Review Article
Esophageal Cancer and Genetic Analysis Using High Throughput mass ARRAY technique-A Review
4746
Views & Citations3746
Likes & Shares
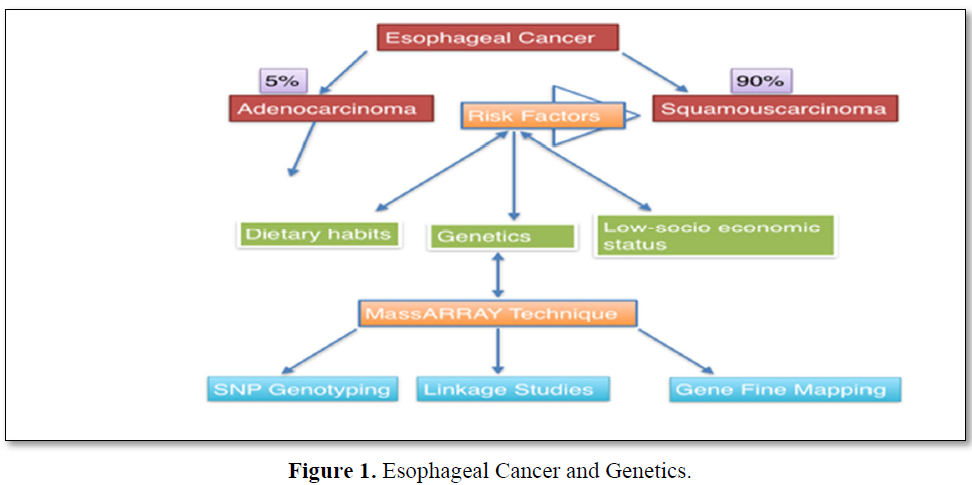
Esophageal Cancer is the eight most commonly found cancers and is a male dominant type of cancer. The prevalence of esophageal cancer varies where 90% are squamous esophageal carcinoma and 5% are adenocarcinoma. Esophageal Cancer incidences are mostly found in Northern central parts of China and Northern Iran. The risk factors which are associated with esophageal cancer are usually poor dietary habits, poor oral hygiene and low-socio economic status and genetics. Mass Array is a high-throughput technique used for the calculable test to check the differences of gene expression in multiple samples. Genotyping through Mass Array is a cost-effective technique and also provides a proper track to detect the heritable dissimilarities through high-throughput next generation sequencing (NGS).
Keywords: Esophageal cancer, Esophageal squamous carcinoma, Adenocarcinoma, Mass Array, NGS, Genotyping
INTRODUCTION
Esophageal cancer is one of the eighth most common cancer and male dominant aggressive type of malignancy which remains least studied due to its poor survival rate [1-3]. Esophageal Cancer is further divided into two major histological cancers Esophageal Squamous cell carcinoma (ESCC) and Adenocarcinoma (ACE). Both the cancers share high mortality rate [2]. Esophageal Squamous cell carcinoma is that type of epithelial malignancy which arises from the prickle-squamous cell layers of epidermis and shows keratinocytic differentiation. Adenocarcinomas of esophagus are the uncommon neoplasms with a poor prognosis. The prevalence of esophageal cancer varies where 90% are esophageal squamous cell carcinoma (ESCC), 5% are esophageal adenocarcinoma (EAC) while as other 5% includes rare malignancies [3].
The risk factors involved in prevalence of esophageal cancers have been associated with factors like lifestyle, dietary habits, low socio-economic status, poor oral hygiene, and genetics [4]. One of the major risk factors associated with esophageal cancers is genetics where loss or gain of chromosomes, gene amplification and microsatellite instability could enhance the risk of leading to esophageal cancer [3]. A survey by Global Cancer incidence, mortality and prevalence number (GLOBOCAN) in 2018 reported
about 572,034 new esophageal cases and 508,585 deaths due to esophageal cancer worldwide [5].
The highest incidence of esophageal cancer has been seen along North Central China to Northern Iran and among these most of the deaths occurs in Republic of China [6]. In Asia, squamous cell carcinoma is the major type of cancer which is rapidly increasing. In one of the studies, it is seen that Eastern Asia and Southern Africa have the highest rates of esophageal cancer, whereas Europe and North America shows the lower rates of esophageal cancer [7-9]. In North-eastern states of India like Assam, Meghalaya, Mizoram and Nagaland, it was observed to have the highest cases of
esophageal cancers in both men and women. In North-eastern states of India like Assam, Meghalaya, Mizoram and Nagaland, it was observed to have the highest cases of esophageal cancers in both men and women. Moreover, the region of Jammu and Kashmir in India has also been considered as an epidemic cancer zone [8].
GENETICS-MASS ARRAY TECHNIQUE
To know the genetic variants which are associated with esophageal cancer there are many techniques like pyro sequencing, Sanger sequencing, mass array which are used for genotyping analysis. Above all techniques mass array is considered to be more accurate and cost effective and it shortens the time by 12 h when it is compared to Sanger sequencing. Mass array could easily obtain several SNPs per test. The Mass array system is an accessible platform with a suite of research applications for both quantitative and qualitative nucleic acid assay design and fast time to time results. This system is widely being adopted for many genomic applications including gene fine mapping, validation of genome-wide association studies, linkage studies etc.
A highly accurate, sensitive, and high-throughput method for quantitative analysis of gene expression variations in multiple samples have been devised of which Mass ARRAY is one of the finest techniques for SNP genotyping. This method combines competitive PCR with matrix assisted laser desorption ionization-ionization-time of flight (MALDI-TOF) mass spectrometry by which SNP genotyping is validated to observe gene variants through a high-throughput Next-generation sequencing (NGS).
In one of the studies in J&K-India [9], 12 single nucleotide polymorphisms (SNPs) related to specific genes involved in ESCC have been studied which includes genes TCF21, CYP19A1, TERT, ERCC5, PIK3CA, REV1, FGFR2, GSTP1, TERF2, DCC and BCL2. Moreover, this study also tries to expedite the relation of genetic and environmental factors with the occurrence of ESCC. Out of 12 SNPs investigated, two of the genes showed significant association with ESCC and there were 9 SNPs showing non- significant relationship in J&K population. However, this study needs to be replicated in large cohorts to further validate this claim [9].
In another study involving Zhejiang Eastern population, the mass ARRAY technology was used to investigate 24 genetic variants in association with Esophageal cancer and it was observed that ESCC was associated with rs2188136 and negatively associated with rs10895458 and rs875339 [10].
Mass ARRAY technology has been used in Kazakh population to analyze the DNA methylation of 32 CpG sites within miR-203 in ESCC patients. It has shown that miR-203 is a potential biomarker in ESC [11].
In a study involving Chinese population, the genotypes were determined by MALDI-TOF MS and it was observed that rs2274223 of PLCE1 was associated with the higher risk of esophageal cancer [12] (Figure 1).
CONCLUSION
Mass array is a high through put technique that helps to investigate genetic variants associated with ESCC. ESCC is one of the most prevalent cancers and this technique is highly beneficial in investigating the genetic variants in association with this dreaded disease. In future, the genes explored by this technique can be used as important biomarkers that can help in early diagnosis.
- Abbas G, Krasna M (2017) Overview of esophageal cancer. Ann Cardiothorac Surg 6(2): 131-136.
- Holmes RS, Vaughan TL (2007) Epidemiology and pathogenesis of esophageal cancer. Semin Radiat Oncol 17(1): 2-9.
- Mir MM, Dar NA (2009) Esophageal Cancer in Kashmir (India): An enigma for researchers. Int J Health Sci (Qassim) 3(1): 71-85.
- Zhang Y (2013) Epidemiology of esophageal cancer. World J Gastroenterol 19(34): 5598-5606.
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, et al. (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6): 394-424.
- Hongo M, Nagasaki Y, Shoji T (2009) Epidemiology of esophageal cancer: Orient to Occident. Effects of Chronology, Geography and Ethnicity. J Gastroenterol Hepatol 24(5): 729-735.
- Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, et al. (2013) GLOBOCAN 2012 v1. 0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. IARC, Lyon, France.
- Rasool MT, Lone MM, Wani ML, Afroz F, Zaffar S, et al. (2012) Cancer in Kashmir, India: Burden and pattern of disease. J Cancer Res Ther 8(2): 243-246.
- Shah R, Sharma V, Bhat A, Singh H, Sharma I, et al. (2020) Mass ARRAY analysis of twelve cancer related SNPs in esophageal squamous cell carcinoma in J&K, India. BMC Cancer 20(1): 497.
- Wang KL, Chen XL, Lei L, Li P, Hong LL, et al. (2019) Validation study of susceptibility loci for esophageal squamous cell carcinoma identified by GWAS in a Han Chinese subgroup from Eastern China. J Cancer 10(16): 3624-3631.
- Cui X, Chen X, Wang W, Chang A, Yang L, et al. (2017) Epigenetic silencing of miR-203 in Kazakh patients with esophageal squamous cell carcinoma by Mass ARRAY spectrometry. Epigenetics 12(8): 698-707.
- Gu H, Ding G, Zhang W, Liu C, Chen Y, et al. (2012) Replication study of PLCE1 and C20orf54 polymorphism and risk of esophageal cancer in a Chinese population. Mol Biol Rep 39(9): 9105-9111.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Spine Diseases
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- International Journal of AIDS (ISSN: 2644-3023)




