4646
Views & Citations3646
Likes & Shares
MATERIALS AND METHODS
Collected in our hospital between April 2014 and October 2017 hospitalized cases of hand, foot and mouth disease, according to the condition is divided into intensive (cure) and critical (death) group, respectively from infection and ICU cases, diagnostic classification according to the ministry of health of the People's Republic of China promulgated the "hand, foot and mouth disease diagnosis and treatment guidelines (2010 edition)" [4] standard execution, and peripheral blood test positive for intestinal virus EV71 - IgM, ruled out all kinds of chronic disease cases in at the same time. In the severe (cured) group, there were 25 cases, including 14 males and 11 females, with an average age of (2.23±1.12) years. In the critical (dead) group, there were 22 cases, including 12 males and 10 females, with an average age of (2.12±1.09) years. 30 healthy children who underwent physical examination in the outpatient department of our hospital at the same time were randomly selected as the (healthy) control group, including 17 males and 13 females, with an average age of (2.31±1.35) years old. There was no statistically significant difference in gender and age between the control group and the other 2 groups (P>0.05). This study was approved by the ethics committee of the hospital, and all treatment regiments were examined with the informed consent of the patient's family members.
Scientific research designed that all cases were grouped according to their disease, system and system level. According to the condition into severe (cure) groups, critical (death) group and control group (healthy), according to the system above cases can be divided into the immune system and other systems group, according to the rank order from small to large systems will set immune system into the lymphocyte subgroup and the lymphocyte neutrophils system (lymphatic neutral system) two groups, the lymphocyte subgroup by respectively reflect the blood to the total number of T lymphocytes (CD3 + T) and reflect the blood to the total number of B lymphocytes (CD19 + B), lymph neutral system by the blood to the total number of lymphocytes (L) and blood to the total number of neutrophils (N), Blood CD3+T (%), CD19+B (%), L (%) and N (%) were selected as observation indicators, and blood white blood cell count (WBC), c-reactive protein (CRP), blood glucose (GLU) and platelet count (PLT) were selected as observation indicators in other system groups.
Methods specimen collection peripheral venous blood was collected from all cases included in the scientific research group upon admission. Roche 400 Plus automatic biochemical analyzer was used to test GLU and CRP. Mindray bc-3000 blood routine analyzer, test items are L (%), N (%), WBC, PLT. CD3 + T and CD19 + B in peripheral blood were determined by BD FACS CantoII flow cytometry and its associated lymphocyte subsets. All the experimental methods (inter-laboratory control) were approved by human clinical laboratory center.
SPSS 18.0 statistical software was used to analyze the above data. The measurement data were expressed as mean ± standard deviation (x± s). One-way analysis of variance was used for comparison among multiple groups, and P < 0.05 was considered as significant difference. P < 0.01 indicates a significant difference.
RESULTS
The immune system in lymphocyte subgroup and lymphatic neutral group each observation data comparison, the lymphocyte subsets CD3 + T (%) and CD19 + B (%) in the control group (healthy), severe (cure) and critical (death) group presents the opposite change tendency, CD3 + T (%) with the deterioration of the illness is reduced, and CD19 + B (%) increased with the deterioration of the condition, the results showed that the illness condition group lymphocyte subsets CD3 + T (%), CD19 + B very significant difference (%), were statistically significant (F = 55.7, 78.3, P < 0.01); Lymphatic neutral group in the control group (healthy), severe (cure) and critical (death) group also presents the opposite change tendency, L (%) decrease with the deterioration of the illness, N (%) increased with the deterioration of the condition, the results showed that in each disease group N (%), L was very significant difference (%), were statistically significant (F = 126.5, 141.6, P < 0.01) (Table 1).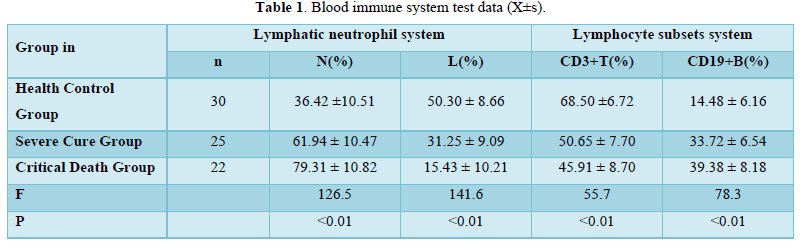
In the other system groups, WBC, CRP, GLU and PLT all increased with the aggravation of the disease in the (healthy) control group, the severe (cured) group and the critical (death) group, and the differences in the values of the research groups were statistically significant (F=65.3, 10.7, 33.9, 47.4, all P <0.01), as shown in Table 2.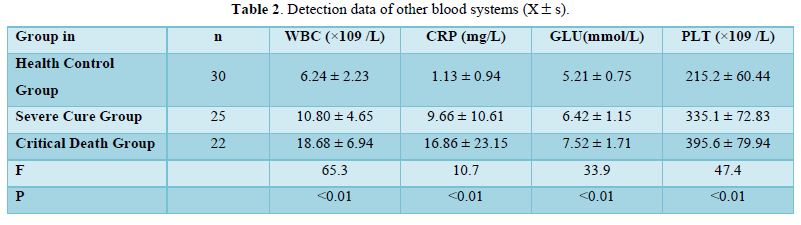
DISCUSSION
"Compensation" is a common phenomenon in natural organisms, and the law of "compensation" is similar to the philosophy of natural science in the field of medicine. Study of the pathogenesis of sepsis in the past few decades is more through local inflammatory cells, inflammatory mediators and cytokines micro field, but on the whole (system) research work is less, the research work is similar to "didn't see the forest for the trees," the situation, with the deepening of the clinical research, although people have been increasingly concerned its immunological pathogenesis, but still hasn't been a breakthrough in terms of research findings, the study of the past few decades the practice proved: asking people at a higher Angle wider field of vision to understand the pathogenesis of sepsis inherent law. In recent years, some scholars have used the viewpoint of "system theory" to theoretically discuss the pathogenesis of sepsis on the basis of the systemic equilibrium of "immune network (innate immunity → antigen presentation → adaptive immunity)", and put forward the theoretical viewpoint of "compensation/decompensation" of innate immunity and maximum activation of adaptive immunity [3]. View of system theory:
- The system is composed of interrelated elements; each part of the system is independent, but also interrelated and interdependent.
- The system has integrity: the components of the system are not a simple aggregation that can be separated, but a whole formed in a regular and certain way.
- The system is hierarchical: each system can be attributed to a larger system [5].
Due to the unclear understanding of the pathogenesis of sepsis, some medical papers on the immunopathological mechanism of HFMD in the past failed to reach a clear conclusion, and the discussion was often ended with immune dysfunction [8]. In this paper, in addition to discussing the results of this study, we will also discuss some research results of medical colleagues in the past and conduct clinical test of the new ideas. Based on years of accumulation of research on HFMD sepsis, this study still selects cases of HFMD sepsis for research and discussion. Compensated in order to better understand different immune function group differences, not copy first by different cardiac function in individuals with visual image as an example of analogy analysis, each bo cardiac output and heart rate as the cardiac function system (cardiac output) two elements, two components compensate each other to follow the system function maximization principle [9], assume that cardiac function of two different individual heart load equal (cardiac output), cardiac output = every cardiac output by the heart rate, cardiac function better individual main performance for each Po cardiac output reserve function stronger (compensatory potential is larger), first can increase per bo cardiac output compensation is more efficient, Therefore, compensation by increasing heart rate is less; On the contrary, individuals with poor cardiac function have lower reserve function of output per cardiac wave. In order to ensure the same cardiac output, it is more necessary to compensate by increasing heart rate. The system compensates with a specified degree, and if the specified degree is exceeded, functional decompensation will occur [5]. The function compensation of immune system was analyzed by analogy according to the law of cardiac function compensation. The immune system is composed of innate immunity and adaptive immunity. The adaptive immune system is composed of cellular immunity and humoral immunity. For the convenience of discussion, here temporarily by the immune system is composed of adaptive immunity and inherent immunity is discussed, under the precondition of the same infection, compare the immune function of different two individual compensatory response, the immune function of relatively strong individual mainly for adaptive immune function is stronger, the first can be compensated by activating efficient adaptive immunity, less natural immune compensatory; However, individuals with relatively weak immune function have lower adaptive immune reserve function, which can only maintain the balance of the system by activating innate immune compensation, and the inflammatory response is enhanced [3]. According to the above analysis, immune function is the performance of mutually compensatory optimization and maximization of various elements in the immune system. The stronger the immune function, the greater the potential of adaptive immune activation compensation, the less the intrinsic immune compensation, the lighter the inflammatory response and the lighter the disease. Conversely, the more severe the disease. Through the above multi-system demonstration, it is further proved that the compensation law is universal. The author view is the body of hand, foot and mouth disease intestinal virus immune response mainly through cellular immunity [10,11], humoral immune enhancement is compensatory reaction, more severe, critically ill children with hand, foot and mouth disease clinically defects associated with different levels of immune function, this is mainly related to human genetic polymorphism which [12-14], The results of this study support the author's opinion and are consistent with the results of most medical peer reports [15,16]. According to the sequence of system grade from small to large, the lymphocyte subgroup system and the lymphoid neutral system were selected for observation. The lymphocyte subgroup system was composed of CD3+T reflecting cellular immunity and CD19+B reflecting humoral immunity. The lymphatic neutrophilic system is composed of two elements: L reflecting adaptive immunity and N reflecting innate immunity. It can be seen from table 1 that the two components of the lymphocyte subgroup system, namely CD3+T and CD19+B, show a reciprocal trend, and the disease shows a significant negative correlation with CD3+T (%) and a significant positive correlation with CD19+B (%), which conforms to the balance compensation law of the above system. The two components of the lymphatic neutral system, namely adaptive immunity L and innate immunity N also follow the law of reciprocal compensation, and the disease has a significant positive correlation with N (%) and a significant negative correlation with L (%) [17]. The corollary: hand, foot and mouth disease sepsis immune pathological mechanism is due to the cellular immune deficiency, first through the humoral immune compensatory/decompensation, lead to adaptive immunity compensatory/decompensation, ultimately through the inherent immune compensatory/decompensated, higher percentage of neutrophils progressive, reflect systemic inflammatory response index the WBC and CRP with increasing aggravation of progressive as shown in Table 2 [18], it also conforms to the system theory system has a hierarchical, each system can be relegated to a larger system [5] law of compensation. Sepsis can affect the neuro-endocrine-immune network [19], and the body produces a stress response by secreting adrenocorticotrophin from the pituitary gland to raise blood sugar. This study supports the above view, as shown in table 2. Sepsis can lead to blood coagulation dysfunction [20], incidence of along with the aggravation of platelet count, as shown in table 2, can be understood as a coagulant function abnormality early response, PT, TT, aTTP, Fbg abnormal in most of the cases is not obvious [21], may be related to viral sepsis activation of blood coagulation system function as inferior to bacterial sepsis. Disorders of the neuro-endocrine-immune and clotting systems resulting from sepsis can be considered as a systemic compensatory response on a larger scale. The results of this study showed that the immune mechanism of sepsis in hand, foot and mouth disease (HFMD) all levels of the blood system followed the law of systemic equilibrium compensation, and the levels of the blood system from small to large continuous response induced the intrinsic immune compensation/decompensation and a larger range of compensatory inflammatory responses.
- Yao Y-Y, Zhang Y-M (2017) A new understanding of the pathogenesis of sepsis J. J Graduate Med Sci 30(7): 678-683.
- Qiu Y, Guo-Wei T, Min-Jie J, Yang C, Luo Z (2019) The Immune System Regulation in Sepsis: From Innate to Adaptive. Curr Protein Pept Sci 20(8): 799-816.
- Yao L-L, Yang X, Hua-Qing T (2016) Rational analysis of pathogenesis of systemic inflammatory response syndrome. J Med Philos 37(1B): 79-81.
- The ministry of health of the People's Republic of China, foot and mouth disease diagnosis and treatment guidelines 2010.
- Da-Rin HE (2005) Introduction to philosophy of medical science and technology [M]. Beijing: higher education press pp: 175-191.
- Wang S-M, Lei H-Y, Huang K-J, Wu J-M, Wang J-R, et al. (2003) Pathogenesis of enterovirus 71 brainstem encephalitis in pediatric patients: Roles of cytokines and cellular immune activation inpatients with pulmonary edema. J Infect Dis 188(4): 564-570.
- Gu-Lung L, McGinley JP, Drysdale SB, Andrew JP (2018) Epidemiology and Immune Pathogenesis of Viral Sepsis. Front Immunol 9: 2147.
- Wang J, Chen D, Zhao XF (2008) Level analysis of immune-related indicators in children with EV71 hand-foot-mouth disease. Chin J Nosocomial Infect Dis 28(14): 2197-2201.
- Yao L-L, Chen W, Du Y-H, Li C-L, Luo Y-W, et al. (2013) Immune mechanism of systemic inflammatory response syndrome in hand, foot and mouth disease. J Med Philos 34(2B): 78-89.
- Zhang Y, Yang E, Pu J, Liu L, Che Y, et al. (2014) The gene expression analysis of peripheral blood mononuclear cells in rhesus infants and the significance in pathogenesis. PLoS One 9: e33766.
- Song J, Hu Y, Hu Y, Wang J, Zhang X, et al. (2016) Global gene expression analysis of peripheral blood mononuclear cells in rhesus monkey infants with CA16 infection-induced HFMD. Virus Res 214: 1-10.
- Namath A, Patterson AJ (2009) Genetic Ploymorphisms in sepsis. Crit Care Clin 25(4): 835-836.
- Mao Z, Zhang SL, Feng B (2017) Association of IL-10 (-819T /C,-592A /C and -1082A /G) and IL-6 -174G /C gene polymorphism and the risk of pneumonia-induced sepsis. Biomarkers 22(2): 106-112.
- Chen l, Diao B, Yan DQ (2019) Correlation between the polymorphism of hla-drb1 gene and susceptibility to sepsis in children. South China J Defense Med 33(07): 468-472.
- Wang J, Deng HL, Yuan J (2017) The relationship between lymphocyte subpopulation imbalance and EV71 hand-foot-mouth disease. Chin J Exp Clin Infect Dis 11(2): 156-161.
- Hui-Ling D, Xiao-Kang W, Yu-Feng Z (2017) Analysis of immune function in 108 children with severe hand-foot-mouth disease. Shaanxi Med J 46(5): 556-558.
- Yi Z, Yuan Z, Min W (2008) Correlation analysis of blood routine changes and prognosis in patients with sepsis. Chongqing Med Sci 47(35): 4548-4550.
- Ran F, Wang Y, Zhong L, Liu Z, Duan R, et al. (2016) The relevance of the serum levels of C-reactive protein and creatine kinase-MB to the severity of hand-foot-and-mouth disease patients in China: A meta-analysis. Pediatr Infect Dis 8(1): 15-25.
- Kasahara E, Inoue M (2015) Cross-talk between HPA-axis-increased glucocorticoids and mitochondrial stress determines immune responses and clinical manifestations of patients with sepsi. Redox Rep 20(1): 1-10.
- Saracco P, Vitale P, Scolfaro C, Pollio B, Pagliarino M, et al (2011) The coagulopathy in sepsis: significance and implications for treatment. Pediatric Rep 3(4): e30.
- Jun L, Dan-Dong H, Jing W (2008) Changes and clinical significance of clotting function in children with critical hand-foot-mouth disease EV71. Thrombus Hemostasis 24(03): 439-441.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- International Journal of Diabetes (ISSN: 2644-3031)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)


