Mini-Review
Porous Coated Cement Less Total Hip Arthroplasty: Minimum 5 Year Follow-up
4454
Views & Citations3454
Likes & Shares
Despite total hip arthroplasty having successful outcomes, previous cement less femoral stems displayed thigh pain and stress shielding. Through several design changes, modern cement less total hip arthroplasties have solved these concerns. This study’s cohort consisted of 100 consecutive cement less total hip arthroplasties. Low complication rates, excellent survivorship and Harris hip scores were observed at final follow up. The modern cement less total hip arthroplasty allows the surgeon excellent Harris Hip Scores, low revision rates and no thigh pain.
INTRODUCTION
While total hip arthroplasty has been named the surgery of the century [1], the outcomes are correlated to the orthopedic surgeon’s ability to correctly contour the proximal femur to accept the cement less implant [2]. Due to the fact that cemented stems often loosen, particularly in younger patients [3,4], and most surgeons have turned to cement less implants.
Modern implants are designed with proximal porous coating and pronounced tapers in an effort to decrease thigh pain and limit stress shielding to the proximal femur. To maximize the stress transference of the implant to bone, modern implants are constructed with titanium alloys to more closely mimic the physiological stress of native bone. This study aims to report 5 year follow up of 100 consecutive total hip arthroplasties and to evaluate Harris Hip Scores in these patients.
MATERIALS AND METHODS
Implant design
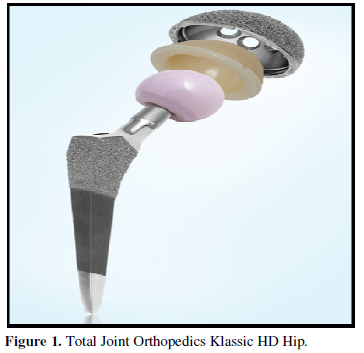
This study’s implant consisted of a double wedge Zweymuller-type stem made of a titanium alloy designed by Total Joint Orthopedic, Inc.’s. This Classic HD® stem (Figure 1) features a proximal porous Ti-Coat®, titanium ultra-porous coating (>60% porosity), for bony in-growth while the mid-stem is designed for bony on growth by finishing the stem with a grit-blasted titanium. The femoral prosthesis is non modular and collarless and comes in both 121- and 131- degree neck shaft angle constructs.
The hemispherical acetabular cup is made of a titanium alloy with Ti-Coat ultra-porous coating. All patients received a standard flat faced highly cross linked polyethylene and acetabular component fixation was augmented in all cases with the use of can cellous bone screws.
Study design
A retrospective chart review of 100 consecutive total hip arthroplasties performed in 2013 and 2014 was performed. All surgeries were performed by the senior author (AAH) using a posterior lateral approach; a cement less Classic HD acetabular cup and femoral stem with either a 32mm or 36mm head was implanted in all cases. Postoperative recovery included full protected weight bearing immediately after surgery for 6 weeks, followed by weight bearing with a crutch or cane until the patient no longer had a discernable limp. Pharmacological anti-coagulation consisted of warfarin 5mg with an INR goal of 2.0 for 3 weeks followed by 81mg ASA for 3 months postoperatively. Follow up was performed at three and six weeks; three, six and nine months and then annually thereafter. Detailed physical examination and radiographic evaluation was performed at each follow up visit and Harris Hip Scores were calculated at final follow up. Radiographs were evaluated by an orthopedic fellow and the senior author (AAH), examining for heterotrophic bone according to the Booker classification [6], osteolytic lesions, stability, subsidence, and pedestal formation.
RESULTS
Of the original 100 participants, six patients were deceased for reasons unrelated to their hip procedure and nine were lost to follow up. Patient age ranged from 48 to 99 years old (Average 71-year-old), average weight was 89kg with 56% female participants. Harris Hip Scores at final follow up were calculated with a range of 71-100 (average of 89). Prior to the regular use of tranexamic acid, four hematomas occurred during this study period. These hematomas were successfully treated with a superficial incision and drainage, one hematoma however that was thought to be infected. One patient required a closed reduction for dislocation, and one patient had an unstable hip necessitating a constrained liner. There was a 100% and 99% survivorship of the stem and cup respectively at five-years. No hip revisions were due to pain or osteolysis and no patient complained of thigh pain. One patient developed Booker class 2 heterotrophic bone formations causing a late unstable hip who required a constrained liner for treatment.
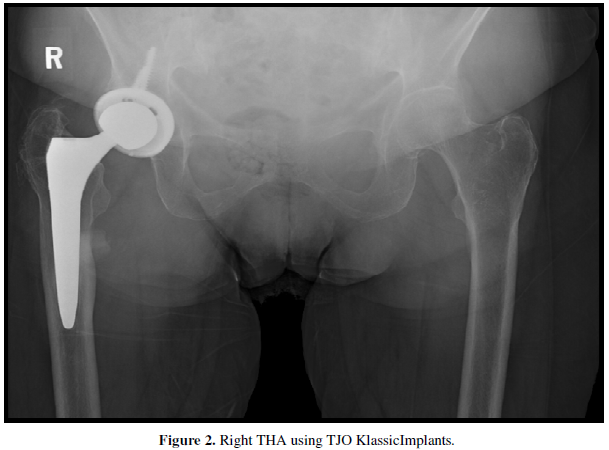
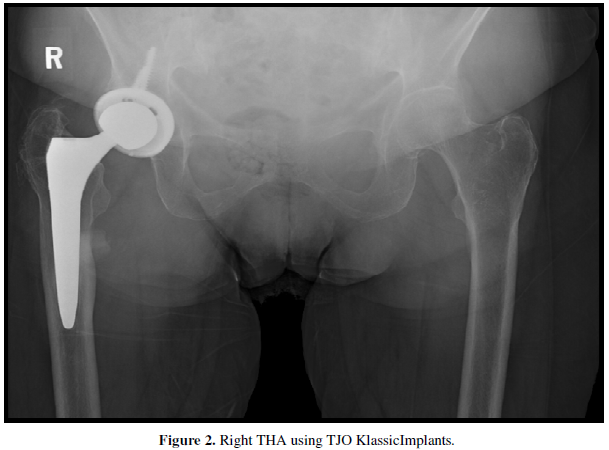
One patient with intractable psoas tendonitis, a 54-year-old female, underwent revision of the acetabular component 28 months after her initial implantation (Figure 2).
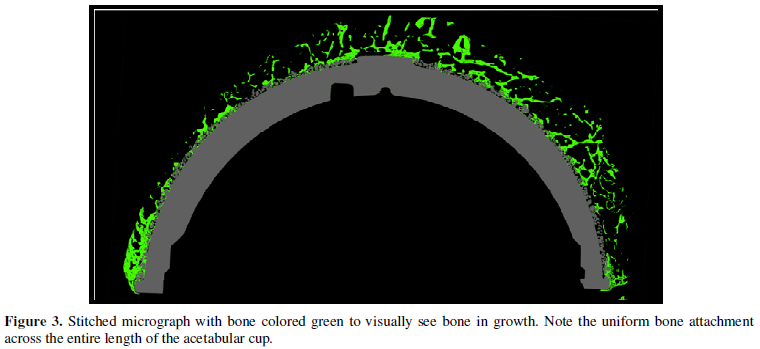
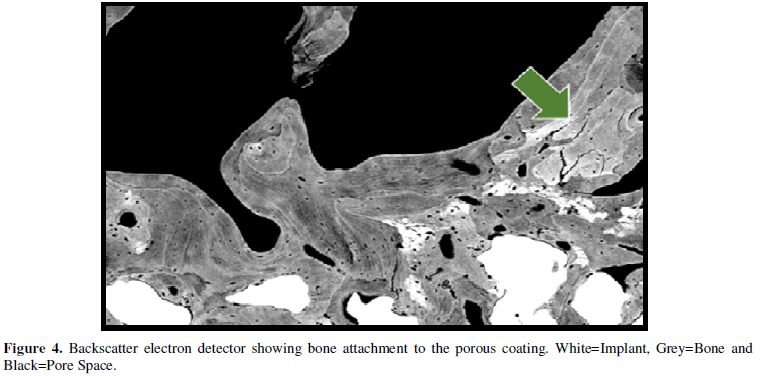
This component was treated in 10% neutral buffered formalin, dehydrated in progressively increasing concentrations of ethanol, infiltrated and fixed in polymethyl methacrylate. Following specimen hardening in PMMA, 3mm slices were divided, ground and polished. Specimens were stained and evaluated using light microscopy and images taken utilizing a scanning electron microscopy. Bone penetration was extensive demonstrating up to 54% bone present in the pore spaces of the porous coating. (Figures 3 & 4).
DISCUSSION
At 5 year follow up, cement less total hip arthroplasty is shown to be safe and effective. Hip scores and survivorship are note-worthy, revision rates are low and no patients complained of thigh pain. Several authors [4,5,7-9] have demonstrated high survivorship in similar older style femoral implants, but having high percentage of thigh pain and significant bone loss during extraction. Other modern blade style implants demonstrate improved survivorship, decreased thigh pain but higher incidences of subsidence [10]. The stem used in this study shows superior survivorship, no thigh pain and no subsidence at 5 year follow up. Survivorship of other Zweymuller style stems have been reported in the literature demonstrating 100% survivorship at 10 years [8] and nearly 96% survivorship at 25 years [11].
Of the 100 patients in this study, four hematomas occurred during this 2-year period. Hematoma formation has been documented as the third most common complication in the literature and has completely disappeared in our practice since the routine use of tranexamic acid [7]. In conclusion, this cement less total hip arthroplasty demonstrates superior Harris Hip Scores and survivorship without thigh pain or loosening.
- Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: Total hip replacement. Lancet
- Hofmann AA, Feign ME, Klauser W, VanGorp CC, Camargo MP (2000) Cement less primary total hip arthroplasty with tapered, proximally porous-coated titanium prosthesis. J Arthroplasty 15: 833-839.
- White SH (1988) The fate of cemented total hip arthroplasty in young patients. Clin Orthop 231: 29-34.
- Dorr LD, Takei GK, Conaty JP (1983) Total hip arthroplasties in patients less than forty-five years old. J Bone Joint Surg Am 65: 474-479.
- Keisu KS, Mathiesen EB, Lindgren JU (2001) The uncemented fully textured Lord hip prosthesis: A 10-to 15-year follow up study. Clin Orthop 382: 133-142.
- Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55: 1629-1632.
- Hwang S (2014) Experience of Complications of Hip Arthroplasty. Hip Pelvis 26: 207-213.
- Ottink K, Barnaart L, Westerbeek R, vanKampen K, Bulstra S, et al. (2015) Survival, clinical and radiological outcome of the Zweymuller SL/Bicon-Plus total hip arthroplasty: A 15-year follow-up study. Hip Int 25: 204-208.
- Grant P, Nordsletten L (2004) Total hip arthroplasty with the lord prosthesis. J Bone Joint Surg Am 86: 2636-2641.
- Davies MS, Hua J, Parker BC, Walker PS, Ward DA (1999) Migration of the uncemented CLS femoral component. Orthopedics 22: 225-228.
- Pardos AC, Rey EG, Cimbrelo EG (2017) Total Hip Arthroplasty with Use of the Cement less Zweymüller allo classic System. J Bone Joint Surg 99: 1927-1931.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Diabetes (ISSN: 2644-3031)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Pathology and Toxicology Research
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Allergy Research (ISSN:2642-326X)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- BioMed Research Journal (ISSN:2578-8892)






