1666
Views & Citations666
Likes & Shares
According to the World Bank, (2024) Nigeria’s poverty is projected to hit 52% by 2026, while poverty in Nigeria stood at 38.9% in 2023 (World Bank, 2025). In Nigeria, a lot of people still rest their hope for treatment in the divine, they patronize religious houses expecting miracle healing, these are mostly poor people who have lost hope in the constituted authority’s ability to provide succor. Majority in the rural and urban areas still take herbs for treatment of tropical ailment like malaria, yellow fever and typhoid. In place of the figures released yearly for public health spending, health infrastructure falls short, while the ever-increasing population stretched the available health infrastructure. There is evidence of increased health spending but corresponding effect on poverty remain uncertain. The advent of the forth republic in Nigeria in 1999 sees increase in public health expenditure, however, the poverty level keeps fluctuating, Figure 1, presents a better picture. Public health expenditure for year 2000 stood at 15.22 billion Naira (Central Bank of Nigeria [CBN], 2022), poverty rate was at 64.9% (Nigerian National Bureau of Statistics [NBS], 2022), for year 2005 public health expenditure increased to 34.20 billion Naira (CBN, 2022), poverty rate reduced to 55.9% (NBS, 2022). Furthermore, for 2010 public health expenditure stood at 99.10 billion Naira (CBN, 2022), while poverty rate increased to 56.4% (NBS, 2022), for 2015 public health expenditure increased to 257.70 billion Naira (CBN, 2022), poverty rate remained at 56.4% (NBS, 2022), for 2020 public health expenditure was at 423.36 billion Naira (CBN, 2022), while poverty rate reduced to 40.1% (NBS, 2022). This demonstrated that although, public health expenditure increased consistently, but poverty rate did not reduce in reflection to the increase experienced in public health expenditure within the period in focus.

Making sure that citizens live healthy lives is important for sustainable development, as the recent experience during the novel COVID-19 pandemic has indicated the reality that health predicament has what it takes to disrupt economies and destabilize people lives (Oladosu, 2022). Improving access to healthcare services at the community level informed Nigeria’s government decision to embrace the primary healthcare system in 1986 and today almost all wards in the country has a primary healthcare center (Anaemene, 2016). However, access to healthcare services especially for rural dwellers in Nigeria presents a situation where they have to travel for hours to access health care facilities, while for urban dwellers it’s the cost implication, thereby questioning the functionality of the primary healthcare system. In both cases, access is affected for the rural dwellers both location and finance, while for the urban dwellers finance only in some cases. The disparity in income is evident in Nigeria, this negates one of the goals of public health expenditure, and this affect access to healthcare services for people both in rural and urban areas. According to Oladosu, (2022) enhance health spending is key for all country’s growth objective, to fall in line with the sustainable development goals (SDG 3) put forward by the United Nations (United Nations Sustainable Development Goals, 2020). While Agbeni, (2025) submits that public spending is expected to reduce poverty and enhance growth, and likewise public spending on health has a corresponding effect to improve productivity of labour leading to increase in national output.
Various studies in relation to the theme of this paper dwell on various methodology arriving at various outcomes. Agbeni, (2025) used ARDL technique to conduct their study on disaggregated technique on; poverty rate, public spending and Nigeria’s economic performance between 1991 to 2023, they found that public spending positively affect poverty. Kalu, (2025) explored ARDL to appraise the connection between health spending and results considering income level in sub-Saharan nations and that public spending on health does not affect poverty positively as a result of poor management of allocated resources especially financially based resources. On the other hand, this study is on assessing the nexus between public health expenditure and poverty in Nigeria, utilizing data between 2000 and 2022, while extant literature presents studies on public health expenditure using various method such as ARDL, GMM, multilevel linear mixed effect technique. Outcome varies, resting on technique, geography and time period. This study uses NARDL which superiority rest on its ability that decomposes the effect of the independent variables on the dependent variable into their negative and positive components. Specifically, on Nigeria this methodology seems scarce, therefore in filling this gap this study might happen on a more robust outcome that might impact policy direction and help in mitigating the effect of poverty for enhance economic performance in Nigeria.
LITERATURE REVIEW
Theoretical Literature
Vicious Cycle of Poverty Theory
Ragner Nurkse, (1953) put forward the vicious cycle of poverty theory, with the thrust that; people are poor because they are poor, and the situation of poor families where the head of household (HOH) is unable to make available the basic needs of the household such as; health, food, clothing, shelter, education and many others (Bass, 2011). The poverty will perpetuate for generations to come, if the earlier HOH was unable to provide all the basic requirements. Unless either of the two factors interrupts; supply side solution, here Nurkse advocated increase in savings to improve on investment, where short-run and long-run investment should be well coordinated. And demand side solution, here Nurkse advocated widening of the market so that people can have access to incentive to invest and through balance growth, so that demand in one sector can be fulfilled by another sector. Nurkse, (1953) detailed his theory through a source of income in developing countries that is yet to fully developed will cause the whole household suffered the same poverty problem. This points that, the vicious circle of poverty in developing countries leads to low level of savings and investment. Low investment especially in education will lead to low productivity which again leads to low income. Figure 2 depicts a better picture, starting with, low income will lead to low purchasing power among the poor as a result of corresponding low productivity which may arise as a result of their low level of skills or education, and in developing countries this may not be unconnected with the low level of human capital development. The order will incidentally diminish their ability to save and invest; investment which is supposed to create new jobs in the economy, this might lead to increase in the rate of unemployment. While on the supply side, low income will also lead to low saving power capacity which as a result makes their income barely enough for their daily needs (Bass, 2011). In Nigeria the poverty rate might be influenced by the low level of productivity as a result of low level of investment and investment is low because savings is low, savings is low because of the low level of income, and income is low because productivity is low. This circle goes on as a result; while the poor remain poor, unemployed, sometimes because of their low level of skill.

Health Intervention Based Theory
Tannahill, (1980) put forward a health promotion theory christened, Intervention Based Theory (IBT), the theory is made up of three intersecting domains for actions; health education, disease prevention and health protection. Health educations main goal is changing the information, attitudes, beliefs and behavior such that it makes outcome better. While the goal of disease prevention is to minimize risk factors and curtail the magnitude of disease; it is made up of primary, secondary and tertiary prevention. Health protection on the other hand rest on fiscal of legal regulations and policies and deliberate codes of practice targeted at averting illness and promoting health. Furthermore, according to Obisike, (2021) and Tannahill, (2009) protecting the public include policies and spending focused at the public, that promotes open access to health system, employment, access to drugs and education. Critics posits that, fiscal and legal concepts are wide-ranging and hence, dwell on the theory’s inability to give exhaustive clarification of fiscal or legal regulation and policies. They also furthered that, theory fall short in its inability to model a state for better analytical analysis mathematically and statistically. However, for the reason of this study, we dwell on the theories ability to capture key components that interest public expenditure on health which are; health education, disease prevention and health protection.
Theoretical Framework
This study is anchored on the Ragner Nurkse, (1953) vicious cycle of poverty theory which postulated that, people are poor because they are poor; in other words, the situation of poor families where the head of household (HOH) is unable to make available the basic needs of the household such as; health, food, clothing, shelter, education and many others. Alternatively, poverty will perpetuate for generations to come, if the earlier HOH was unable to provide all the basic requirements. Unless either of the two factors interrupts; supply side solution, here Nurkse advocated increase in savings to improve on investment, where short-run and long-run investment should be well coordinated. And demand side solution, here Nurkse advocated widening of the market so that people can have access to incentive to invest and through balance growth, so that demand in one sector can be fulfilled by another sector. In this case, public health expenditure serves as the demand side solution, where public health spending fills in the income gap.
Empirical Literature
Lagos communities’ knowledge on tragic spending on health and ancillary reasons was examine by Wright, (2025). The study explored cross sectional survey method to collect data from 2492 homes within four local councils in Lagos metropolis, with the aid of a questionnaire. The data was analyzed with STATA, using univariate, bivariate and binary logistic regression. Outcome indicated that, 15% of families encounter tragic healthcare spending. Furthermore, healthcare insurance registration was positively linked to tragic health spending. While, gender, faith, family location, income level, self-rated health status are positive determinants of tragic health spending. The study concluded that, tragic health spending is common with families with lower socioeconomic status, urban dwellers and not enroll in health insurance programme. Therefore, suggested that, enlightenment about health insurance scheme should be ongoing and scheme be widened to cover households from poor socioeconomic background. However, public health spending was put side by side with all-encompassing growth in Nigeria, focusing on the place of institutions by Ngozi & Olusegun, (2025). Data was sourced between 1990 to 2023 using ARDL for estimation. Outcome from the study indicated that, public health spending has positive effect on all encompassing growth futuristically. While for the short and long run interface between public health spending and institutional excellence lies significant effect. The study submits that institutional excellence deter effort of attaining all-encompassing growth in Nigeria. And therefore, suggests that, rejigging Nigeria’s institutions.
Appraisal of the connection between health spending and results considering income level in sub-Saharan nations was carried out by Kalu, (2025). Data was drawn from 45 SSA nations, while ARDL technique was used for estimation and outcome suggests that, inadequate healthcare delivery is an indication of poor management of allocated fuds not lack of funds across the SSA nations. The study advocated for strong institutions, enhanced budgetary allocation and backing for low income nations, will mitigate the poor healthcare delivery across the SSA nations. For Agbeni, (2025) conducted a study on disaggregated technique on; poverty rate, public spending and Nigeria’s economic performance between 1991 to 2023. The study explored the ARDL estimation technique for analysis and findings indicated that, performance of the economy decreases poverty in the long and short run, public spending having significant impact on poverty. The study submits that, public expenditure in education, health and agriculture in Nigeria is either inadequate or poorly distributed, in that its effect on poverty is negligible. The study suggested that, public spending on key areas like; health, agriculture infrastructure and education should be enhanced to improve on growth.
Anderson behavioral model-based interrogation of factors associated with health poverty susceptibility in rural China, after the poverty relief era was interrogated by Wang, (2024). The study used binary logistic regression and outcome showed that, rural households are at danger of falling back into poverty as a result of their health challenges. The study concludes that, to prevent rural families from once more becoming poor, poverty reduction should be focus on prevention and policy should be futuristic driven. On the other hand, Arinze, (2024) posed the question if the authorities’ efficiency is key on investment in public health and maintainable health results within 45 sub-Saharan nations in Africa. Data was taken for these countries from 1960 to 2022 and using ARDL for estimation. Outcome indicated that, poor health result not limited to poor funding only, but also from administrative efficiency. The study submits that strong institutions and safety nets be put in place to regulate inefficiency and abuse of privileges to mitigate incidence harmful to public health investment. Furthermore, the authorities should rejig its primary health system to take care of health challenges at the grass roots in SSA nations.
Nigeria’s case was considered by Adekunle, (2024) on public spending and interdependence of poverty between 1981-2019. The study explored Engel Granger causality test and ARDL for estimation and outcome indicated that, in the short run public spending upset per capita consumption and weak effect in the future. The study concludes that; it has shade light on the Nigerian poverty dynamics. Therefore, the study suggests that public spending be directed at infrastructural development. While, the economic effect of public health spending was interrogated by Singh, (2024) the study used quantitative technique for analysis and findings indicated that, per capita income affects health, stability political wise and non-terrorist activities bring about high impact on health spending. Furthermore, bogus allocation to the health sector don’t mean positive health results. The study recommends improved public health to enhanced health outcomes in India.
Under five deaths was examine in sub-Saharan African nations based on health spending and institutional excellence by Sibanda, (2024) between 2000 to 2021. Data was sourced from 46 sub-Sahara African countries, using GMM model for estimation. Result indicated that, public health spending and external support help to mitigate the incidence of under-five mortality. Furthermore, out of pocket health spending also help in reducing under five deaths. The spread of HIV and maternal mortality negatively affect child health. The study submits that, enlightenment, immunization for children and ICT innovation can help mitigate the incidence of under-five mortality, while positive economic performance influence child health. Therefore, the study suggests that, sub-Saharan African nation evolve strong institutions as it helps improve the effectiveness of health expenditure. Examination of the extent of health spending on purposed changeable poverty in India: reasoning Ayusha Bharat experience by Thakur, (2024). Using stratified sampling procedure to collect data and analyze using multivariable logistic regression. Outcome indicated that out of pocket health expenditure drives people to poverty, furthermore, outpatient concerns have significant effect on removable poverty. The effect is more telling on rural households across the country. The study therefore, suggest the need for universal healthcare coverage and a total health insurance framework in India.
Causative outcome of terrible spending on health on poverty was examine by Kolasa & Weychert, (2024). Data was drawn from families spending survey in Poland between 2010 to 2013 and 2016 to 2018, while recursive bivariate probit model were used for analysis. Outcome of the study indicated that, significant causal link exists between terrible health expenditure and relational poverty in Poland. The study submits that; policy makers should be more concern about the reality of out of pocket health spending that the statistics are stating. The study suggested that, support should be given to those hit by terrible health spending. Furthermore, across the West African economic and monetary union, civic health spending impact on maternal mortality ratio was interrogated by Boundioa & Thiombiano, (2024). Panel data for 7 West African nations were sourced from the World Bank between 1986 to 2018. Two steps least squares on health demand was exploited for estimation. Outcome of the study showed that, civic outlay on health care indicated a non-positive but significant association with maternal mortality, while out of pocket spending indicated non-negative association. The study submitted that, civic health outlay is key in mitigating the negative impact of maternal mortality across West Africa. Hence, the study suggested that, if the region needs to positive improve maternal mortality incidence, its civic outlay on health must be enhance.
The reasons for inequality in public health spending across the African regional commercial communities between 2000 to 2019 was examined by Ngepah & Mouteyica, (2024). The study explored multilevel linear mixed effect technique for estimation. Outcome indicated that, gross domestic product per capita (GDPPC) indicated non-influential, poverty level and growth heighten, public health spending inequality. Although, information communication technology (ICT) penetration shrink the inequality in public health spending. Therefore, they advocated for more investment and trade in ICT to help mitigate the disparities in civic health spending across the African regional economic communities. Biltagy & Hamdi, (2024) studied Egypt’s family cycle poverty and government’s spending on Healthcare between 2005 to 2015. The study employed the quantitative technique for estimation with data from the world bank and Egypt economic forum. Outcome of the study indicated that, public health spending in Egypt make available healthcare services for years among urban and rural dwellers, and to all homes across all families’ wealth divide in the country.
Tragic healthcare in Nigeria was examine by Edeh, (2022) using the logistic regression model. Outcome showed that more families are faced with tragic healthcare spending depending on economic status of the families and geopolitical zones. The study submits that to reduce the income distribution gap, furthermore, widening the health insurance gap are strategies to mitigate the tragic health spending being experience by many families in Nigeria. For Orji, (2021) asked if wealthy nation is healthy all the time, based on Nigeria link between health outcomes and spending, between 1985-2019. The study explored regression analysis and indicated that, health spending by the authorities and immunization to fight measles decreases under five mortality level meaningfully thereby improves life expectancy, while HIV spread reduces life expectancy. Banking on the outcome the study suggested that, health spending be targeted at areas that makes more impact. When resources are adequately used a resourceful country like Nigeria can improve the health outcome for its citizens.
Nigeria’s poverty level and effect of public capital spending was examined by Jideofor, (2021) using ARDL estimation technique. Outcome of the study showed that, capital spending has important effect on poverty level in Nigeria. Therefore, the study suggested that more capital spending be directed at; education, energy, health and economic services, the study also canvassed judicious utilization of resources. While Wagner’s hypothesis was tested in Nigeria by Olayiwola, (2021) in light of Nigeria’s economic performance and its public health spending between 2000 to 2016. The study explored the ARDL and Engel Granger causality test for estimation. Outcome from the study presented a futuristic link between public spending in health and economic performance in Nigeria, while no causal link was found between the variables. The study advocated for expansion of the health insurance scheme to capture people especially the non-forma sector to boost resources for the health sector.
For Omoniyi, (2018) it was the consideration for the reasons for poverty on Nigeria’s economic performance. The study exhaust data between 198o to 2013 while exploring the error correction model for estimation. Outcome indicated existence of influential link between persistent rise in the prices of goods and services, life expectancy and economic performance in Nigeria. Conclusion submitted that, debt, poverty, corruption, mortality rate, unemployment and human capital development negatively affects economic performance. On the other hand, banking on Health account framework Lawanson & Olaniyan, (2013) did a relative study on Northern Nigeria’s health spending and status to that of Southern Nigeria. The study covered the period 2003 to 2005. Outcome indicated that, healthcare spending in both region (North and South) Nigeria is moderately lower, with poor health status and reliance on families. Therefore, suggested that public spending on health should be enhanced base on the low income of majority, especially in the north, that will improve the health status of the people.
METHODOLOGY
Nature and Sources of Data
The study utilizes time series data Poverty Rate (POR), from Nigerian National Bureau of Statistics (NBS), Public Health Expenditure (PHE), Education Expenditure (EDE) and Access to healthcare (AHC) from Central Bank of Nigeria Statistical Bulletin, Gross Domestic Product Per Capita (GDPPC) from World Development Indicator and Employment rate (ER) from Penn World Table.
Model Specification
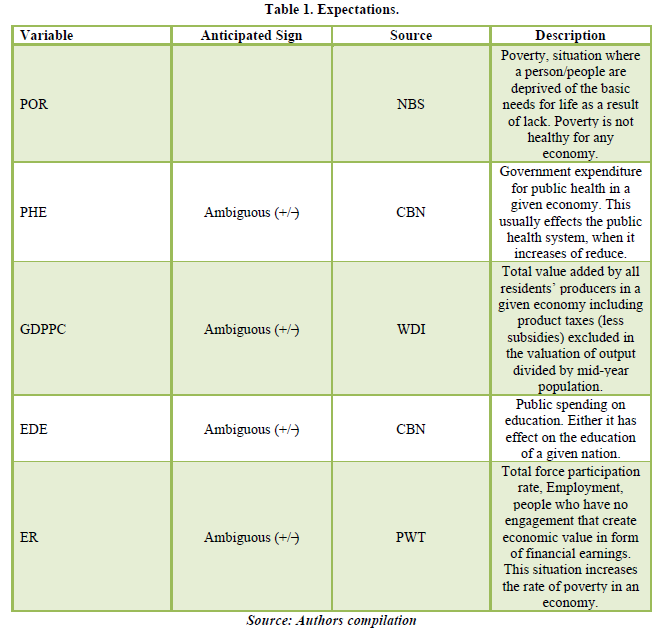
The study utilized the Non-Linear Auto Regressive Distributed lag (NARDL) to interrogate the nonlinear link between public health expenditure and poverty in Nigeria. This model allows for the possible examination of the asymmetric effect of the positive and negative fluctuations inherent in the independent variables on the dependent variables (Shin, Yu & Greenwood-Nimo, 2014) (Table 1).

Where: POR: Poverty Rate; PHE: Public Health Expenditure; GDPPC: Gross Domestic Product Per Capita; EDU: Education Expenditure; ER: Employment Rate; AHC: Access to Healthcare; α0 to α5 indicates unknown vector parameters; Ɛt depicts stochastic term; Δ represents first difference operator; p is the lag order of the dependent variable; q1, q2, q3, q4 are lag orders of the independent variables; θ+ and θ- capture the long-run effects of positive and negative changes in PHE.
PRESENTATION AND DISCUSSION OF RESULT
Outcome of the ADF unit root test indicated a mix order of stationarity, with poverty rate, public health expenditure, educational expenditure stationary at first difference and gross domestic product per capital and employment rate stationary at level (Table 2).

The result of the NARDL bounds test result showed that the F. Table 3 statistics value is higher than the lower and upper bound at 5%. This implies accepting the alternate hypothesis of existence of a long run link between the variable of interest, public health expenditure and poverty in Nigeria. This call for the estimation of the short and long run NARDL model.
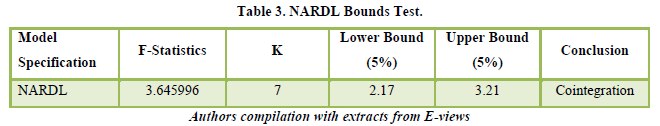
Table 4 showed outcome of the Wald test result implying significance and existence of an asymmetric link between public health expenditure and poverty in Nigeria.
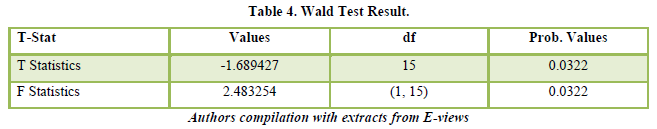
Table 5 depicts outcome of the long and short run of the NARDL, which showed that the independent variable, public health expenditure, gross domestic product per capita, educational expenditure, employment rate explained about 70% of the cumulative adjustments in poverty rate, while the remaining 30% is taken by the stochastic term. The probability value showed that the model used for the study is robust.
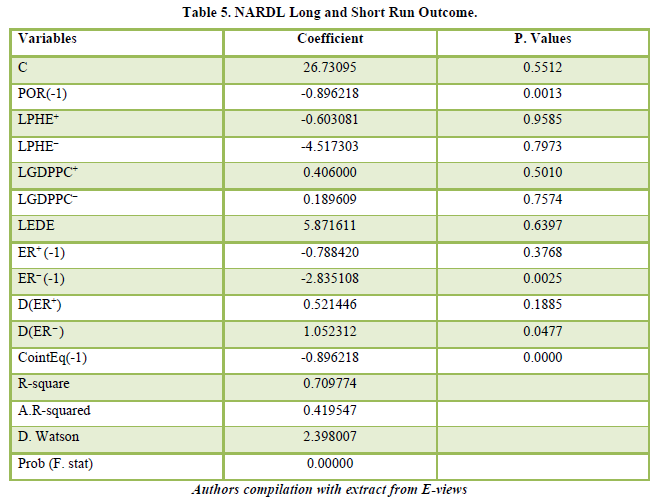
The long run on Table 5 indicated that the positive and negative components of the coefficient of public health expenditure are not significant at 5%. Though both of the coefficient is negative, this implies that in the future effect resulting from shocks as a result of the positive and negative components of public health expenditure are the same. The estimated coefficient of positive public health expenditure is -0.603081, indicating that in the future a percentage surge in public health expenditure will result in contraction in poverty by 0.6% with a probability value not significant at 5%. The coefficient of the negative public health expenditure is -4.517303, implying that, in the future a percent surge in public health expenditure will result in contraction in poverty by 4.5%, with a probability value not significant at 5%. This might imply that, in the future poverty will not be affected by public health expenditure in spite to the surge. With increase in allocation which is expected to impact on job creation especially in the health sector and its multiplier effects on households’, its effect on poverty might be negligible. Perhaps Nigeria increase in population in the absence of adequate planning and implementation might be responsible.
The inflationary pressure might stifle the effect of increased allocation to the health sector, although it might create jobs, increased income but the increase might mean more funds will be allocated to meeting basic needs as prices keeps rising. This is indicated by the period covered between 2000 to 2022 for this study, as public health expenditure increases consistently in Nigeria over the period its effect on poverty remains negligible. On the other hand, (Agbeni, 2025) found contrasting view that public health expenditure has significant impact on poverty in Nigeria, though their study was between 1991 and 2023.
Gross domestic product per capita has a positive coefficient on both the positive and the negative components, and both are not significant at 5%. On the positive component, gross domestic product per capita has a coefficient of 0.40600 implying that in the future a percent decrease in gross domestic product per capita will lead to a contraction in poverty in Nigeria that will amount to 0.4%, with an insignificant probability value at 5%. The coefficient of the negative component of gross domestic product per capita is 0.189609 implying that in the future surge in gross domestic product per capita will lead to a contraction in poverty in Nigeria of about 0.2% with an insignificant probability value at 5%. This implies decrease in gross domestic product per capita will negative affect the poverty level, because people fall into poverty when their productivity is affected in the negative light. Although, increase in public health expenditure creates an enabling environment for people to better their health and be more productive, healthy people will mean more work hours and this will positively affect their output. While on the other hand, unhealthy people will spend more time being unproductive attending to their health. The outcome of this finding agrees with Ngozi & Olusegun, (2025) where they found that, public health spending has positive effect on all encompassing growth (implying more output) in the long run.
Educational expenditure has a positive coefficient and non-asymmetric in the future, indicating that the effect of educational expenditure on poverty in the future is not asymmetrical and also not significant at 5%. The coefficient of educational expenditure is 5.871611 which means that in the future a percentage surge in educational expenditure will bring about shrinkage in poverty of about 5.8% and with a probability value not significant at 5%. This is an indication that with increase in educational expenditure access to education will be widen and more people will be opportune to improve their educational status thereby standing a better chance for better employment opportunity and earning better income in the future. Education, especially at the tertiary level improves better chances for economic mobility for the poor, and this is a welcome development for the fight against poverty especially for a developing economy like Nigeria.
Employment rate indicated a negative outcome for both coefficients and presented only the first lag situation. Incidentally, the positive component is not significant while the negative component presents an opposite situation both at 5%. In the first lag, the coefficient of the positive component of employment rate is -0.788420 an indication that in the future surge in employment rate will bring about contraction in poverty by 0.7% in Nigeria, with a probability value that is not significant at 5%. The coefficient of the negative component of employment rate is -2.835108 an indication that in the future surge in employment rate will bring about contraction in poverty rate in Nigeria of about 2.8% with a significant probability value at 5%. Rise in employment rate will improve poverty rate on a positive note, while fall in employment rate will affect poverty rate negatively. When disposable income of people increase they spend more and this will enable producers expand their business and engage more hands, this is in conformity with the Keynesian prescription.
However, in the interim asymmetry between public health expenditure and poverty rate in Nigerian does not exist, but exist between poverty and employment rate, while the probability value of the positive component is insignificant that of the negative component is significant all at 5%. The coefficient of positive component of employment rate is 0.521446 implying all things being equal in the interim a unit surge in employment rate will lead to a contraction of about 0.5% in poverty rate in Nigeria, with an insignificant probability value at 5%. For the negative component of employment rate, the coefficient is 1.052312 meaning that all things being equal in the interim a unit change in employment rate will initiate an expansion in poverty rate in Nigerian by about 1.1%, with a significant probability value at 5%.
CONCLUSION AND RECOMMENDATION
We examine the negative and positive components between public health expenditure and poverty in Nigeria using data between 2000 to 2022. The study explored the superiority of NARDL model technique, this permit disaggregation of the effect of the independent variables on the dependent variable, for the analysis of the future and interim asymmetric effect between the concerned variables, this is the contribution of this study. Considering these under linear technique might be misleading especially for Nigeria. Findings showed that asymmetry exist between public health expenditure and poverty in Nigeria in the future but not in the interim. However, asymmetry between poverty and employment rate exist in the interim. The study found that public health expenditure has no meaningful effect on poverty in Nigeria in the future. Based on this outcome the following recommendations were arrived at;
Increase in public health expenditure should be accompanied with expansion in the access to health insurance packages this will contribute in redistribution of income in the society and might contribute in deepening the effect of the increase on poverty rate in Nigeria. Increase in public health expenditure should also go along with increase in education expenditure, because when more people are educated their sense of personal hygiene and also improves and their chances for economic mobility also increases. Employment generation contribute to the rise in the output of individuals and on the aggregate. Therefore, relevant authorities should dedicate more funds on infrastructure in the health sector to widen chances for jobs for both the skilled and unskilled in the health sector.
- Agbeni, K., Akanni, O., Francisca, A. Y., Gbadebo, A. J., Chioma, P. E. et al. (2025). Government Expenditures Economic Growth and Poverty Levels in Nigeria: A Disaggregated Approach. International Journal of Economics and Management Review, 3, 18-33.
- Adekunle, S. A. O. (2024). Public expenditure and poverty interdependence: Evidence from Nigeria. Pakistan Journal of Life and Social Sciences, 22.
- Anaemene C.E. (2016). Local government and challenges of primary healthcare delivery services in Imo state. International Journal of Academic Management Science Research, 2, 19-33
- Arize, A., Kalu, E. U., Lubiani, G., & Udemezue, N. N. (2024). Public health expenditure and sustainable health outcomes in 45 Sub-Saharan African countries: Does government effectiveness matter? Economies, 12, 129.
- Biltagy, M., & Hamdi, M. (2024). Public health expenditure and household poverty: Case study of Egypt. Future Business Journal, 10, 1-12.
- Bo, S. (2020). Centralization and regional development Evidence from a political hierarchy reform to create cities in China. Journal of Urban Economics, 115, 103-182.
- Boundioa, J., & Thiombiano, N. (2024). Effect of public health expenditure on maternal mortality ratio in the West African Economic and Monetary Union. BMC Women's Health, 24(1), 109.
- Edeh, H. C. (2022). Exploring dynamics in catastrophic health care expenditure in Nigeria. Health Economics Review, 12, 22.
- Jideofor, N. J., Michah, C. O., & Ikhite, H. O. (2021). Impact of public capital expenditure on poverty rate in Nigeria. International Journal Papier Public Review, 2, 46-55.
- Kalu, E. U., Arize, C. A., Okwueze, F. O., & Udemezue, N. (2025). Evaluating the nexus between health expenditure and health outcomes with consideration for income characteristics in SSA countries. Future Business Journal, 11, 1-22.
- Kolasa, A., & Weychert, E. (2024). The causal effect of catastrophic health expenditure on poverty in Poland. The European Journal of Health Economics, 25, 193-206.
- Krishna, A. (2010). One illness away why people become poor and how they escape poverty. NewYork Oxford University Press.
- Lawanson, A. O., & Olaniyan, O. (2013). Health expenditure and health status in Northern and Southern Nigeria A comparative analysis using national health account framework. African Journal of Health Economics 2, 31-42.
- Liu, M., Feng, X., Wang, S., & Qiu, H. (2020). China’s poverty alleviation over the last 40 years: Successes and challenges. Australia Journal Agricultural Resource Economics, 64, 209-228.
- Ngepah, N., & Mouteyica, A. E. N. (2024). Factors influencing inequality in government health expenditures within African regional economic communities. BMC Health Services Research, 24, 1-12.
- Ngozi, A. E., & Olusegun, A. J. (2025). Government health expenditure and inclusive growth in Nigeria. The role of institutions. Journal of Economics and Allied Research, 225, 225-244.
- Obisike, N. E., Iwuchukwu, U. R., Unegbu, P. I., & Achumie, E. N. (2021). Impact of public health spending on health outcomes in Nigeria. International Journal of Economics and Financial Management, 6, 1-18.
- Oladosu, A. O., Chanimbe, A., & Anaduaka, U. S. (2022). Effect of public health expenditure on health outcomes in Nigeria and Ghana. Health Policy Open, 3.
- Omoniyi, B. B. (2018). An examination of the causes of poverty on economic growth in Nigeria. Africa’s Public Service Delivery and Performance Review 6, 1-10.
- Orji, A., Ogbuabor, J. E., Mba, P. N., & Anthony-Orji, O. I. (2021). Are wealthy countries always healthy health outcomes and public health spending nexus in Nigeria. SAGE Open 1-14.
- Saheed O. Olayiwola, O. S., Bakare-Aremu, T. A., & Abiodun, S. O. (2021). Public health expenditure and economic growth in Nigeria Testing of Wagner's hypothesis. African Journal of Economic Review, 9, 130-150.
- Sibanda, K., Qoko, A., & Gonese, D. (2024). Health expenditure institutional quality and under-five mortality in sub-Saharan African countries. International Journal of Environmental Research and Public Health, 21, 333.
- Tannahill, A. (2009). Health promotion The Tannahill model revisited. Public Health, 123, 396-399.
- Perez-Fargallo, A., Marin-Restrepo, L., Centreras-Espinoza, S., Bienvenido-Huertas, D. (2023). Do we need complex and multidimensional indicators to assess energy poverty? The case of the Chilean indicator. Energy and Buildings, 295, 1-14.
- Rowntree, B. S. (1901). Poverty a study of town life. New York Policy Press.
- Singh, N. (April, 2024). Analysis of public healthcare expenditure and its economic impact. International Journal of Research in Social Sciences and Humanities; 14, 38-52.
- Thakur, R., & Faizan, M. A. (2024). Magnitude of health expenditure induced removable poverty in India: Some reflections of Ayushman Bharat. Heliyon, 10.
- United Nations (2020). Sustainable Development Goals.
- Wang, W., Chen, K., Xiao, W., Du, J., & Qiao, H. (2024). Determinants of health poverty vulnerability in rural areas of Western China in the post-poverty relief era an analysis based on the Anderson behavioral model. BMC Public Health, 24, 1-16.
- Wright, K.O., Adeniran, A., Aderibigbe, A., Akinyemi, O., Fagbemi, T. (2025). Factors associated with catastrophic healthcare expenditure in communities of Lagos Nigeria A megacity experience. PLoS ONE 20: 0316814.
- Xiang, Q., Yan, C., Ma, Y., Liao, H., & Wang, J. (2021). Classification and influencing factors of rural elderly’s vulnerability to health-related poverty in central and western regions of China. Global Health Journal, 5: 135-43.
- Zhu, J., Liu, S., Li, Y. (2021). Removing the hats of poverty effects of ending the national poverty county program on fiscal expenditures. China Economic Review, 69: 20-38.




