5097
Views & Citations4097
Likes & Shares
Clinical Characteristics
Most patients presented with pain and weakness of their lower limbs. 32.6% of patients had sensory symptoms of the limbs such as para-anesthesia and anesthesia. 30% had bowel and bladder involvement prior to surgery. The majority of patients (60%) had no fever or malaise (Figure 2).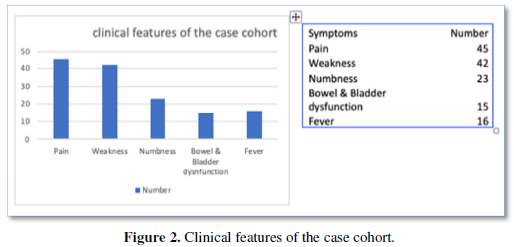
On Examination, clinical signs were different ranging from swelling and deformity of the spine (gibbus) (52%), tenderness (almost all patients), paraspinal abscess and collection (39.13%), lower limb weakness (present in all but 6 patients), and sensory deficits (almost 50% of patients) as shown in Figure 3.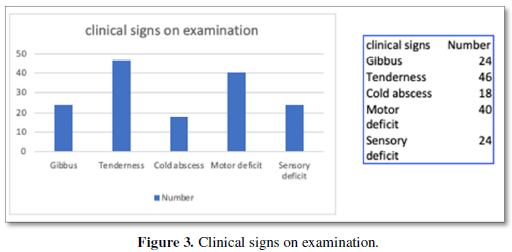
Cold abscesses were seen in almost 40% of cases. Most of the abscesses were seen on the thoracic and lumbar regions extending into the iliopsoas sheath (Figure 4).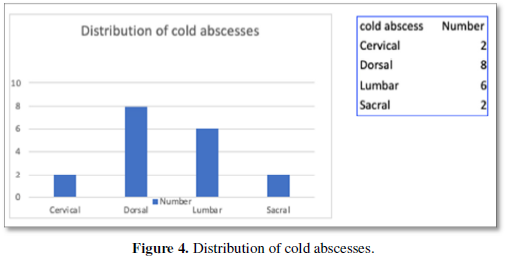
The presence of Motor deficit was the most important factor in deciding on whether surgery was to be performed or not as it emphasized the prognosis and function status of the patient viz-a-viz surgery. 6 patients didn’t have any deficit. However, 4 patients had severe quadriparesis and 6 were complete paraplegics (Figure 5).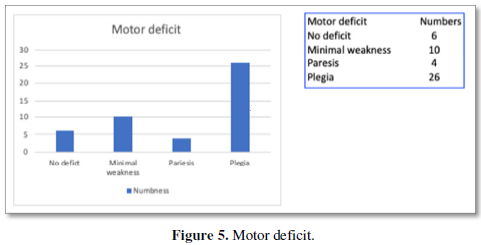
Radiological Characteristics
The definitive diagnosis and planning for surgery was made with radiological investigations. Of the 46 patients with TB, 12 showed wedging and collapse of vertebral bodies on Xray and 14 showed features suggestive of cold abscess. The final diagnosis was reserved for CT and MRI of the spine. Cord compression was noted in 42 patients while paraspinal collection was seen in 18 patients. Ct was done to demonstrate the bony destruction associated with long standing TB. The distribution of the disease was also characteristic with the majority in the thoracic and lumbar regions, as shown in Figure 6.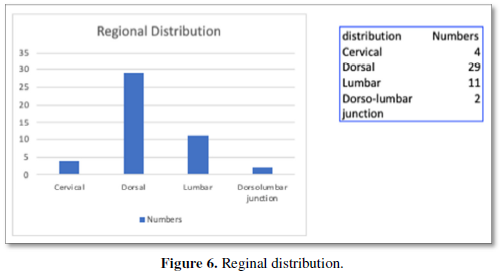
Most vertebral involvement was characteristically involving 2 levels, emanating from the adjacent disc space. Few only had 1 level involvement while 4 cases had more than 2 level involvement (Figure 7).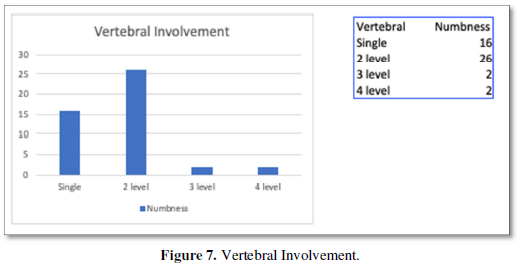
SURGERY
All 46 patients underwent spinal stabilization with decompression of the spinal canal. Implants with bone grafts were used as well to augment the stabilization and fusion. Specific surgical situations are described as follows.
1 patient had an Odontoid fracture with a cold abscess around the C1 C2 joint. The patient underwent an occipito-cervical fusion using contour rods and bone grafting coupled with craniovertebral junction decompression and drainage of cold abscess. However due to significant anterior compression persisting, he underwent a transpolar odontoidectomy with anterior decompression.
3 patients underwent anterior cervical discectomy with debridement of the granulation tissue in the paraspinal region coupled with iliac crest bone grafts ensuring stability with decompression.
4 patients developed serous wound discharge post-surgery which was managed conservatively. The wounds healed with regular dressing and appropriate antibiotic therapy. No re-explorations were performed.
6 patients had stabile spines just requiring decompression. No fusion was performed in them.
13 patients were fused posteriorly alone with canal decompression and abscess drainage in the lumbar region.
14 patients underwent thoracic decompression by costo-transversectomy. Stabilization was done with pedicle screw augmented by rib grafts.
15 patients underwent thoracotomies with anterolateral fusion with mono-axial screws and rods to the vertebral bodies coupled with debridement of the phlegm on and decompression of the cord.
Post-Operative Complications
No neurological worsening was noted after surgery. No implant breakage or malalignment was seen.
Hospital Stay
Ranged from 1 week (in patients without stabilization) to 4 weeks (in patients requiring thoracotomy and chest tubes).
Time to Ambulation
Patients were ambulated in the first week itself on a Zimmer frame with either a thoraco-lumbar brace or a lumbar corset. Early mobilization aided in reduction of pain and early return to functionality. Patients with paraplegia were ambulated on wheelchairs after 4 weeks.
Antituberculosis Therapy
Anti TB therapy of 5 drugs was given for 18 months regularly. 6 patients were given extended therapy for 24 months, due to extensive disease on recommendation of experts.
Outcome
Outcome has been measured in 2 ways: as per neurological improvement of the patient coupled with the reduction in inflammatory markers signifying reduction of disease intensity.
All patients improved after 6 months of continuous physiotherapy. On follow up 4 out of 6 paraplegics had complete neurological recovery and were ambulant with minimal support. The ASIA grading of outcome is shown in Figure 7 while, ESR reduction was gradually noted in most patients. The gradual reduction is shown in Figure 8.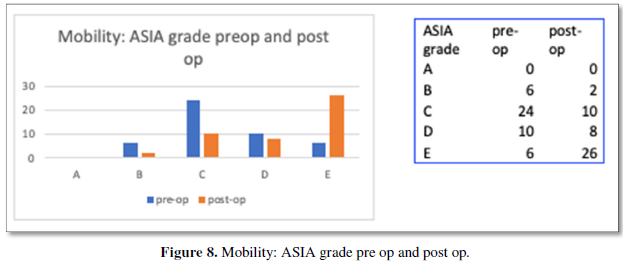
DISCUSSION
Tuberculosis of spine has had a storied history in India with extensive documentation in both surgical and bacteriological perspectives [16,17]. Hence, we present our data in comparison with the latest established dictums of spinal surgery and bacteriology to elucidate the authenticity of our work as well as offer explanations regarding deviations from the established norm.
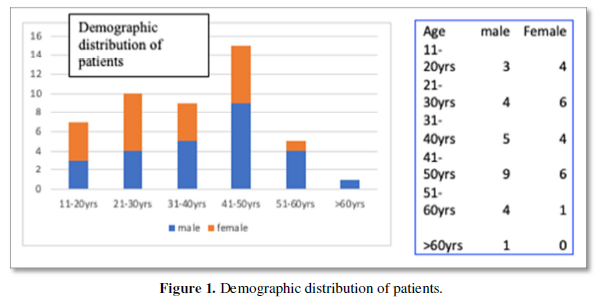
Our study showed a 61% of males involved with the maximum age group being between 41-50-year age group (33%) In a similar study by Park et al in Korea in 2007, maximum mean age of 41.5 years comparable with our values [18-20]. Most studies had the majority of patients presenting to the clinic with pain. Few had weakness of limbs which varied significantly between socioeconomic groups and nationalities. We however had a massive 91% of neurological weakness. The reason for our high levels of motor weakness is possibly that our patients come from low socioeconomic backgrounds and hence present late with severe symptoms [21-23]. For the same reason or study also had a very high incidence of bowel and bladder dysfunction (32.6%).
The dorsal and lumbar segments were involved in the majority of patients as is with other international case series, probably due to the watershed phenomena in vascular supply affecting these segments of the spine predominantly [23,24]. Most patients in our study had 2 vertebrae involved on either side of the affected disc space (56.5%) which is also in line with international data. The involvement of so mites in hematogenous spread of the disease allows for a disc space and its adjacent vertebrae to be fed together, thereby affecting the same segments pathologically as well [25]. 39% of our patients had visible swellings on their backs which is greater than comparable published data. However due to our patients coming late for surgery, the data isn’t remarkable in itself. Kyphosis was also seen in 52.17% due to the same reason.
Outcomes were good despite the serious presentation of patients. Udwadia [25] demonstrates a recovery rate of 92% with 74% improving from non-ambulatory to ambulatory status [23-27]. As shown in Figure 7, ASIA grades of the patients when compared from pre-op to post op showed excellent improvements. As mentioned earlier, 4 of the 6 paraplegic patients were ambulatory post rehabilitation.
Surgical procedures employed were standard, with emphasis on cord decompression with stabilization to ensure early mobilization and optimal recovery. Deformity correction when applicable was also done as mentioned above. Transpedicular instrumentation systems have distinct advantages such as rigid segmental fixation, stabilization of the three columns of the spine, least failure at bone metal interface, early post-operative mobilization with efficient nursing care and least complications in the management of tuberculosis of the thoraco-lumbar spine [26,27].
All patients had 18 months of antituberculosis therapy as per category 3 revised national TB control programme (RNTCP) guidelines in India. All patients were also registered with the National Tuberculosis Registry and monitored for drug compliance to ensure optimal bacteriological clearance. Some patients were given extended regimens based on individual requirements and expert opinion.
CONCLUSION
Although the prevalent impression of TB spine presents a picture of despondency and negativity, judicious use of appropriate surgery and aggressive physiotherapy, presents a viable option towards good recovery and return to functionality. Emphasis on early detection, prompt decompression, stabilization along with antituberculosis therapy must be made to ensure optimum results to all affected.
- Ferrer MF, Torres LG, Ramírez OA, Zarzuelo MR, González NDP (2012) Tuberculosis of the spine. A systematic review of case series. Int Orthop 36: 221-231.
- Khoo LT, Mikawa K, Fessler RG (2003) A surgical revisitation of Pott distemper of the spine. Spine J 3(2): 130-145.
- Kiran NAS, Vaishya S, Kale SS, Sharma BS, Mahapatra AK (2007) Surgical results in patients with tuberculosis of the spine and severe lower-extremity motor deficits: A retrospective study of 48 patients. J Neurosurg Spine 6: 320-326.
- Tuli SM (2007) Tuberculosis of the spine: A historical review. Clin Orthop Relat Res 460: 29-38.
- Varatharajah S, Charles Y-P, Buy X, Walter A, Steib J-P (2014) Update on the surgical management of Pott's disease. Orthop Traumatol Surg Res 100(2): 229-335.
- Moon M-S (2006) Development in the management of tuberculosis of the spine. Curr Orthop 20: 132-140.
- Rasouli MR, Mirkoohi M, Vaccaro AR, Yarandi KK, Rahimi-Movaghar V (2012) Spinal Tuberculosis: Diagnosis and Management. Asian Spine J 6(4): 294-308.
- Mak KC, Cheung KMC (2013) Surgical treatment of acute TB spondylitis: indications and outcomes. Eur Spine J 22(Suppl4): 603-611.
- Patil SS, Mohite S, Varma R, Bhojraj SY, Nene AM (2014) Non-surgical management of cord compression in tuberculosis: A series of surprises. Asian SpineJ 8: 315-321.
- Nene A, Bhojraj S (2005) Results of nonsurgical treatment of thoracic spinal tuberculosis in Spine J 5: 79-84.
- Wouda EMN, Stienstra Y, Werf TSV, Kerstjens H, de Lange WCM, et al. (2017) Neurological and functional recovery in tuberculosis patients with spinal cord injury in the Netherlands. Neuro Rehab 40: 439-445.
- Jain AK (2010) Tuberculosis of the spine: A fresh look at an old disease. J Bone Joint Surg Br 92: 905-913.
- Rajasekaran S (2001) The natural history of post-tubercular kyphosis in children. Bone Joint J 83-B: 954-962.
- Rajasekaran S (2007) Buckling collapse of the spine in childhood spinal tuberculosis. Clin Orthop Relat Res 460: 86-92.
- Wimmer C, Ogon M, Sterzinger W, Landauer F, Stöckl B (1997) Conservative treatment of tuberculous spondylitis: A long-term follow-up study. J Spinal Disord 10: 417-419.
- Upadhyay SS, Saji MJ, Sell P, Sell B, Hsu LC (1994) Spinal deformity after childhood surgery for tuberculosis of the spine. A comparison of radical surgery and debri-dement. J Bone Joint Surg Br1 76: 91-908.
- Upadhyay SS, Saji MJ, Sell P, Hsu LC, Yau AC (1996) The effect of age on the change in deformity after anterior debridement surgery for tuberculosis of the spine. Spine 21: 2356-2362.
- Rajasekaran S (2012) Kyphotic deformity in spinal tuberculosis and its management. Int Orthop 36: 359-365.
- Mukherjee JS, Rich ML, Socci AR, Joseph JK, Virú FA, et al. (2004) Programmes and principles in treatment of multi drug-resistant tuberculosis. Lancet 363: 474-481.
- Mase S, Chorba T, Parks S, Belanger A, Dworkin F, et al. (2020) Bedaquiline for the treatment of multidrug-resistant tuberculosis in the united states. Clin Infect Dis 71(4): 1010-1016.
- Ferlazzo G, Mohr E, Laxmeshwar C, Hewison C, Hughes J, et al. (2018) Early safety and efficacy of the combination of bedaquiline and delamanid for the treatment of patients with drug-resistant tuberculosis in Armenia, India, and South Africa: A retrospective cohort study. Lancet Infect Dis 18: 536-544.
- Guglielmetti L, Dû DL, Jachym M, Henry B, Martin D, Caumes E, et al. (2015) Compassionate use of bedaquiline for the treatment of multidrug-resistant and extensively drug resistant tuberculosis: Interim analysis of a French cohort. Clin Infect Dis 60: 188-194.
- Giridharan P, Selladurai E, Balaji S, Pramila SK, Arunagirinathan V, et al. (2020) Drug resistant TB spine in a two-year-old child: a case report. Indian J Tuberc 67(3): 374-377.
- Shah SS, Goregaonkar AA, Goregaonkar AB (2017) Extensively drug-resistant tuberculosis of the lumbar spine in a six-year-old child: A case report. J Orthop Case Rep 7: 40-43.
- Udwadia ZF, Amale RA, Mullerpattan JB (2014) Initial experience of bedaquiline use in a series of drug-resistant tuberculosis patients from India. Int J Tuberc Lung Dis 18(11): 1315-1318.
- Li Y, Huang H, Dong W, Lan T, Fan J, et al. (2019) Penetration of linezolid into bone tissue 24 h after administration in patients with multidrug-resistant spinal tuberculosis. PLoS One 14(10): e0223391.
- Rao SPS, Alonso S, Rand L, Dick T, Pethe K (2008) The proton motive force is required for maintaining ATP homeostasis and viability of hypoxic, non-replicating myco-bacterium tuberculosis. Proc Natl Acad Sci 105(33): 11945-11950.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Oncology Clinics and Research (ISSN: 2643-055X)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns










