1023
Views & Citations23
Likes & Shares
The
present perspective is a synthesis of 75 published investigations in the
setting of rechanneling of supracardiac totally anomalous pulmonary venous
connection with or without vertical vein ligation in the literature. In this
article, we review the issue of unligated/ligated vertical vein, adjustable
vertical vein ligature, routine left atrial augmentation and atrial septal
fenestration after rechanneling of supracardiac totally anomalous pulmonary
venous connection in order to decrease perioperative pulmonary hypertensive
crises, postoperative low cardiac output syndrome and mortality. Additionally,
this review attempts to address the guidelines for selective vertical vein
patency in patients with obstructive supracardiac totally anomalous pulmonary
venous connection.
Keywords: Vertical vein, Totally anomalous pulmonary
venous connection, Pulmonary hypertensive crises, Adjustable vertical vein
ligature
INTRODUCTION
Reports addressing the issue of not ligating the vertical vein
following repair of totally anomalous pulmonary venous connection, and related
postoperative hemodynamics are limited and conflicting [1-11]. Traditionally,
ligation of the vertical vein at the time of rechanneling of totally anomalous
pulmonary venous connection has been recommended to prevent the perceived
consequences of a residual left-to-right shunt [1-11]. Some investigators have
expressed concern about the occurrence of acute hepatic necrosis following
ligation of the vertical vein [12]. This concept was so ingrained in the
practice of rechanneling of totally anomalous pulmonary venous connection that
five major anatomical and pathophysiological issues of obstructive totally
anomalous pulmonary venous connection were either not well appreciated or
ignored.
METHODS
With these
deficiencies in mind, we have analysed the published literature to identify the
described instances of repaired obstructive and non-obstructive supracardiac
totally anomalous pulmonary venous connection, unligated/ligated vertical vein,
left atrial augmentation, adjustable vertical vein ligature and atrial septal
fenestration and evaluated all clinical studies describing the principles,
indications, techniques and outcomes. The search engines employed were Medline,
PubMed, Google scholar, Cochrane database and Embase. The search included
literature in all languages. This strategy yielded 75 investigations that
provided best answer to these topics. We have then synthesized all these
features to outline the rationale, issue of concern and potential future trends
of various surgical strategies of rechanneling of obstructive supracardiac
totally anomalous pulmonary venous connection in general and adjustable
vertical vein ligature in particular [1-75].
This review article
outlines the pathophysiologic mechanisms underlying totally anomalous pulmonary
venous connections and the hemodynamic consequences of leaving the vertical
vein open versus occluded following rechanneling of obstructed totally
anomalous pulmonary venous connection. With respect to drawing conclusions from
the sum total of the peer-reviewed published literature, we have attempted to
interpret the results utilizing standardized definitions of key elements as
under:
Preoperative
pulmonary venous drainage was considered obstructive if there was
echocardiographic or angiographic data that indicated: (i) a significant
gradient between the pulmonary veins and their point of drainage (flow
acceleration >2 m/s by echocardiography or pressure gradient >4 mm Hg),
(ii) monophasic and continuous Doppler flow pattern in the individual pulmonary
veins, the pulmonary venous confluence or the vertical vein, or (iii)
angiographically evident localized reduction in a single pulmonary vein
diameter of 50% or more. Pulmonary hypertension was defined as a right-to-left
ventricular systolic pressure ratio of 0.6. According to systemic pulmonary
artery pressure (SPAP), as measured by cardiac catheterization or on
echocardiography on the basis of the velocity of tricuspid regurgitation,
pulmonary hypertension was graded as follows: none (SPAP<18 mm Hg), mild
(SPAP 19-30 mm Hg), moderate (SPAP 31-50 mm Hg), or severe (SPAP >50 mm Hg).
Isolated or simple TAPVC was diagnosed if the patient had TAPVC in association
with a secundum atrial septal defect (ASD), a patent ductus arteriosus or both.
An operation was classified as an emergency if the patient was taken to the
operating room within the first 24 h after arrival at the hospital for
hemodynamic or ventilatory compromise.
In the published
literature, the indications of preoperative cardiac catheterizations are: (1)
anatomy that is unresolved by echocardiography, (2) characterization of the
primary venous obstruction, or (3) exclusion of major associated cardiac
anomalies that required delineation or intervention.
Low cardiac output
syndrome in repaired TAPVC was diagnosed if the patient required inotropic
support (dopamine at 4-10 µg/[kg - min], dobutamine at 5-10 µg/[kg - min],
epinephrine at 0.01-0.1 µg[kg - min], milrinone at 50 µg/kg intravenous bolus
followed by 0.375-0.75 µg/[kg – min]), either isolated or in combination in the
operating room or in the intensive care unit to maintain stable hemodynamics in
the absence of residual structural lesions and mechanical external compression
after correction of all electrolytes or blood gas abnormalities and after
adjustment of the preload to its optimal value. Low-output syndrome was also
diagnosed if there was an increasing requirement of the previously mentioned
inotropes along with afterload reduction with sodium nitroprusside. Patients
who received less than 4 µg/(kg - min) dopamine to increase renal perfusion
were not considered to have low output syndrome.
Invasive monitoring
to measure cardiac output directly (thermodilution catheter, PA pressure line
and thermistors) is cumbersome and hazardous in children and generally avoided,
except in complex cases. Generally, the intracardiac monitoring is limited to
right atrial, left atrial and pulmonary artery pressure lines.
Accordingly, under
the definition of low output syndrome after repaired TAPVC, an integration of
relevant clinical, laboratory and bedside echocardiographic criteria was used.
The criteria for diagnosis were as follows: cold extremities, absent pedal
pulses, decreased toe temperature, reduced systolic pressure, impaired renal
function and oliguria (<1.0 mL/[kg – h]), metabolic acidosis, increased
serum lactate levels (>2 mmol/L for >2 h), low mixed venous oxygen
saturation (<50%) and blunted sensorium in the absence of residual
anastomotic or pulmonary venous obstruction.
CONCEPT
In an attempt to
address these controversial issues we have developed a conceptual framework in
the context of clinical phenotypes.
According to the age at presentation: Infants
versus adults
The differences
noted between infants and adults undergoing rechanneling of supracardiac
totally anomalous pulmonary venous connection provide important insight into
factors associated with adverse outcomes and mortality. For instance, an
obstructive totally anomalous pulmonary venous connection has a greater
prognostic role in pediatric patients than in adults. Only few patients reach
adulthood and they usually have non-obstructive type of totally anomalous
venous connection, low pulmonary vascular resistance, normal or moderately high
pulmonary artery pressure and large left-to-right shunt [46-50].
According to the obstruction of pulmonary
venous flow: Obstructive versus non obstructive
The anatomical
factors most important in determining the clinical status of the patient
include the presence and location of a right-to-left shunt and the presence or
absence of obstruction in the pulmonary venous circuit. Published literature
documents seven sites of possible obstruction to the pulmonary venous flow in
totally anomalous pulmonary venous connection: i) compression of the vertical
vein by the left/right pulmonary artery and the left/right bronchus, ii) the
vertical vein coursed between the left pulmonary artery and the ductus
arteriosus and compressed by this “circulus vasculosus”, iii) stenosis at the
junction of pulmonary veins and the common chamber, iv) stenosis at the
insertion site of the vertical vein into the superior caval vein or the
brachiocephalic vein, v) compression of the vertical vein by the aortic arch,
vi) small sized individual pulmonary veins, and vii) a restrictive atrial
septal defect [31,45-47,53].
Subjects with
obstructive totally anomalous pulmonary venous connection present early in
infancy, with features of pulmonary edema. Those without obstruction, present with
features of large left-to-right shunt, pulmonary plethora and congestive heart
failure [31,45-47,50,53].
Ligated vs. unligated vertical vein in
supracardiac totally anomalous pulmonary venous connection
Clinical studies on
an unligated vertical vein in the setting of obstructive supracardiac totally
anomalous pulmonary venous connection are too limited and insufficient to
generate evidence-based guidelines. The vertical vein, when present is usually
ligated or divided during surgical correction of totally anomalous pulmonary
venous connection to prevent a residual left-to-right shunt [54]. As yet, there
are no specific criterions for candidate selection to maintain a patent
vertical vein and there is no consensus in the literature regarding the fate of
unligated vertical vein following repair of totally anomalous pulmonary venous
connection. Literature documents clear anecdotal cases of spontaneous
involution of the anomalous vertical vein at one end of the spectrum and a
functioning conduit with shunt induced cardiac failure at the other end
[34-44].
In order to allow
the left heart to adopt and maintain adequate cardiac output, various surgical
techniques have been adopted to construct an unrestrictive anastomosis between
the common pulmonary venous chamber and left atrium [44,49]. Historically,
ligation or interruption of the vertical vein and incorporation of the vertical
vein as part of the new anastomosis have been described [48]. Several
investigators have developed ingenious surgical techniques by creating a large
tension-free anastomosis, maintaining precise geometric alignment of the common
pulmonary venous chamber with the left atrium, thus avoiding distortion and
rotation of the pulmonary veins. Innovative suture less techniques and use of
absorbable polydioxanone sutures have been described at reducing the recurrence
of pulmonary vein stenosis [55-61].
In 2007, the
authors documented their observations that acute vertical vein ligation
resulted in elevated left atrial pressure and left ventricular function and
cardiac output are negatively impacted suggesting that for a period of time the
small, poorly compliant left ventricle of the patient with obstructive totally
anomalous pulmonary venous connection was unable to maintain adequate cardiac output
[34,62]. Indeed, it is routine to see elevated left atrial pressure and
pulmonary artery pressure combined with systemic hypotension and decreased
cardiac output after weaning from cardiopulmonary bypass in patients with
obstructive totally anomalous pulmonary venous connection [34,62]. Since the
pulmonary veins/capillaries do not have any valves, any rise in left atrial
pressure will lead to pulmonary hypertension. The postoperative course targets
management of these issues and occasionally extracorporeal membrane oxygenation
is necessary while the pulmonary vascular bed recovers and left ventricular
compliance improves [63,64]. The time course of this adjustment is variable. It
is conjectured that there is a feedback loop whereby acute elevation of left
atrial pressure results in excessive pulmonary arteriolar constriction with
out-of-proportion pulmonary hypertensive response that further exacerbates the
low cardiac output state caused by a poorly compliant left ventricle [65].
We postulated that
a patent vertical vein may function as a temporary reservoir for pulmonary
venous blood after repair of totally anomalous pulmonary venous connection,
volume unloading the small, non-compliant, left-sided cardiac chambers until
they grow and adopt to increased flow demands [13-20,34]. Not all investigators
have accepted these findings or utilized these techniques. In order to test the
above-mentioned postulates to reduce the perioperative mortality and morbidity,
the authors initiated a programme of routine adjustable vertical vein ligature
in patients with obstructive totally anomalous pulmonary venous connection with
post bypass systemic or suprasystemic pulmonary arterial hypertension [34,62].
The unligated
vertical vein served as a temporary “pop off” valve in the event of pulmonary
hypertensive crises. This strategy allowed a more gradual occlusion of the
vertical vein so that acute elevation of the left atrial pressure was avoided,
albeit with some period of pulmonary over circulation and elevated right-sided
filling pressure, thereby tiding over the postoperative phase of heightened
pulmonary vasoreactivity. Such a band allowed easy tightening in increments,
with gradual increase of ventricular afterload without the need for multiple
reoperations [34,62-65].
James S Tweddell in
his editorial on the issue of vertical vein ligature revisited some
observations during the early years of cardiology and cardiac intervention
[65]. In 1916, Lutembacher [66] described the impact of an atrial septal defect
on acquired mitral stenosis by trading mild elevation of right atrial pressure
and pulmonary over circulation for acute elevation of left atrial pressure. In
1949, Bland and Sweet [67] anastomosed azygous vein to pulmonary vein to
improve the functional status of patients with critical rheumatic mitral
stenosis permitting spillover of the congested pulmonary veins into the
capacious systemic venous system. Revisiting these observations of Cope et al.
[2], Chowdhury [34,62], Lutembacher [66] and Bland [68] suggest that the
systemic venous system and pulmonary
vasculature can accommodate the excess volume and limit the impact of excessive
left atrial pressure.
Adjustable vertical vein ligation
Based on the
literature and reasoning cited above, the authors embarked on a programme of
routine adjustable vertical vein ligation in patients with obstructive totally
anomalous pulmonary venous connection with post-bypass systemic or
suprasystemic pulmonary arterial hypertension and published the technical
details and preliminary results in Cardiology in the Young [62]. Thus, there
were seven forces driving our criterions for selection of patients whose
vertical vein was kept patent after rechanneling of totally anomalous pulmonary
venous connection:
i.
The desire to
reduce the pulmonary artery pressure in the perioperative period after
achieving an adequate-sized, unrestrictive anastomosis along with
pharmacological manipulations.
ii.
The desire to
reduce pulmonary hypertensive crises, low cardiac output, and hospital
mortality following repair of totally anomalous pulmonary venous connection
with pulmonary hypertension.
iii.
The desire
that the unligated vertical vein may function as a temporary venous reservoir
for pulmonary venous blood, volume unloading the small non-compliant left-sided
cardiac chambers until they are able to grow and adapt to the requisite flow
demands.
iv.
The desire
that the unligated vertical vein may serve as a temporary “pop-off” valve in
the event of pulmonary hypertensive crises and thereafter the same may be
subjected to a gradual process of occlusion.
v.
The desire to
gradually tighten or loosen the ligature under optimal physiologic conditions,
once the disease-related/bypass-related pulmonary vasoreactivity disappears.
vi.
The desire to
gradually increase the ventricular afterload without causing unstable
hemodynamics under optimal physiologic conditions, and
vii.
The desire to
occlude the vertical vein in the event of a significant left-to-right shunt and
right heart failure without re-sternotomy or thoracotomy [34,62].
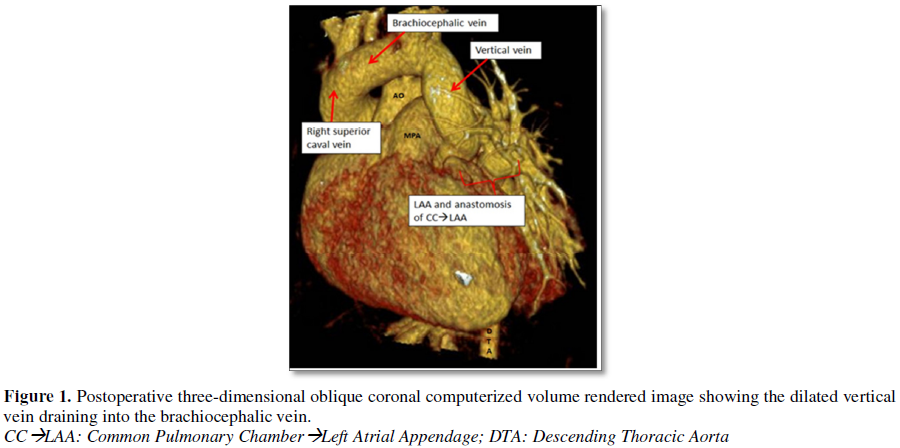
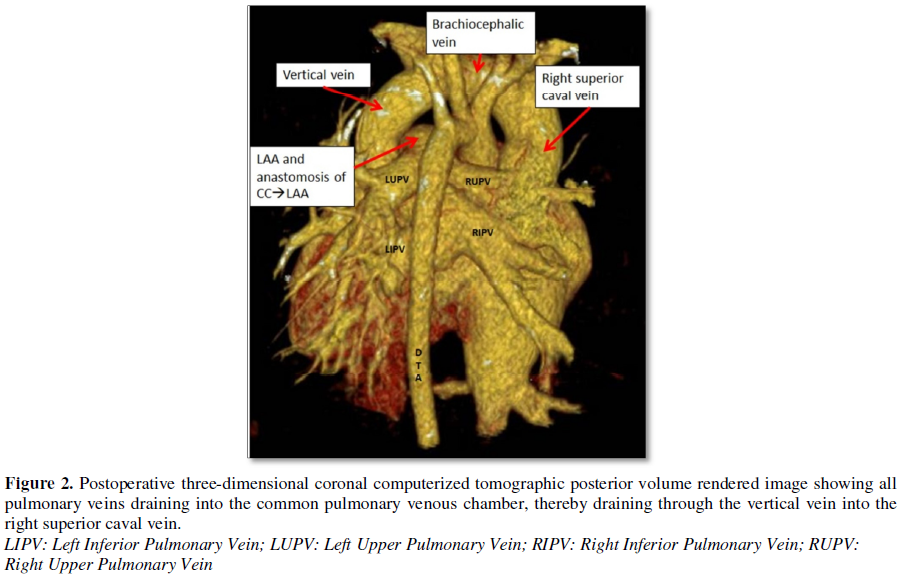
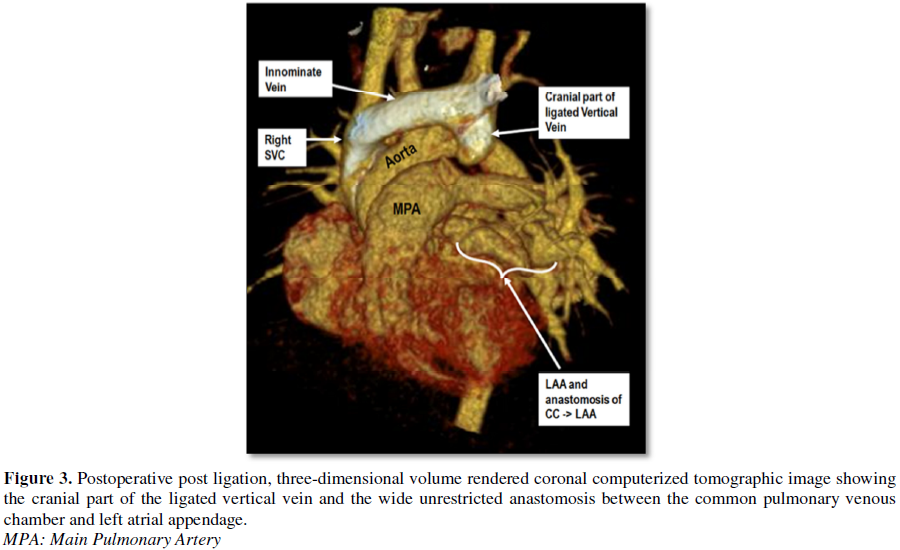
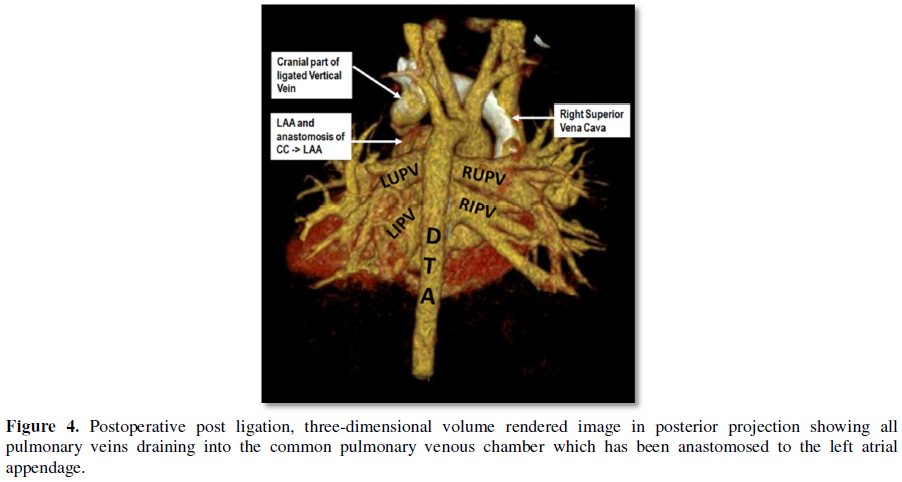
Postoperatively, we
performed computed tomographic angiography on all patients at varying time
intervals during follow-up and demonstrated wide, unrestricted anastomosis
between the common pulmonary venous chamber and left atrial appendage, absence
of flow through the vertical vein and ruled out distortion at the left superior
pulmonary vein and left brachiocephalic vein (Figures 1-4) [34,62].
Routine left atrial augmentation
As described
earlier, the left sided chambers are smaller than normal and the left atrium
lacks both normal compliance and reservoir function in totally anomalous
pulmonary venous connection [13-22]. In order to allow the left heart to adopt
and maintain adequate cardiac output, we have used a redundant Dacron patch for
interatrial septum, deviating the same to the enlarged right atrium and have
incorporated part of the vertical vein to achieve structural alignment and
augmentation of the left atrial cavity [34,62]. The concept of enlarging the
left atrium is almost similar to that described by Cooley and colleagues except
that in our patients, we achieved it by excising the floor of the fossa ovalis
and utilizing a Dacron patch graft to close the atrial septal defect and
enlarge the left atrium [69,70]. The two-patch technique of left atrial
enlargement has been popularized by Corno et al. [71]. Subsequently, several
investigators have demonstrated increased incidence of supraventricular
arrhythmias due to the use of a transverse right atrial incision and division
of the supraventricular crest [71]. We have not used this technique.
Interatrial septal fenestration
Traditionally, an
intentional atrial septal fenestration is created permitting the “spill-over”
or “pop-off” in the setting of postoperative right ventricular dysfunction
following intracardiac repair of tetralogy of Fallot, pulmonary atresia,
Ebstein’s anomaly, Rastelli’s operation and one and one-half ventricular repair
[34,62]. During episodes of pulmonary hypertensive crises with limited right
ventricular output and an elevated central venous pressure, a fenestrated
atrial septal patch permitted right-to-left shunting; increasing left
ventricular preload and cardiac output albeit with mild desaturation. A review
of the literature on this topic reveals that it can be performed relatively
safely and patients do reasonably well at follow-up. Since 2000, it has been
the author’s practice to perform atrial septal fenestration in patients with
obstructive supracardiac and infracardiac totally anomalous pulmonary venous
connection [34,62].
Thus, the unligated
vertical vein in conjunction with left atrial augmentation and a calibrated
atrial septal fenestration, decompressed the small left atrium after repair,
equalized the left atrial and central venous pressure and was the automatic
choice to avoid a dismal outcome in the perioperative period [34,62].
Introduction of
phenoxybenzamine in the management of pulmonary hypertensive crisis, use of
ultrafiltration to remove excess lung water and delayed sternal closure are
additional factors for reduced perioperative mortality in recent years [34-50].
CONCERNS
The technical
aspects of rechanneling of supracardiac totally anomalous pulmonary venous
connection, left atrial augmentation using a Dacron polyster fabric, atrial
septal fenestration and adjustable vertical vein ligature along with operative
pictures have previously been enumerated in detail in our earlier publication
and are not repeated here [62].
An initial concern
about this technique was the possibility of distortion of the left upper
pulmonary vein and left brachiocephalic vein. To address these concerns, we
have performed the following maneuvers: (i) we threaded the loop ligature
through a polytetrafluoroethylene felt and secured the same with the adventitia
of the vertical vein to prevent its displacement, and (ii) both the arms of the
silk suture were then brought out through the second left intercostal space
away from the sternotomy incision, perpendicular to the vertical vein ensuring
a vertical straight lie, avoiding subsequent distortion or occlusion of the
left superior pulmonary and brachiocephalic veins [62].
The second concern
of an unligated vertical vein is the change of the shunting pattern from the brachiocephalic
vein to the left atrium via the vertical vein causing cardiac failure. In our
initial investigation, 11 patients with obstructive totally anomalous pulmonary
venous connection with an unligated vertical vein continued to have tachypnoea
and right heart failure between 1 to 2 postoperative weeks. The vertical vein
was subsequently ligated through re-sternotomy on 4 patients, left
anterolateral thoracotomy in 2 patients and adjustable vertical vein ligature
in 5 patients. Subsequently, all patients are managed by using an adjustable
vertical vein ligature. Similar experience have been documented by other
investigators [3,4].
In our previous
investigation, autopsy findings on 4 patients revealed a small pulmonary venous
confluence, diffuse hypoplasia, intimal hypertrophy, increased pulmonary
vascular medial thickness, pulmonary lymphangiectasia and interstitial
emphysema [34]. On the basis of these observations, we speculate that the
medial and intimal changes seen in preoperative obstruction may predispose
towards the development of intrinsic pulmonary vein stenosis. We concur with
the observations of other investigators that an unligated vertical vein in this
subset of patients with co-existing pulmonary arteriopathy exerts an unfavorable
effect on the morbidity and surgical outcome despite adequate pulmonary venous
decompression [24-32]. Given the bleak prognosis for these patients,
alternative management strategies like lung transplantation may perhaps be
considered [72-74].
One important
finding of our investigation, given their age at the time of surgery, is the
occurrence of suprasystemic pulmonary arterial pressure in our patients
subsequent to weaning from bypass. Overall, one hundred and thirteen (78.4%)
patients were more than one month of age. This is in contrast to the situation
in most western countries, where more than half of patients undergo surgery
before one month of age. In our earlier publication, we demonstrated that late
referral and late presentation lead to the development of severe pulmonary
hypertension, a prolonged period of malnutrition and ultimately cardiac cohexia
[34]. These factors predispose them to pulmonary infection, sepsis,
postoperative pulmonary hemorrhage, and unfavorable reactions to stresses such
as cardiopulmonary bypass and postoperative events [34,62].
RESULTS
Cope et al. [2] in 1997 reported 4 patients
of repaired obstructive supracardiac totally anomalous pulmonary venous
connection and unligated vertical vein, aged between 1 day to 5 years. At a
range of 1 day to 106 months after operation, echocardiography failed to reveal
flow in any of the unligated vertical vein. They concluded that vertical vein
should be left unligated in obstructive totally anomalous pulmonary venous
connection [2].
Caspi et al. [3] in
2001 reported 12 patients with a mean age at operation of 21 days and standard
deviation of 8 days, weighing between 3 and 4 kg with supracardiac totally
anomalous pulmonary venous connection. Nine patients had obstructive and 3
patients had unobstructive drainage. Three patients with obstructive totally
anomalous pulmonary venous connection had an unligated vertical vein. All
patients had a 5-0 polypropylene purse string suture around the vertical vein
at the junction with the brachiocephalic vein. All patients underwent closure
of the vertical vein in intensive care unit by tightening the snare. They
concluded that a patent vertical vein has favorable effects on the morbidity
and postoperative outcome [3].
Shah et al. [4] in
2000 reported 2 patients aged 2.5 months and 2 months, weighing 3.5 kilogram
and 4.0 kg respectively with repaired obstructive supracardiac totally
anomalous pulmonary venous connection with post bypass suprasystemic pulmonary
artery pressure and unligated vertical vein. Both patients survived the
operation. Both the patients developed symptoms of left-to-right shunt and
cardiac catheterisation demonstrated widely patent vertical vein. Both
underwent delayed successful vertical vein ligation and the author recommended
non-ligation in obstructive totally anomalous pulmonary venous connection [4].
Kumar et al. [9] in
2001 documented four patients aged between 5 and 80 days, weighing between 3.0
and 4.5 kg undergoing rechanneling of obstructive totally anomalous pulmonary
venous connection. Three patients with repaired supracardiac and one patient
with infracardiac drainage had an unligated vertical vein. Cardiac
catheterization between 6 months to 2 years after surgery demonstrated widely
patent vertical vein in all of them and these investigators did not support
elective non-ligation of the vertical vein at the time of initial surgery [9].
Saritas et al. [10]
in 2011 reported 14 patients with obstructive totally anomalous pulmonary
venous connection with a mean age of 3.8 ± 2.1 months and mean body weight of
4.4 ± 1.1 kg. All patients had an unligated vertical vein at operation. At a
mean follow up of 48 ± 36 months, the vertical vein in two patients was closed
surgically and in one patient with high pulmonary artery pressure and pulmonary
vascular resistance, it closed spontaneously. These authors concluded that
patients with obstructive totally anomalous pulmonary venous connection benefit
from intact vertical vein in the postoperative period. Since they have left
chambers with poor compliance [10].
Zhao et al. [6] in
2015 reported 77 patients of supracardiac totally anomalous pulmonary venous
connection with age ranging from 27 days to 44 years, with a mean of 8.5 and
standard deviation of 7 years. Twenty patients with an unligated vertical vein
were followed up from day one to five years. Eight patients had spontaneous
closure and in 12 patients, the vertical vein remained patent. They recommended
patent vertical vein in obstructive totally anomalous pulmonary venous
connection [6].
On the other hand
in the study reported by Kelle et al. [8] in 2010 on 39 patients of obstructive
supracardiac totally anomalous pulmonary venous connection with age ranging
from 0 to 1.7 years and a median age of 14.6 days. Their weight was ranging
between 1.3 and 10 kg with a median weight of 3.5 kg. 22 patients had
obstructive supracardiac totally anomalous pulmonary venous connection. The
vertical vein was ligated in all patients and postoperative pulmonary
hypertension was managed by nitric oxide therapy and conventional ventilator
management strategies with a mortality rate of 30.7%. These authors advised
ligation of vertical vein in all patients of obstructive and non-obstructive
supracardiac totally anomalous pulmonary venous connection [8].
In our initial
investigations on 48 patients undergoing rechanneling of totally anomalous
pulmonary venous connection between 1997 and 2006, 27 (46.5%) patients did not
undergo vertical vein ligation [34]. Contrary to the report by Cope et al.
[2,34], in which patent venous pathway atrophied, 11 of 23 survivors of
obstructive supracardiac totally anomalous pulmonary venous connection allowed
symptoms of a large left-to-right shunt through the unligated vertical vein
requiring delayed closure of the vertical vein in all cases. Although delayed
closure of the vertical vein was successful in all cases, with concomitant
elevation of pulmonary artery pressure, it was attended by extremely high left
atrial pressure in six patients and proved a difficult postoperative challenge.
These findings were suggestive of a relatively small, non-compliant,
dysfunctional left-sided chamber [34].
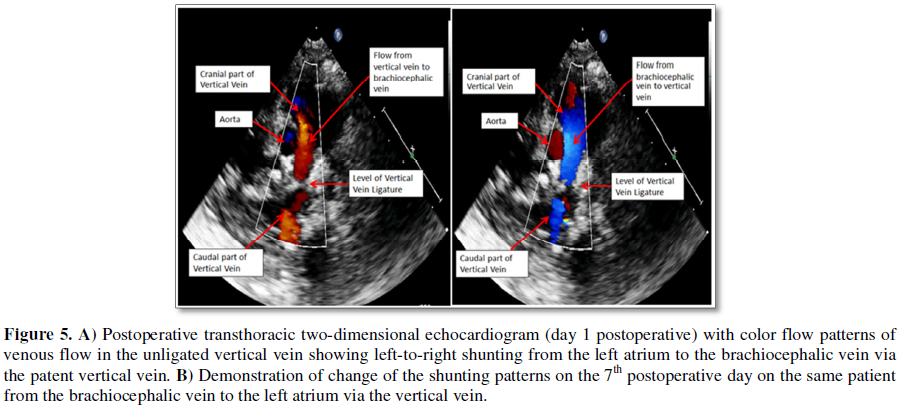
Subsequently, in
2007 we introduced the concept of adjustable vertical vein ligation in the
setting of obstructive supracardiac totally anomalous pulmonary venous
connection with the aims and objectives as narrated above [62]. We demonstrated
that the unligated vertical vein during repair of obstructive totally anomalous
pulmonary venous connection is associated with decreased episodes of pulmonary
hypertensive crisis, postoperative low cardiac output syndrome, lessened
duration of ventilation and inotropic support, provided early normalization of
hemodynamic and decreased in hospital mortality. There were no late deaths. At
a mean follow-up of 33.34 ± 29.88 months, median, 30 months, the actuarial
survivals were 92.6% ± 0.05% in the unligated category and 71% ± 0.08% for the
ligated category (p=0.03) [34,62]. All patients underwent serial
cross-sectional and Doppler echocardiographic evaluation in the postoperative
period and gradual process of vertical vein ligation at varying time intervals
between 5 and 25 days, as soon as right-to-left shunting through the vertical
vein disappeared (Figures 5A and 5B). None required anti-failure cardiac
medications [34,62].
Whether an
adjustable vertical vein ligature with concomitant rechanneling of supracardiac
totally anomalous pulmonary venous connection is advantageous over the
traditional concept of routine vertical vein ligation is a subject of debate
[34,62]. Since all investigators and surgeons have not accepted these findings
or utilized these techniques, the answer to the above postulates and
observations is forthcoming.
It is pertinent to
state that a persistent left-to-right shunt and right heart failure through an
unligated vertical vein does not necessarily relegate a patient to a second
stage operation and does not warrant modification of our selection criteria for
the unligated vertical vein. They may be candidates for adjustable vertical
vein ligature or percutaneous angiographic vertical vein embolization [75].
The mechanisms
causing heightened pulmonary vasoreactivity following repair of totally
anomalous pulmonary venous connection are multifactorial, and may reflect
release of platelet-activating factors, endothelin and arachidonic acid
metabolites from pulmonary endothelial cells, decreased ratio of prostacyclin
to thromboxane and a decline or absence of acetylcholine responsiveness
[34-50]. Many agents have been advanced as being optimal on the grounds that
they selectively reduce pulmonary vascular resistance, but few do so, and no
clearly superior one has been identified. Therefore, in the authors’ centre, a
varying combination of fentanyl, hyperventilation, correction of acidosis,
inhaled nitric oxide, sodium nitroprusside and phenoxybenzamine were used to
manage pulmonary hypertensive crises [34,62].
EXPLORING THE UNKNOWNS: FUTURE DIRECTIONS
This short
communication is not meant in any way to convince those surgeons satisfied with
their own methods of rechanneling of totally anomalous pulmonary venous
connection. Rather it hopes to point out that a patent vertical vein is
beneficial in the setting of totally anomalous pulmonary venous connection with
more than moderate pulmonary arterial hypertension.
A careful
quantitative evaluation of the preoperative morphologic and physiologic
characteristics of both left and right-sided chambers for all patients with
obstructive totally anomalous pulmonary venous connection could then be used to
determine whether and under what left heart conditions, leaving vertical vein
patent is beneficial. Such information would be welcome and noteworthy. Nothing
in the literature even remotely addresses the issue of making a quantitative
assessment of the left side of the heart that can be used to objectively decide
between the surgical options. Indeed, when one examines the underlying
concepts, it is clear that there are new concerns and basic questions that
await resolution by careful investigation only after its basic physiology is
better understood will its potential benefit be realized.
In our study, the
occurrence of systemic or suprasystemic pulmonary artery pressure on snaring
the vertical vein was the determining factor for leaving the vertical vein open
[34,62]. To properly test the hypothesis that “vertical vein ligation results
in inferior outcome and non-ligation in selected subsets of totally anomalous
pulmonary venous connection results in superior outcome”, a
multi-institutional, prospective randomized trial of ligation vs. non-ligation
would be necessary and would be the last refuge for those who cannot accept the
conflicting complex findings of the anatomy and pathophysiology of obstructive
totally anomalous pulmonary venous connection.
These types of
trials are challenging due to small sample sizes, heterogeneity of the
underlying congenital heart disease and exclusion of sicker patients. Perhaps
one of the greatest challenges in designing such trials is the selection of
appropriate end points. End points must include not only cardiac quantifiable
end points (such as pulmonary vein sizes, pulmonary venous chamber and left
heart dimensions) but also specific pulmonary vascular obstructive changes such
as indexed pulmonary vascular disease and neurocognitive assessments.
We have known for a
while that creation of a large, tension-free anastomosis, precise geometric
alignment of the pulmonary venous chamber with the body of left atrial avoiding
torsion and rotation of pulmonary veins, introduction of phenoxybenzamine in
the management of pulmonary hypertensive crisis and delayed sternal closure are
the factors for reduction of perioperative mortality after repair of totally
anomalous pulmonary venous connection in recent years [34-44]. Future
publications auditing the above-mentioned issues will add nothing to our
understanding of the problem of postoperative low cardiac output syndrome. Now,
we need to identify the anatomic and physiologic issues involved in a subset of
patients with obstructive totally anomalous pulmonary venous connection. The
issues to be resolved are: a) identification of the structurally smaller left
sided chambers, b) identification of non-compliant and dysfunctional left
ventricle, c) identification of concomitant disproportionately increased
pulmonary vascular medial thickness, and finally, d) identification of
concomitant hypoplasia of the pulmonary venous system.
CONCLUSION
On the basis of the
published literature including ours enunciated in this manuscript, we conclude
that a patent, unligated vertical vein in patients with obstructive and
non-obstructive totally anomalous pulmonary venous connection with more than
moderate post cardiopulmonary bypass pulmonary arterial hypertension
facilitates reduction of pulmonary arterial pressures, thus avoiding pulmonary
hypertensive crisis and postoperative low cardiac output syndrome and
contributes to a favorable outcome. Patients who have undergone this approach
should be followed closely for a significant, persistent left-to-right shunt
and right heart failure.
The technique of
adjustable vertical vein ligature is simple, safe, effective and allows easy
tightening in increments with gradual increase of ventricular afterload without
the need for multiple operations. We submit that an increased appreciation of
an adjustable vertical vein ligature, left atrial augmentation and atrial
septal fenestration in patients with supracardiac totally anomalous pulmonary
venous connection with more than moderate pulmonary hypertension may well
contribute to improved future surgical management.
COMPLIANCE WITH ETHICAL STANDARDS
Statement of human rights/ethical approval
The authors assert
that all procedures contributing to this study comply with the ethical
standards of the relevant national guidelines on human experimentation and with
the Helsinki declaration of 1975, as revised in 2008 and has been approved by
the Institutional Research Committee.
Declaration of conflicting interests
The author(s) declared
no potential conflicts of interest with respect to the research, authorship
and/or publication of the article.
Funding
The authors
received no financial support for the research, authorship and/or publication
of this article.
1. Mustard
WT, Keith JD, Trusler GA (1962) Two stage correction of total anomalous
pulmonary venous drainage in childhood. J Thorac Cardiovasc Surg 44: 477-485.
2. Cope JT,
Banks D, McDaniel NC, Shockey KS, Nolan SP, et al. (1997) Is vertical vein
ligation necessary in repair of total anomalous pulmonary venous connection?
Ann Thorac Surg 64: 23-29.
3. Caspi J,
Pettitt TW, Fontenot EE, Stopa AR, Heck HA, et al. (2001) The beneficial
hemodynamic effects of selective patent vertical vein following repair of
obstructed total anomalous pulmonary venous drainage in infants. Eur J
Cardiothorac Surg 20: 830-834.
4. Shah MJ,
Shah S, Shankargowda S, Krishnan U, Cherian KM (2000) Left-to-right shunt: A
serious consequence of TAPVC repair without ligation of vertical vein. Ann Thorac
Surg 70: 971-973.
5. Jegier
W, Charrette E, Dobell ARC (1967) Infra-diaphragmatic anomalous pulmonary
venous drainage: Normal hemodynamics following operation in infancy.
Circulation 35: 396-400.
6. Zhao K,
Wang H, Wang Z, Zhu H, Fang M, et al. (2015) Early- and intermediate-term
results of surgical correction in 122 patients with total anomalous pulmonary
venous connection and biventricular physiology. J Cardiothorac Surg 1: 172.
7. Spray TL
(2001) Commentary: The fate of the unligated vertical vein after surgical
correction of total anomalous pulmonary venous connection in early infancy. J
Thorac Cardiovasc Surg 122: 617.
8. Kelle
AM, Backer CL, Gossett JG, Kaushal S, Mavroudis C (2010) Total anomalous
pulmonary venous connection: Results of surgical repair of 100 patients at a
single institution. J Thorac Cardiovasc Surg 139: 1387-1394.
9. Kumar
RNS, Dharmapuram AK, Rao IM, Gopalakrishnan VC, Pillai VR, et al. (2001) The
fate of the unligated vertical vein after surgical correction of total
anomalous pulmonary venous connection in early infancy. J Thorac Cardiovasc
Surg 122: 615-617.
10. Saritas
B, Celik M, Tatar T, Ozkan M, Tokel K, et al. (2011) The outcome of the
vertical vein left intact during the surgery for total anomalous pulmonary
venous connection and its effects on ventricular functions. Anadolu Kardiyol
Derg 11: 638-642.
11. Kron IL,
Cope JT (2002) Letter to the Editor: Fate of the unligated vertical vein after
surgical correction with total anomalous pulmonary venous connection in early
infancy. J Thorac Cardiovasc Surg 123: 829.
12. Katz NM,
Kirklin JW, Pacifico AD (1978) Concepts and practices in surgery for total
anomalous pulmonary venous connection. Ann Thorac Surg 25: 479-487.
13. Goor DA,
Yellin A, Frand M, Smolinsky A, Neufeldt S (1976) The operative problem of small
left atrium in total anomalous pulmonary venous connection: Report of 5
patients. Ann Thorac Surg 22: 245-248.
14. Mathew
R, Thilenius OG, Replogle RL, Arcilla RA (1977) Cardiac function in total
anomalous pulmonary venous return before and after surgery. Circulation 55:
361-370.
15. Keith
JD, Rowe RD, Vlad P (1954) Complete anomalous pulmonary venous drainage. Am J
Med 16: 23.
16. Suga H
(1974) Importance of atrial compliance in cardiac performance. Circ Res 35:
39-43.
17. Hammon
JW Jr, Bender HW Jr, Graham TP Jr, Boucek RJ Jr, Smith CW, et al. (1980) Total
anomalous pulmonary venous connection in infancy: Ten years’ experience
including studies of postoperative ventricular function. J Thorac Cardiovasc
Surg 80: 544-551.
18. Graham
TP Jr, Jarmakani JM, Canent RV Jr. (1972) Left heart volume characteristics
with a right ventricular volume overload: Total anomalous pulmonary venous
connection and large atrial septal defect. Circulation 45: 389-396.
19. Taylor
RR, Covell JW, Sonnenblick EH, Rose J Jr. (1967) Dependence of ventricular
distensibility of filling of the opposite ventricle. Am J Physiol 213: 711-718.
20. Trusler
GA, Bull RC, Hoeksema T, Mustard WT (1963) The effect on cardiac output of a
reduction in atrial volume. J Thorac Cardiovasc Surg 46: 109-116.
21. Nakazawa
M, Jarmakani JM, Gyepes MT, Prochzka JV, Yabek SM, et al. (1977) Pre and
postoperative ventricular function in infants and children with right
ventricular volume overload. Circulation 55: 479-484.
22. Bove KE,
Geiser EA, Meyer RA (1975) The left ventricle in anomalous pulmonary venous
return. Morphometric analysis of 36 fatal cases in infancy. Arch Pathol 99:
522-528.
23. Nakazawa
M, Jarmakani JM, Gyepes MT, Prochazka JV, Yabek SM, et al. (1977) Pre and
postoperative ventricular function in infants and children with right ventricular
volume overload. Circulation 55: 479-484.
24. Latson
LA, Prieto LR (2007) Congenital and acquired pulmonary vein stenosis.
Circulation 115: 103-108.
25. Parr GV,
Kirklin JW, Pacifico AD, Blackstone EH, Lauridsen P (1974) Cardiac performance
in infants after repair of total anomalous pulmonary venous connection. Ann
Thorac Surg 17: 561-573.
26. Haworth
SG (1982) Total anomalous pulmonary venous return. Prenatal damage to pulmonary
vascular bed and extrapulmonary veins. Br Heart J 48: 513-524.
27. Newfeld
EA, Wilson PA, Paul MH, Reisch JS (1980) Pulmonary vascular disease in total
anomalous pulmonary venous drainage. Circulation 61: 103-109.
28. Yamaki
S, Tsunemoto M, Shimada M, Ishizawa R, Endo M, et al. (1992) Quantitative
analysis of pulmonary vascular disease in total anomalous pulmonary venous
connection in sixty infants. J Thorac Cardiovasc Surg 104: 728-735.
29. Perez M,
Kumar TK, Brieceno-Medina M, Alsheikh-Ali M, Sathanandam S, et al. (2016)
Common pulmonary vein atresia: Repair of three cases and review of literature.
Cardiol Young 26: 629-635.
30. Peterson
RC, Edwards WD (1983) Pulmonary vascular disease in 57 necropsy cases of total
anomalous pulmonary venous connection. Histopathology 7: 487-496.
31. Seale
AN, Webber SA, Uemura H (2009) Pulmonary vein stenosis: The UK, Ireland and
Sweden collaborative study. Heart 95: 1944-1949.
32. Jenkins
KJ, Sanders P, Orav EJ, Coleman EA, Mayer JE, et al. (1993) Individual
pulmonary vein size and survival in infants with totally anomalous pulmonary
venous connection. J Am Coll Cardiol 22: 201-206.
33. Ricci M,
Elliott M, Cohen GA, Catalan G, Stark J, et al. (2003) Management of pulmonary
venous obstruction after correction of TAPVC: Risk factors for adverse outcome.
Eur J Cardiothorac Surg 24: 28-36.
34. Chowdhury
UK, Subramaniam G, Joshi K, Varshney S, Kumar G, et al. (2007) Rechanneling of
total anomalous pulmonary venous connection with or without vertical vein
ligation: Results and guidelines for candidate selection. J Thorac Cardiovasc
Surg 133: 1286-1294.
35. Oh KH,
Choo KS, Lim SJ, Lee HD, Park JA, et al. (2009) Multidetector CT evaluation of
total anomalous pulmonary venous connections: Comparison with echocardiography.
Pediatr Radiol 39: 950-954.
36. Dyer KT,
Hlavacek AM, Meinel FG, De Cecco CN, McQuiston AD, et al. (2014) Imaging in
congenital pulmonary vein anomalies: The role of computed tomography. Pediatr
Radiol 44: 1158-1168.
37. Michielon
G, Di Donato RM, Pasquini L (2002) Totally anomalous pulmonary venous
connection: long-term appraisal with evolving technical solutions. Eur J
Cardiothorac Surg 22: 184-191.
38. Bando K,
Turrentine MW, Ensing GJ (1996) Surgical management of totally anomalous
pulmonary venous connection: Thirty year trends. Circulation 94: 12-16.
39. Hancock
Friesen CL, Zurakowski D, Thiagarajan RR, Forbess JM, del Nido PJ, et al. (2005)
Total anomalous pulmonary venous connection: An analysis of current management
strategies in a single institution. Ann Thorac Surg 79: 596-606.
40. Padalino
MA, Cavalli G, Franceschi MD, Mancuso D, Maschietto N, et al. (2014) Surgical
outcomes of total anomalous pulmonary venous connection repair: A 22 year
experience. J Card Surg 29: 678-685.
41. Shi G,
Zhu Z, Chen J, Ou Y, Hong H, et al. (2017) Total anomalous pulmonary venous
connection: The current management strategies in a pediatric cohort of 768
patients. Circulation 135: 48-58.
42. Sakamoto
T, Nagashima M, Umezu K, Houki R, Ikarashi J, et al. (2018) Long-term outcomes
of total correction for isolated total anomalous pulmonary venous connection:
Lessons from 50 years’ experience. Interact Cardiovasc Thorac Surg 27: 20-26.
43. Yashimura
N, Fukahara K, Yamashita A, Doki Y, Takeuchi K, et al. (2014) Current topics in
surgery for isolated total anomalous pulmonary venous connection. Surg Today
44: 2221-2226.
44. Wilson
WR, Ilbawi MN, DeLeon SY, Quinones JA, Arcilla RA, et al. (1992) Technical
modification for improved results in total anomalous pulmonary venous drainage.
J Thorac Cardiovasc Surg 103: 861-871.
45. Ando M,
Takahashi Y, Kikuchi T (2004) Total anomalous pulmonary venous connection with
dysmorphic pulmonary vein: A risk for postoperative pulmonary venous
obstruction. Interact Cardiovasc Thorac Surg 3: 557-561.
46. Craig
JM, Darling RC, Rothney WB (1957) Total puolmonary venous drainage into the
right side of the heart; report of 17 autopsied cases not associated with other
major cardiovascular anomalies. Lab Investig J Tech Methods Pathol 6: 44-64.
47. Delisle
G, Ando M, Calder AL, Zuberbuhler JR, Rochenmacher S, et al. (1976) Total
anomalous pulmonary venous connection: Report of 93 autopsied cases with
emphasis on diagnostic and surgical considerations. Am Heart J 91: 1199-1222.
48. Phillips
SJ, Kongtahworn C, Zeff RH, Skinner JR, Chandramouli B, et al. (1990) Correction
of total anomalous pulmonary venous connection below the diaphragm. Ann Thorac
Surg 49: 734-739.
49. Lupineti
FM, Kulik TJ, Beckman RH, Crowley DC, Bove EL (1993) Correction of total
anomalous pulmonary venous connection in infancy. J Thorac Cardiovasc Surg 106:
880-885.
50. Jian X,
Huang J, Ding Y, Xiao X, Wu M, et al. (2012) Surgical outcome of isolated total
anomalous pulmonary venous connection in adults: A 14 year experience. J
Cardiac Surg 27: 736-739.
51. Arikawa
K, Shimokawa S, Maruko M, Watanabe K, Watanabe S, et al. (1990) Surgery for
total anomalous pulmonary venous drainage in adults. Case reports and review of
eight Japanese patients over 40 years of age. J Cardiovasc Surg (Torino) 31:
231-234.
52. Berg GA,
Jamieson MPG, Pollock JCS (1986) Repair of total anomalous pulmonary venous
connection in adults. Thorac Cardiovasc Surg 34: 359-361.
53. Kikuchi
S, Yokozawa M (2005) Total anomalous pulmonary venous connection with a ductus
arteriosus aneurysm in a neonate: Report of a case. Surg Today 35: 1076-1077.
54. Kirklin
JW, Barratt-Boyes BG (1993) Total anomalous pulmonary venous connection. In:
Kirklin JW, Barratt-Boyes BG, editors. Cardiac surgery. 2nd Edn. New York:
Churchill Livingstone, pp: 645-673.
55. Yoshimura
N, Fukahara K, Yamashita A, Doi T, Takeuchi K, et al. (2017) Surgery for total
anomalous pulmonary venous connection: Primary suture less repair vs.
conventional repair. Gen Thorac Cardiovasc Surg 65: 245-251.
56. Azakie
A, Lavrsen MJ, Johnson NC, Sapru A (2011) Early outcomes of primary suture less
repair of the pulmonary veins. Ann Thorac Surg 92: 666-671.
57. Lacour-Gayet
F, Zoghbi J, Serraf AE (1999) Surgical management of progressive pulmonary
venous obstruction after repair of total anomalous pulmonary venous connection.
J Thorac Cardiovasc Surg 117: 679-687.
58. Caldarone
CA, Najim NK, Kadletz M, Smallhorn JF, Freedom RM, et al. (1998) Relentless
pulmonary vein stenosis after repair of total anomalous pulmonary venous
drainage. Ann Thorac Surg 66: 1514-1520.
59. Hawkins
JA, Minich LL, Tani LY, Ruttenberg HD, Strutevant JE, et al. (1995) Absorbable
polydioxanone suture and results in total anomalous pulmonary venous
connection. Ann Thorac Surg 60: 55-59.
60. Devaney
EJ, Ohye RG, Bove EL (2006) Pulmonary vein stenosis following repair of total
anomalous pulmonary venous connection. Semin Thorac Cardiovasc Surg Pediatr
Card Surg Ann 9: 51-55.
61. Yanagawa
B, Alghamdi AA, Dragulescu A, Viola N, Al-Radi OO, et al. (2011) Primary suture
less repair for “simple” total anomalous pulmonary venous connection: Midterm
results in a single institution. J Thorac Cardiovasc Surg 141: 1346-1354.
62. Chowdhury
UK, Mishra A, Saxena A, Kothari SS, Malhotra A, et al. (2007) A novel
percutaneously adjustable device for ligature of the vertical vein in the
setting of obstructive totally anomalous pulmonary venous connection. Cardiol
Young 17: 380-386.
63. Gaines
WE, Pierce WS, Prophet GA (1984) Pulmonary circulatory support: A quantitative
comparison of four methods. J Thorac Cardiovasc Surg 88: 958-964.
64. Ishino
K, Alexi-Meskishvili V, Hetzer R (1997) Myocardial recovery through ECMO after
repair of total anomalous pulmonary venous connection: The importance of left
heart uploading. Eur J Cardiothorac Surg 11: 585-587.
65. Twedell
JS (2007) The vertical vein: To ligate or not to ligate. Rechanneling of total
anomalous pulmonary venous connection with or without vertical vein ligation:
Results and guidelines for candidate selection. J Thorac Cardiovasc Surg 133:
1135-1136.
66. Lutembacher
R (1916) De la sténosemitrale avec communication interauriculaire. Arch Mal
Coeur 9: 237-260.
67. Bland
EF, Sweet RH (1949) A venous shunt for marked mitral stenosis. JAMA 140: 1259.
68. Bland EF
(1987) Rheumatic fever: The way it was. Circulation 76: 1190-1195.
69. Cooley
DA, Collins HA (1959) Anomalous drainage of entire pulmonary venous system into
left innominate vein: Clinical and surgical considerations. Circulation 19:
486.
70. Cooley
DA, Ochsner A Jr. (1957) Correction of total anomalous pulmonary venous
drainage. Surgery 42: 1014.
71. Corno A,
Giamberti A, Carotti A, Giannico S, Marino B, et al. (1990) Total anomalous
pulmonary venous connection: Surgical repair with double patch technique. Ann
Thorac Surg 49: 492-494.
72. Mendeloff
EN, Spray TL, Huddleston CB, Bridges ND, Canter CB, et al. (1995) Lung
transplantation for congenital pulmonary vein stenosis. Ann Thorac Surg 60:
903-907.
73. St.
Louis J, McCracken CE, Turk EM, Hancock HS, Menk JS, et al. (2018) Long-term
transplant-free survival after repair of total anomalous pulmonary venous
connection. Ann Thorac Surg 105: 186-192.
74. Massie
AB, Kucirka LM, Segev DL (2014) Big data in organ transplant: Registries and
administrative claims. Am J Transplant 14: 1723-1730.
75. Kabayashi
D, Forbes TJ, Dellus RE, Aggarwal S (2012) Amplatzer vascular plug for
transcatheter closure of persistent unligated vertical vein after repair of
infracardiac total anomalous pulmonary venous connection. Catheter Cardiovasc
Interv 80: 192-198.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Spine Diseases
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)