Case Report
Two Staged Surgical Correction of Kyphoscoliosis with Intraspinal Anomalies
4415
Views & Citations3415
Likes & Shares
Introduction: The kyphoscolitic deformity may be associated with various intraspinal anomalies which usually occur early in life. These can be managed safely in two staged with gap of 3-6 month between two procedures.
Objective: To retrospective study of 20 patients who underwent two staged surgical treatment for progressive spinal deformity and co-existing intraspinal anomalies.
Method: The study of 20 patients with kyphoscoliosis associated with intraspinal abnormalities which were operated by neurosurgery department for intraspinal anomaly and then the 2nd stage surgery for deformity correction by spine unit headed by chief author during Jan-2016 to Feb-20 in our institution.
Result: The mean age was 11.4 years, with 13 females and 7 males. Most common anomaly was Diastematomyelia with 10 patients, 4 tethered spinal cord, 3 of syringomyelia 3 with ACM. The mean duration between two surgeries was 6 months. The mean operation time was 7.3 hours (range, 6–9 hours) and the mean blood loss was 1460 mL (700-2360 ml). The mean hospitalization stay was 9 days (7-18 days). None of the patients experienced deterioration in their neurologic status after surgery. None of the patients had infection, pseudoarthrosis, or loss of correction during the follow-up visits.
Conclusion: Two staged surgical treatment has lesser complications and seems to be a safer treatment option with respect to reduced operative time and less blood loss as compared to single stage procedure and proves to be a safe management principle to such challenging problem.
Keywords: Intraspinal anomalies, congenital scoliosis, Diastematomyelia, Tethered cord syndrome, PVCR
INTRODUCTION
Intra spinal anomalies associated with kyphoscoliosis could be various conditions like tethered cord, Diastematomyelia, lipoma, syringomyelia teratoma. The incidence of congenital scoliosis is 1/1000 live births and that of intraspinal anomalies associated with spinal deformity varies from 20-47% as reported in different studies around the globe [1-3]. Congenital spinal deformity occurs during the first 8 weeks of gestation during which the bony element of the spine forms and the neural axis completes its folding and these congenital developmental spine anomalies can be seen in ultrasonography. All congenital vertebral anomalies have an increased risk (approximately 15%) of intraspinal anomalies. Neonatal spinal ultrasound performed before extensive laminar ossification has occurred (6-12 week) will show major intraspinal anomalies and tethering [4]. Any adverse effect around this period can lead to congenital spinal deformities such as scoliosis, kyphosis along with intraspinal anomalies. Intraspinal anomalies can lead to rapid curve progression, neurological deficit, and cardio-respiratory arrest.
Patients at presentation if all symptomatic for their corresponding intraspinal anomaly present with complaints of spasticity, progressive neurological deficit, or bowel bladder involvement, indicating further investigations like MRI, Ct scan, myelogram etc. However, patients presenting for asymptomatic cosmetic reasons for their scoliosis in non-adolescent age group further investigations must be done as MRI as shown by Rajasekaran [1,3].
Diastematomyelia is known as a congenital disorder in which a part of the spinal cord is split by bony/cartilaginous spur. Split is in a sagittal direction usually at the upper lumbar vertebra. Congenital bony or fibro cartilage septum present in the spinal cord and by means of removal of this bony spur surgically this problem can be treated.
Tethered spinal cord syndrome is a disorder caused by tissue attachments that limits spinal cord movement within the spinal column because of adhesion of cord. Closely associated with spina bifida. Syringomyelia is a disorder in which a cystic cavity forms within the spinal cord. The cyst (syrinx) can expand and elongate over time destroying the spinal cord. Surgery is the treatment of choice. Arnold Chiari malformation is a disorder of hindbrain in which there is herniation of posterior fossa contents through foramen magnum. Scoliosis is seen in 50%-90% of patients with ACM. Sub occipital decompression done to release anatomical and physiological CSF blockage.
OBJECTIVE
To retrospective analysis of 20 consecutive patients who underwent two staged surgical treatment for progressive spinal deformity and coexisting intraspinal pathologies.
METHOD
This is a retrospective study of 20 patients with kyphoscoliosis associated with intraspinal abnormalities which were operated during Jan-2016 to Feb-20 in our institution. In the first stage all patients were operated by neurosurgery department for intraspinal anomaly then after 3-6 month the second stage surgery for kyphoscoliotic deformity correction by spine unit headed by chief author for deformity correction.
Those patients were selected for study who presented with spinal deformity associated with intra- spinal anomalies and age less than 13-year age with normal or near normal neurology are included in study. Those patients who had major neurological deficits with or without bowel bladder involvement, syndromic or neuromuscular and patients who developed deficits post neurosurgical procedure, those are not give consent for risk of surgical procedure were excluded from the study group.
All the patients were looked for age at presentation, sex, and measurement of associated kyphosis and scoliosis with cob’s method and neurological status. All the patient had standing AP, lateral, right and left bending films, suspension views of the spine from C7 to sacrum were taken to measure various angle (cob’s angle) to determine magnitude and extent of deformity. 3D CT scan of the affected part taken to confirm any type of bony defect, vertebral anatomy and pedicle geometry was evaluated. All patients were subjected to neural axis MRI from brainstem to sacrum to detect the associated intraspinal anomalies. For screening of genitourinary anomalies ultrasonography, ECG and echocardiography for cardiac anomalies were done. Other investigation done in view to evaluate pulmonary function test, pulse oximetry, blood gas analysis, hematocrit. Multi-disciplinary team comprising neurosurgeon, pediatrician, intensivist, anesthesiologist, pediatric cardiologist is summoned to evaluate and optimize the patient adequately.
Neurosurgical procedure was done in all of these patients and for Diastematomyelia septum or bony spur is excised, in tethered cord detethering or release was done, and foramen magnum decompression is achieved in Arnold Chiari malformation in above all patients. In post-operative period patients were under intensive monitoring and health, nutrition, and blood parameters monitored and optimized for a period of 3-6 months till clearance from pediatric department for the deformity surgery was given.
SURGICAL STEPS
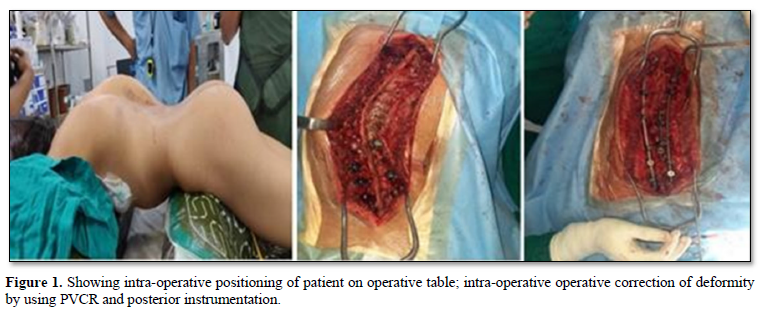
Deformity correction procedure also performed under neuromonitoring with the same midline incision with careful soft tissue dissection around the previous surgery as the bony landmarks around the laminectomy defect were difficult to identify, so first proximal and distal subperiosteal dissection was performed and as per the preoperative planning with UIV stable vertebrae and LIV neutral vertebrae which was significantly touched vertebrae on CSVL was selected, segmental instrumentation with polyaxial pedicle screws with anchors at all levels and approximate implant density more than 70% used, as dysplastic pedicle were present in majority of cases. Deformity correction with hemi vertebrectomy done by PVCR technique at the apex of the curve along with multiple pontes osteotomies, concave rib releases done in case of severe deformity. Cobalt chrome rods used to align screw head by using derotation, segmental compression distraction, translation, and cantilever technique. Posterior fusion with decortications and bone grafting was done in all cases. Post-operative all patients were kept in intensive care and mobilized in Boston brace after 48 h with drain removal when output less than 50 cc in the last 8 h.
Figure 1 shows intra-operative positioning of patient on operative table; intra-operative operative correction of deformity by using PVCR and posterior instrumentation.
RESULTS
We have operated 20 patients having kyphoscoliosis along with intraspinal deformity over a period of 4 yrs. The mean age of the patients at presentation ranged from 3 to 19 years (Mean 11.4 years).
There were 13 female patients and 7 male patients. Out of these cases of congenital scoliosis, there were 6 classified as failure of formation, 5 as failure of segmentation, and 3 as mixed defects. Out of 20 patients 10 patients had Diastematomyelia with tethered cord, 4 with syringomyelia, 3 had tethered cord only and 3 had Arnold chairi malformations.
No patients had neurologic deficits at the time of presentation, and all had associated spinal deformity. Genitourinary anomalies were seen in 3 patients (unilateral agenesis of the kidney in 2 patients and ectopic kidney in 1 patients). None of them had clinical features suggestive of genitourinary anomalies but were incidental findings detected on screening. Cardiovascular anomalies were seen in 6 patients with mitral valve prolapse.
The mean duration between two surgeries was 6 months (range 4-8 months). The mean operation time was 7.3 h (6-9 h), the mean blood loss was 1460 mL (700-2360 mL) and average surgical time of deformity correction was 276 min (186-330 min). All patients spent at least 3 days in intensive care unit and the mean hospitalization time was 9 days (7-18 days).
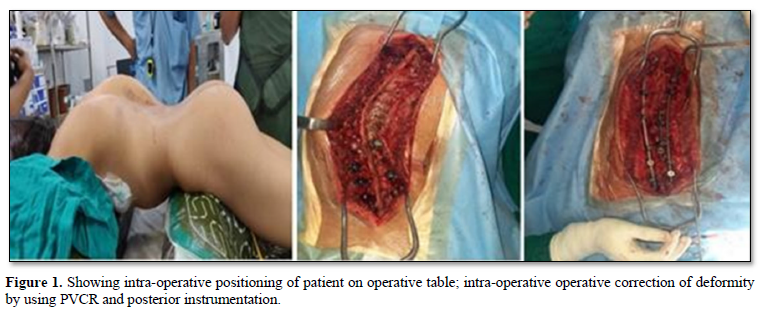
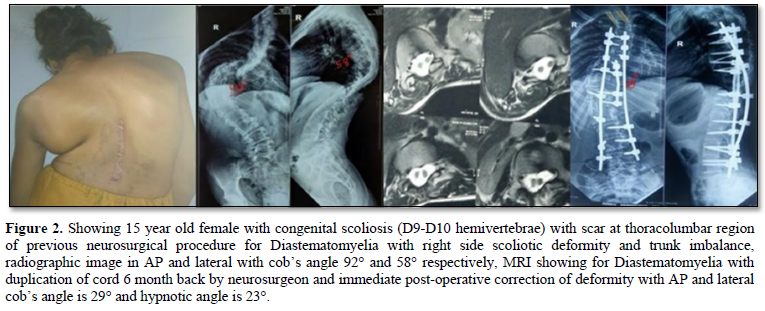
The mean correction angle of deformity was 56.53±25.22 pre-operatively which is corrected to 21.13±14.34 post operatively and 23.93±14.99 at final follow up and the correction loss at the end of follow-up was less than 10%. None of the patients experienced deterioration in their neurologic status after surgery. None of the patients had infection, pseudoarthrosis, or loss of correction during the follow-up visits (Figures 2 & 3).
DISCUSSION
The kyphoscoliosis is related with congenital anomalies in other systems, especially those formed from mesenchymal tissue. These anomalies are often asymptomatic and absent or asymmetric abdominal reflex may remain isolated finding in examination and may remain undetected until the patient is fully assessed following the diagnosis of congenital spinal deformity [4,5].
Theoretically, intraspinal abnormality can predispose the patients to neurological injury when they undergo surgical correction of scoliosis due to excessive traction of spinal cord. However, performing surgery for the intraspinal in asymptomatic patients also carries some risk of morbidity including neurological deterioration and wound problems. However, the neurosurgical procedure performed by laminectomy over 4-5 levels and flavectomy over these levels provide some form of posterior releases around the apex so. In our series of 20 patients, balancing of the S- shaped curves was achieved, and none of the patients experienced deterioration in their neurologic status after surgery.
Rapid surgical correction of severe scoliosis associated with forceful intra-operative maneuvers can increase the risk of neurologic compromise especially in patients with a history of intraspinal anomaly and we do not advocate, since the goals of the surgery are balancing of the curve, preventing progression of deformity or development of neurodeficit. Dysplastic pedicles must be anticipated in the pre-operative planning and get actual axial cut across the pedicles in CT scan and if found dysplastic, sub laminar wires, hooks and cables must be in the backup.
According to Hamzauglu [2] simultaneous surgical treatment for congenital deformity and intraspinal abnormality does not involve significant complications and seems to be an attractive and safe treatment option. It does not increase the surgical time, blood loss, and hospitalization time too much.
According to Winter [6] the classic advocated approach in patients having congenital spine deformity associated with intraspinal abnormality is first to perform surgery for the intraspinal pathologies and then surgery for correction and stabilization of the deformity 3 to 6 months later in a different session. Our study also in favor of two staged correction surgery this allow decrease morbidity of patient post operatively and allow them to recover.
Average age at which a patient presented and female preponderance of congenital scoliosis and intraspinal anomalies and thoracolumbar curve was the most common deformity in our study all was similar to all the previous reports or McMaster series [7,8].
Genitourinary anomalies that can cause obstruction are silent and, if not searched for, may cause serious damage before they are diagnosed. The incidence of genitourinary anomalies was found to be 23.8% in the current study. This is similar to frequencies seen in other studies also [8,9].
Cardiovascular anomalies were the most common of the associated systemic anomalies in our study. They were seen in 28.5% of patients with mitral valve prolapse being the commonest anomaly. According to Winter, the incidence of congenital heart disease in congenital scoliosis was 7% [9,10]. The cause of our high rate may be the small size of the patient group.
Patients with rigid spinal deformity often combine with severe pulmonary function impairment, and many research have shown that anterior spinal surgery had great impact on pulmonary function. PVCR has first been introduced by Suk et al and has been popularized by Lenke [11,12] for severe deformities of the spinal column, it enables translational and rotational correction of spinal column and offers the advantage of a controlled manipulation of both the anterior column and the posterior column at the same time through a single approach. PVCR could not only correct the deformities as good as or better than other surgery, but also could avoid anterior approach related complications, particularly to pulmonary function impairment.
One major concern with PVCR technique is the potential neurologic complications, which may occur from direct neurologic injury during bone resection or deformity correction. The former may be mitigated through techniques such as careful retraction of nerve roots during resection of pedicles and careful planning of osteotome trajectory and force when removing the vertebral body. Neurologic complications may also result from subluxation of the spinal column, dural buckling and compression of the spinal cord by residual bone and soft tissues in the canal after correction [13].
Intraspinal anomalies were associated with 47% of patients with congenital scoliosis in the Indian population. 71% of congenital scoliosis patients with intraspinal anomalies were females. Hemivertebrae was the most common vertebral anomaly in scoliosis, and it was most located in the thoracic spine. Intraspinal anomaly was most common in vertebrae with segmentation and mixed defects. Tethered cord was the most common intraspinal anomaly in the Indian population. Special attention should be given to physical examination and inspecting for any neurocutaneous markers; however, absence of neurocutaneous markers does not rule out intraspinal anomaly. MRI should be the part of routine protocol for assessment of congenital scoliosis patients [1-3,8,12].
In the current study, the incidence of intraspinal anomalies was 35%, which was within the range reported to vary from 18.3% to 47%. Tethered cord syndrome due to tight filum terminal was the most common type of spinal anomaly noted in this study which was similar to observations reported in other studies. The mean age of onset of deformity was 11.4 years in those who had intraspinal anomalies as compared to the AIS group which was 13.2 years indicating that early age of onset is an indicator for presence of such anomalies? There is a significant correlation between age of onset of deformity and intraspinal anomaly in the idiopathic group of patients (P≤0.05). In the current study, all the patients with intraspinal anomalies associated with congenital scoliosis needed neurosurgical intervention before surgical correction of the deformity.
CONCLUSION
The Two staged surgical treatment for congenital deformity with intraspinal abnormality does not involve significant complications and seems to be an alternative and safe treatment option with respect to reduced operative time and less blood loss as compared to single stage procedure and proves to be a safe management principle to such challenging problem.
- Rajasekaran S, Gupta N, Balamurali G, Shetty A (2016) Vertebral and Intraspinal Anomalies in Indian Population with Congenital Scoliosis. Asian Spine J 10(2): 276-281.
- Hamzaoglu A, Ozturk C, Tezer M, Aydogan M (2007) Simultaneous Surgical Treatment in Congenital Scoliosis and/or Kyphosis Associated with Intraspinal Abnormalities. Spine 32(25): 2880-2884.
- Rajasekaran S, Kamath V, Kiran R, Shetty AP (2010) Intraspinal anomalies in scoliosis: An MRI analysis of 177 consecutive scoliosis patients. Indian J Orthop 44(1): 57-63.
- Upasani V, Pamela KD, Estroff J, Benjamin WC, Emans JB, et al. (2016) Prenatal diagnosis and assessment of congenital spinal anomalies. World J Orthop 18: 7(7): 406-417.
- Prahinski JR, Polly DW, McHale K, Ellenbogen RG (2000) Occult intraspinal anomalies in congenital scoliosis. J Pediatr Orthop 20: 59-63.
- Winter RB, Haven JJ, Moe JH, Lagaard SM (1974) Diastematomyelia and congenital spine deformities. J Bone Joint Surg Am 56: 27-39.
- McMaster MJ (1984) Occult intraspinal anomalies and congenital scoliosis. J Bone Joint Surg Am 66: 588-601.
- Gillespie R, Faithfull DK, Roth A, Hall JE (1973) Intraspinal anomalies in congenital scoliosis. Clin Orthop Relat Res 93: 103-109.
- Winter RB (1973) Congenital scoliosis. Clin Orthop Relat Res 93: 75-94.
- Roth A, Rosenthal A, Hall JE, Mizel M (1973) Scoliosis and congenital heart disease. Clin Orthop Relat Res 93: 95-102.
- Suk SII, Kim J-H, Kim W-J, Lee S-M, Chung E-R, et (200) Posterior vertebral column resection for severe spinal deformities. Spine 27: 2374-2382.
- Lenke LG, Sides BA, Koester L (2007) Posterior Vertebral Column Resection (VCR) for Sever Pediatric and Adult Spinal Deformity: Indications, Results and Complications of 43 Consecutive Cases. Scoliosis Research Society 42nd Annual Meeting Course, Edinburgh.
- Suk SII, Chung E-R, Kim J-H, Kim S-S, Lee J-S, et al. (2005) Posterior vertebral column resection for severe rigid scoliosis. Spine 30: 1682-1687.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Alcoholism Clinical Research
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)





