008) Emergency department
evaluation of sudden, severe headache. QJM 101: 435-443.
34. Huff
JS, Melnick ER, Tomaszewski CA, Thiessen ME, Jagoda AS, et al. (2014) Clinical
policy: Critical issues in the evaluation and management of adult patients
presenting to the emergency department with seizures. Ann Emerg Med 63:
437-47.e15.
35. Perry
JJ, Stiell IG, Sivilotti ML, Bullard MJ, Lee JS, et al. (2010) High risk
clinical characteristics for subarachnoid hemorrhage in patients with acute
headache: Prospective cohort study. BMJ 341: c5204.
36. Harden
CL, Huff JS, Schwartz TH, Dubinsky RM, Zimmerman RD, et al. (2007)
Reassessment: Neuroimaging in the emergency patient presenting with seizure (an
evidence-based review): Report of the Therapeutics and Technology Assessment
Subcommittee of the American Academy of Neurology. Neurology 69: 1772-1780.
37. Jagoda
A, Gupta K (2011) The emergency department evaluation of the adult patient who
presents with a first-time seizure. Emerg Med Clin North Am 29: 41-49.
38. (1996)
Practice Parameter: Neuroimaging in the emergency patient presenting with
seizure: Summary statement. Quality Standards Subcommittee of the American
Academy of Neurology in cooperation with American College of Emergency
Physicians, American Association of Neurological Surgeons, and American Society
of Neuroradiology. Neurology 47: 288-291.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Pathology and Toxicology Research
- Journal of Rheumatology Research (ISSN:2641-6999)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Advance Research on Alzheimers and Parkinsons Disease
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Allergy Research (ISSN:2642-326X)