Research Article
Minimally Invasive Surgical Treatment (U Device) in Lumbar Canal Stenosis in Elderly Patients
5074
Views & Citations4074
Likes & Shares
Introduction: Degenerative lumbar stenosis in elderly patients is a serious health problem, surgical treatment seems to be the best results but presents the question of whether all patients with this disease should be treated with the same technique. The purpose was to show the results of the surgical treatment of degenerative lumbar stenosis in patients over 75 years treated at the IMED General Hospital Valencia (Spain).
Methods: We performed a retrospective study in patients older than 75 years diagnosed with degenerative lumbar canal stenosis. The variables studied were age, sex, symptoms, location, major comorbid conditions, and radiographic classification by MRI. Surgical technique was used (Interspainous U device), we used the Oswestry index and Visual Analogue Scale of pain as evaluation instruments.
Results: The series was composed of 10 patients, there was a predominance of female with 67.6%, 1 year follow-up. The predominant symptom was lumbar pain and claudication.
Conclusions: The Oswestry index and visual analog scale pain showed significant improvement in postoperative and obtained 95. % of Excellent results.
Keywords: Degenerative lumbar stenosis, MIS technique, U Device
INTRODUCTION
Canal stenosis is the most common degenerative pathology after 60 years of age. It consists of the progressive closure of the vertebral canal that compresses the lumbar and sacral roots.
The history of stenosis seems to begin in 1803 when Antoine Portal described the narrowing of the spinal canal in his study of cadavers; Gower in 1891 suggested that the narrowing of the foramina could cause damage to the nerve roots and painful symptoms [1].
It is Wiltse in 1893 who performed the first decompressive laminectomy which is followed by Sachs and Fraenkel in 1900 who published that root clamping was the cause of sciatic pain in the elderly [1].
The twentieth century, as part of its great scientific advances, revolutionized the understanding of stenosis, the works of Casamajor and Dejerine in 1911 are followed by those of Donald and Volger in 1925 with the description of the characteristics of the vertebral canal in achondroplasia [1].
Putti [1] in Italy in 1927 described the role of superior articular facet hypertrophy in nerve root entrapment and consequent sciatica.
Elsberg and Dyke began measurements of the spinal canal in 1934, until in 1954 Verbiest was the first to give a detailed description of the lumbar spinal canal stenosis syndrome [2].
This was followed in 1976 by Arnoldi with the classification of nerve root entrapment syndrome, the important works by Kirkaldy-Willis [3] on pathology and pathogenesis of stenosis and later Senegas [4] in 1988 with the classification by pathological anatomy and his decompressive recalibration technique.
There are two classic theories to explain the pathogenesis of pain:
- The theory of neurological compression where the mass effect of hypertrophied structures on the nervous tissue causes less circulation of cerebrospinal fluid and consequently less supply of nutrients with changes in microcirculation and edema, accumulation of residues, change to an acid pH, cell death and fibrosis.
- The theory of vascular compression where the compromise of arterial and venous flow causes venous congestion, increased pressure in the capillaries and little oxygen supply to the nerve roots.
The truth is that the degeneration of the intervertebral disc is the main cause that triggers the succession of phenomena that lead to the stenosis of the spinal canal [5] and this degeneration is basically a process mediated by cells of the nucleus pulposus which as early as in the first decade of life change its composition.
The three-joint concept states that intervertebral movements are generated on a large tripod, where the intervertebral disc is the anterior joint and the joint facets complete the two posterior supports of the three-joint complex. Any alteration in one of these joints, which generally occurs primarily in the disc, generates biomechanical stresses on the others; which results in arthritic or degenerative changes in the articular facets with the consequent further deterioration of the disc itself. This sequence is repetitive and severe damage to the intervertebral movement complex is established [6,7].
The clinical picture generally begins with pain referred to the lower back, which evolve into a crisis type that is becoming increasingly frequent and difficult to treat, then the pain radiating to one or both lower limbs commonly known as sciatica appears. Finally, there are manifestations referring to a greater neurological intake, such as claudication and sphincter disorders, which significantly limits the physical capacity of these patients.
The risks that concur in these older adult patients with their biological and psychosocial characteristics progressively increase and the impact of new favorable conditions on their life expectancy decreases. Therefore, surgical interventions in older patients should be selected because they are clearly effective, with a low relative risk, and their success is related to maximizing longevity [8].
The symptoms are mainly neurogenic claudication, which consists in that when the patient walks a certain number of meters he has to stop or sit due to pain, paresthesia or loss of strength (it is popularly known as the showcase syndrome).
The MRI usually shows a narrowing or stenosis of the lumbar canal. In principle, a conservative treatment with analgesics, anti-inflammatories and physiotherapy can be tried, but if the clinical picture does not subside, surgical treatment is ideal.
There are various techniques, some very aggressive such as laminectomy and lumbar fixation or arthrodesis with transpedicular screws.
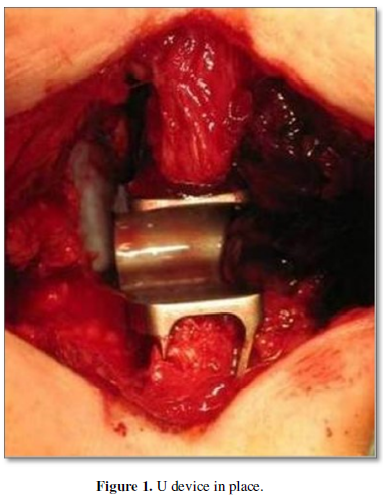
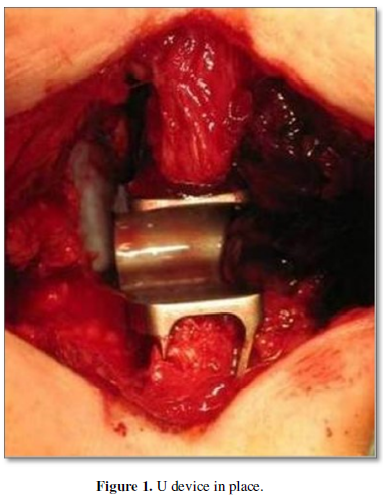
Minimally invasive techniques such as foraminotomies or augmentation of the conjunction hole through which the lumbar roots pass and place small prostheses called interspinous spacers are preferable (U device) increase the diameter of the vertebral canal (Figure 1).
The results obtained are optimal and in more than 90% of the cases the stenosis is resolved.
METHODS
We performed a Retrospective study in patients older than 75 years diagnosed with severe degenerative lumbar Canal stenosis. The variables studied were age, sex, symptoms, location, major comorbid conditions, and radiographic classification by MRI.
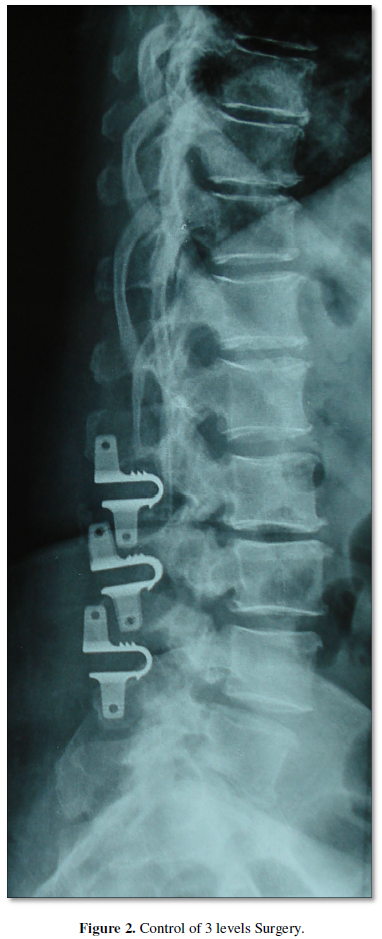
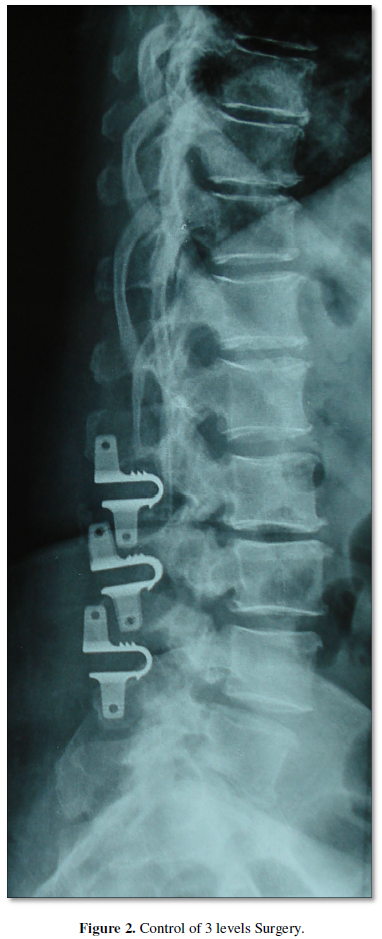
The surgical technique was the placement of the interspinous device U between the affected vertebral segment (maximum 3 levels) (Figure 2).
We used the Oswestry index and Visual Analogue Scale of pain as evaluation instruments.
RESULTS
The series was composed of 10 patients, there was a predominance of females with 67.6%.
The predominant symptom was Lumbar pain and claudication. The Oswestry index and visual analog scale pain showed significant improvement in postoperative and obtained 95% of Excellent results.
DISCUSSION
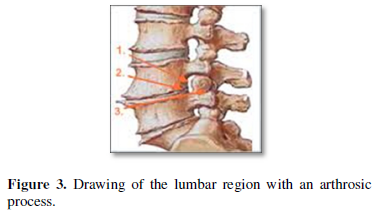
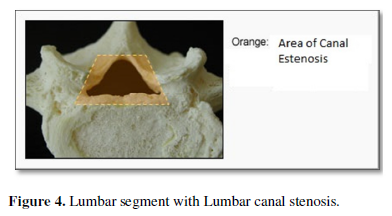
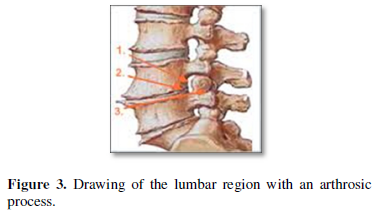
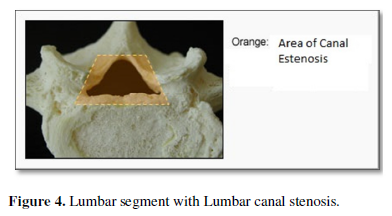
The degenerative joint processes that occur over the years and affect bone, capsular and ligamentous structures are known as osteoarthritis; It is a process where the ligaments hypertrophy and the joints acquire a "spindle" shape by widening laterally. When this degenerative process occurs in the joints of the lumbar spine and consequently causes compression of the nerve structures, a characteristic syndromic picture known as degenerative lumbar stenosis is produced (Figures 3 & 4).
This set of symptoms and signs is becoming more and more frequent in current medical practice, caused by the continuous and incessant increase in the age of the population.
Due to the slow progression of anatomical changes and therefore the appearance of symptoms, the diagnosis is made in most cases late or many times it is not made, which leads to the loss of the patient's activity levels and the appearance of other conditions that sometimes endanger or shorten the life of the patient.
This treatable condition is perhaps the biggest cause of inactivity, loss of productivity, and potentially of independence in many people, particularly older adults.
Some statistical data suggest that this syndrome is present in 5 out of every 1,000 Americans over 50 years of age and is one of the major causes of spinal surgery in that country; in Sweden the rate of spinal surgery for stenosis is 9.7 per 100,000 population. In the United States, the number of surgeries for this condition increased 8 times in the period 1979 to 1992 in patients older than 65 years.
Everything indicates that the degeneration of the intervertebral disc is the main cause that triggers the succession of phenomena that lead to the stenosis of the spinal canal.
The concept of three joints establishes that the intervertebral movements are generated in a large tripod, where the intervertebral disc is the anterior joint and the articular facets complete the two posterior supports of the three-joint complex [9].
Any alteration in one of these joints, which usually occurs primarily in the disc, generates biomechanical stresses on the others; which results in arthritic or degenerative changes in the articular facets with the consequent further deterioration of the disc itself. This sequence is repetitive and serious damage is established in the intervertebral movement complex [10].
The process of degeneration of the intervertebral discs and its effects on the biomechanics of the lumbar vertebral segment is a topic that has been and is investigated by many authors, who show that degenerative changes in the intervertebral disc turn the lumbar vertebral segments in their beginnings more flexible, but for the reasons stated by Kirkaldy-Willis and Farfán, the increase in mobility and instability is followed by the stabilization of the affected segment [11].
Changes in stability are mostly related to disc degeneration, but spinal degeneration occurs both in the disc and in the articular facets that constitute true synovial joints and whose degenerative changes are identical to those observed in osteoarthritis of the joint. other synovial joints. In general, osteoarthritis of the synovial joints commonly presents narrowing, deformity, instability and decreased mobility [12].
The risks that concur in these older adult patients with their biological and psychosocial characteristics progressively increase and the impact of new favorable conditions on their life expectancy decreases. Therefore, surgical interventions in older patients should be selected because they are clearly effective, with a low relative risk, and their success should be related to maximizing longevity [13].
It is demonstrated that the results found with imaging (x-rays and magnetic resonance imaging) have a logical correspondence with the physiological and pathological changes. Below we describe two possible causes of low back pain in older adults and their main manifestations.
- Lumbar canal stenosis or degenerative spondylolisthesis:
Both vertebral stenosis - the narrowing of the canal of the cervical (neck) or lumbar (back) spine - and degenerative spondylolisthesis - when one vertebra slides forward over the one below - are two conditions that appear due to the wear and tear of the joints., typical of age.
In both cases, what causes low back pain is compression of the spinal cord and the roots of the lumbar nerves. This results in the older adult experiencing acute leg pain, mainly when standing and walking normally.
Symptoms are slow to evolve and vary from severe to mild, or they may even go by for days without appearing. Other associated manifestations are:
- Inability to walk a long distance without leg pain
- Low back pain that is relieved shortly after sitting up
- Weakness, numbness, and tingling radiating from the lower back to the buttocks and legs (sciatica).
- Osteoarthritis of the facet joints
Slowly evolving degenerative condition, osteoarthritis of the facet joints causes a flare-up of low back pain accompanied by numbness, pain that is usually more pronounced first thing in the morning and again at the end of the day.
The pain is caused by the degeneration of the cartilage that separates the joint that forms the sheets of two overlapping vertebrae. In its initial phase, low back pain can be scarce, and little by little it can become more constant or even lead to sciatica.
Likewise, this type of low back pain can manifest itself in the following ways:
- Pains that interrupt sleep
- Palpable pain in a localized area of the spine
- Dull, continuous, or intermittent pain in the lower back that worsens after physical activity
- Numbness or loss of flexibility in the back resulting, for example, in the inability to bend at the waist comfortably.
Surgery Technique in elderly patients:
- Recalibration (Hemilaminectomy)
The vertebral recalibration described by Senegas in 1988 is a selective decompression of the vertebral canal that seeks to eliminate compressions on the nervous tissue and preserve stabilizing elements such as the posterior arch with the supra and interspinous ligaments, and at least two thirds of the articular facets. The intention was to preserve the mobility of the operated segment.
- Vertebral arthrodesis (Laminectomy)
In some cases, an arthrodesis (spinal fusion) may be performed at the same time to help stabilize the sections of the spine treated by decompressive laminectomy.
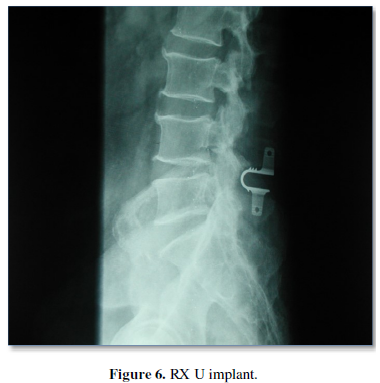
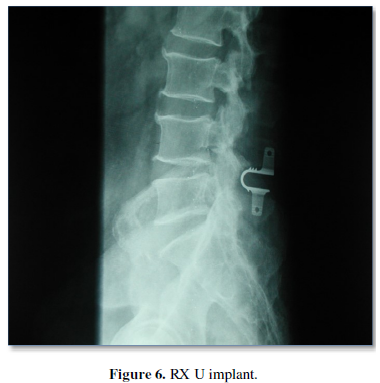
- Interspinous device U. MIS surgery (Figures 5 & 6)
An interspinous spacer is designed to treat the symptoms of spinal stenosis, a sometimes-painful condition caused by a narrowing of the spinal canal. The spacer is an implant designed to keep the space between the spinous processes open so that when you stand up, the nerves in your back do not pinch or cause pain.


By enlarging the space between the back bones, the spacer reduces pressure on the spinal nerves; in this way, it relieves the symptoms of spinal stenosis, including the following: Leg pain or cramps; Numbness or tingling in the lower back, buttocks, and legs.
The spacer is designed to stay permanently in place without the need to drive screws or tools into the bone or ligaments in your back. Because spacers generally do not require the removal of tissue or bone, normally associated with traditional back surgery, the natural anatomy of the spine is preserved.
Interspinous Spacer was conceived to act as a permanent and dynamic implant for use from L1-L5 We developed U N6 for L5 S1 (Figure 7).
The Interlaminar Technology of the Implant was also designed to control mobility, extension and flexion in the lower back.


CONCLUSIONS
-
The implant avoids overloading the adjacent level.
-
Allows mobility in flexion and extension, expanding the foramina and the medullary canal.
-
The implantation procedure is minimally invasive and reversible.
-
Allows to preserve most of the anatomical structures intact.
-
The interspinous stabilization with the implant is ideal in cases of facet arthrodesis.
-
The implantation of the device allows the stabilization of the segment.
-
Control the movement.
-
Reduces tensions in the posterior joints.
-
Above all, it partially modifies lordosis and opening the foramen.
- Carlos SC, Rafael RH, Ernesto FM (2009) Surgical treatment of lumbar canal stenosis. Rev Cubana Ortop Traumatol [magazine on the Internet].
- Verbiest H (1954) A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J Bone Joint Surg Br 36-B(2): 230-237.
- Kirkaldy-Willis WH, Wedge JH, Young-Hing K, Reilly J (1978) Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine 3(4): 319-328.
- Senegas J (1988) Revue de chirurgie orthopedique et reparatrice de l´appereil moteur. J Orthop Surg 2: 93-99.
- Steven R (2010) Garfin Bjorn L.: Rothman-Simeone. The Spine: 5th edn, Capitulo 30, W. B. Saunders. pp: 797.
- Zhou G-Q, Yang F. Leung VVL, Cheung KMC (2008) Molecular and cellular biology of the intervertebral disc and the use of animal models. Curr Orthop 22: 267-273.
- Singh K, Masuda K., Thonar EJ-MA, An HS, Cs-Szabo G (2009) Age-Related Changes in the Extracellular Matrix of Nucleus Pulposus and Anulus Fibrosus of Human Intervertebral Disc. Spine 34(1): 10-16.
- Shabat S, Folman Y, Leitner Y, Fredman B, Gepstein R (2007) Failure of conservative treatment for lumbar spinal stenosis in elderly patients. Arch Gerontol Geriatr 44: 235-241.
- Li A-M, Li X, Yang Z (2017) Decompression and coflex interlaminar stabilization compared with conventional surgical procedures for lumbar spinal stenosis: A systematic review and meta-analysis. Int J Surg 40: 60-67.
- Kong C, Lu S, Hai Y, Zang L (2015) Biomechanical effect of interspinous dynamic stabilization adjacent to single-level fusion on range of motion of the transition segment and the adjacent segment. Clin Biomech (Bristol, Avon) 30(4): 355-359.
- Kuang M-J, Han C, Ma J-X, Li F, Zhao J, et al. (2016) The efficacy of intraoperative autologous platelet gel in total knee arthroplasty: A meta-analysis. Int J Surg 36(Pt A): 56-65.
- Musacchio MJ, Lauryssen C, Davis RJ, Bae HW, Peloza JH, et al. (2016) Evaluation of decompression and interlaminar stabilization compared with decompression and fusion for the treatment of lumbar spinal stenosis: 5-year follow-up of a prospective, randomized, controlled trial. Int J Spine Surg 10: 6.
- Yuan W, Su Q-J, Liu T, Yang J-C, Kang N, et al. (2017) Evaluation of Coflex interspinous stabilization following decompression compared with decompression and posterior lumbar interbody fusion for the treatment of lumbar degenerative disease: A minimum 5-year follow-up study. J Clin Neurosci 35: 24-29.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)









