3842
Views & Citations2842
Likes & Shares
Methods: We analyzed retrospectively 63 records of patients diagnosed with brain metastases from breast cancer and treated in the radiotherapy department at the Salah Azaiz Institute of oncology over a 5-year period between 2007 and 2011. All patients received whole-brain radiotherapy. Only 4 patients had surgical resection of the metastases before radiotherapy and 36,5% of patients received systemic treatment after irradiation.
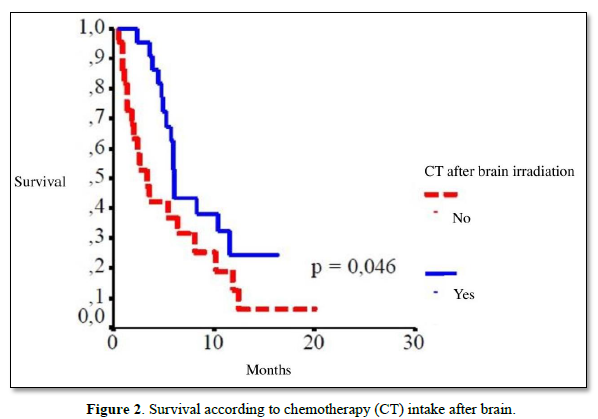
Results: Overall survival was 19% at 1-year and median survival was 4,5 months. Univariate analysis indicated that systemic treatment after irradiation was correlated significantly with longer survival. (p=0,046).
Conclusion: Determining prognostic factors might help optimize individual treatment for metastatic breast cancer. The results of our study suggest that chemotherapy is more effective on brain metastases after irradiation. This can be explained by the fragilization of the blood-brain barrier by radiation and subsequently a better passage of cytotoxic agents.
Keywords: Brain metastases, Metastatic breast cancer, Radiotherapy, Chemotherapy, Palliative care
This article aims to study the relevance of chemotherapy in the case of irradiated brain metastases of breast cancer through a sample of 63 patients treated in the radiotherapy (RT) department at the Salah Azaiz Institute of oncology.
METHODS
We conducted a retrospective study using radiotherapy data sheets and medical records and found a total of 63 patients with brain metastases of breast carcinoma treated in the RT department at the Salah Azaiz Institute over a 5-year period from January 2007 to December 2011.Serving as the national reference center for cancer surveillance, diagnosis, and treatment, the institute plays a crucial role in addressing the healthcare needs of the northern region of Tunisia.
Our patients were all female and were included regardless of their general status.
The diagnosis of brain metastases was made on computed tomography (CT) scan and/or magnetic resonance imaging (MRI). No patient had a diagnostic brain biopsy. Leptomeningeal metastases were excluded from the study.
Associated extra-brain metastases were dominated by bone metastases in 49.2%, lung in 23.8%, liver in 12.69% and lymph nodes in 7.93%.
Brain surgery was performed in 4 cases, in patients in good general condition with a single brain metastasis, alone or associated with other extracranial metastases in 2 cases.
All patients underwent whole-brain radiotherapy (WBRT) after a mean delay of 1 month from diagnosis. The doses of radiotherapy were variable.
Short-term corticosteroids were prescribed before RT or during the treatment period to prevent or reduce intracranial hypertension (ICHT).
Chemotherapy was not routinely administered after radiotherapy. Only 23 patients had or continued chemotherapy. In 19 cases and in the presence of associated extra-brain metastasis, chemotherapy was of the type of Docetaxel (15.78%), Capecitabine (47.36%), Vinorelbine-Cisplatin (31.57%) and Gemcitabine-Carboplatin (5.26%). In 4 cases, chemotherapy was initiated in the absence of extra-cerebral metastasis and was of the Capecitabine type in 3 cases and Vinorelbine Cisplatin in only one case.
Only four patients received adjuvant Trastuzumab (Herceptin®) after completion of locoregional treatment of the initial disease.
Patients were evaluated at 2 months after completion of WBRT. The evaluation was clinical. We considered the clinical response complete in case of disappearance of clinical symptoms with improvement of the general condition. Cerebral radiological control was requested in case of clinical relapse or as part of the evaluation of poly-metastatic disease.
Data entry was performed using SPSS 19 software. Overall survival was calculated from the date of diagnosis of brain metastases to the date of last visit or death. Patients alive at the time of the study were assessed at the date of their last visit. Survival estimates were made using the Kaplan-Meier method.
We set a median interval of 2 years for the occurrence of brain metastases. Any occurrence of these metastases before 2 years was considered early, and late beyond this time.
The accepted statistical value for significance was less than or equal to 0.05.
RESULTS
Descriptive study
The median age was 48 years in our series with age extremes ranging from 24 to 84 years.
The median interval between the initial diagnosis of breast carcinoma and brain metastasis was variable: 19.8 months in the absence of extra-brain metastasis, 20 months in the presence of synchronous visceral metastasis and 25 months in the case of metachronous brain metastasis. In the latter cases, the median time between brain metastasis and visceral relapse was 24 months. Associated extra-brain metastases were dominated by bone metastases in 49.2%, lung metastases in 23.8%, liver metastases in 12.69% and lymph node metastases in 7.93%.
The occurrence of brain metastasis was early in 35 cases (55.56%) and late in 28 cases (44.44%). Brain metastasis was the only site of metastatic relapse in 21 cases. Eighteen patients had a single brain lesion. Brain metastases were multiple in 37 cases and the number of metastases was unspecified in 8 cases.
Only one patient was re-irradiated for local brain recurrence. The clinical response after radiotherapy to the brain was complete in 24 cases (38%) after a median time of 3 weeks and stable in 9 cases (14.28%). Twelve patients progressed (19.04%) after brain irradiation. The neurological status of the patient after radiotherapy was not specified in 18 cases (28.57%). A follow-up brain scan was requested in 23 cases (36.50%). A near disappearance of lesions was observed in 8 cases, a stability of lesions in 9 cases and new lesions appeared in 6 cases after a median delay of 3 months from the end of the irradiation.
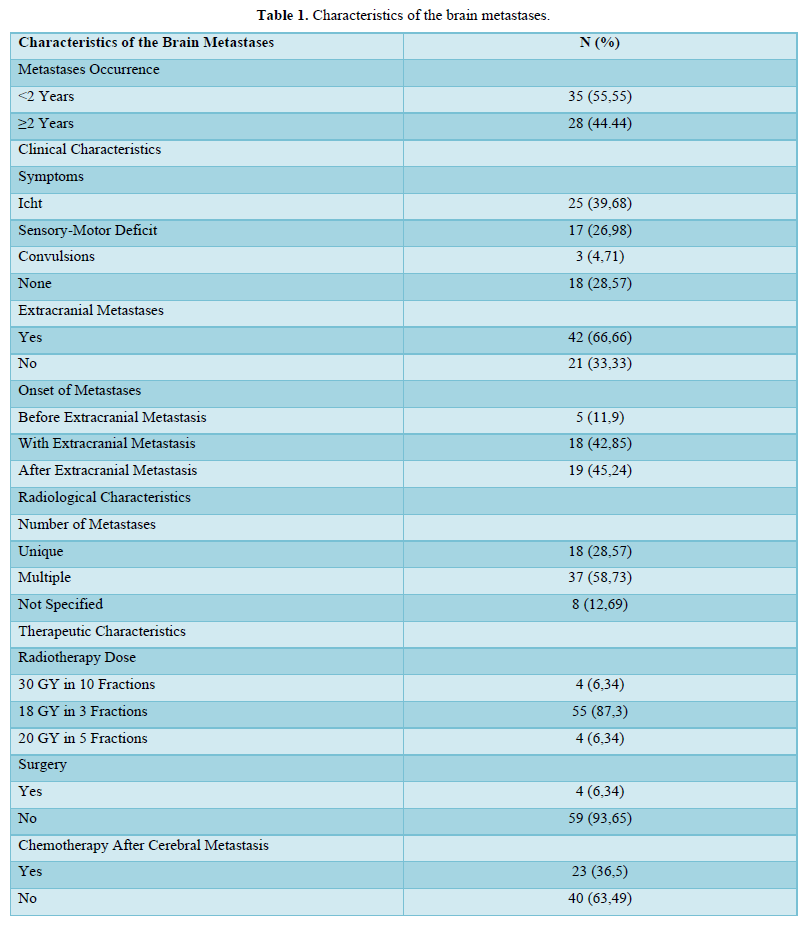
The characteristics of the brain metastases are summarized in Table 1.
Analytic study
Survival
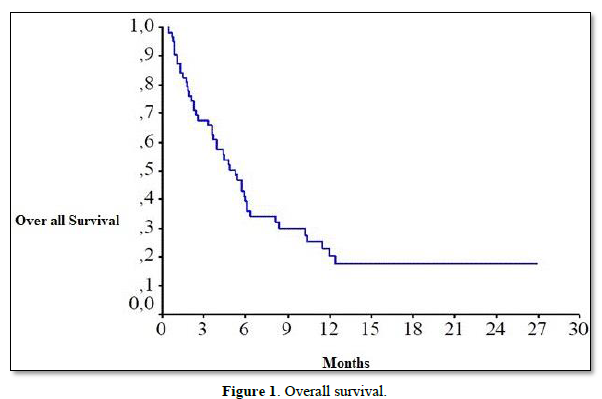
After a median follow-up of 12 months, 63 cases were analyzed. Seventeen patients were alive at the end of our study, and 46 patients had died. Because of the presence of other metastatic sites, it was difficult to specify in our study whether the cause of death was cerebral or extra cerebral progression. The median survival of our patients was 4.5 months. The overall survival was 35% at 6 months and 19% at 1 year (Figure 1).
Chemotherapy after brain irradiation
Patients who received chemotherapy after irradiation of the brain metastasis had a mean survival of 8.7 months and a median survival of 6.1 months. For patients who did not receive chemotherapy, the mean survival was 5.7 months, and the median survival was 3.6 months. The statistical difference was significant (p=0.046) (Figure 2).
DISCUSSION
In the literature, most studies have analyzed brain metastases from different primary sites. Several prognostic indexes have been established and seven prognostic classifications have been proposed [3-6], three of which are specific to breast cancer brain metastases.
Survival
According to Sperduto [7], in a retrospective multicentric study of 3940 patients with brain metastases of different primary sites, the best survival was obtained in the case of a breast primary. This survival depended on certain prognostic factors as well as the applied therapeutic protocol. It ranged from 7 months in case of treatment with radiotherapy alone, to 29.53 months in case of treatment with surgery, WBRT and stereotactic RT. According to the authors, the survival rates of this series were probably overestimated because of the non-inclusion of patients not treated for brain metastases and the retrospective nature of the study. Two retrospective studies [8,9] had similar results to our study with median survival rates ranging from 5 to 7 months in patients treated exclusively with WBRT.
Chemotherapy after brain irradiation
Brain metastases are heterogeneous and prognostic factors differ from one series to another [6]. An important prognostic factor derived from this study is the prescription of chemotherapy after brain irradiation. There was a statistically significant difference in survival between patients treated by whole brain radiation followed or not by chemotherapy (p=0.0001) (34 months vs. 8 months in case of isolated brain metastasis and 13 months vs. 4 months in case of associated extracerebral metastases).
The timing of chemotherapy introduction is also a subject of discussion. Although WBRT is considered the standard treatment for multiple brain metastases, this preference has never been prospectively demonstrated [7].
In our study, the median survival was 6.1 months for patients who received systemic treatment after brain irradiation, whereas it is only 3.6 months in the absence of systemic treatment.
Prescribing or continuing systemic treatment after brain radiotherapy is therefore justified according to some authors [10-12].
The blood-brain barrier is one of the most selective in the body. It consists of capillaries with a non-windowed endothelium with continuous junctions and selective membrane transporters, constituting a physiological barrier to the passage of macromolecules.
Despite the existence of this physiological barrier, which theoretically limits their efficacy, some systemic treatments may have antitumor activity in the central nervous system [13].
The concomitant combination of WBRT and chemotherapy has several theoretical advantages: non-invasiveness and optimization of the treatment of cerebral and extracerebral disease at the same time. Several radiobiological models describe the effects of radio-chemotherapy: additive or synergistic according to spatial and temporal cooperation. The main mechanisms of synergistic effects are based on mutual radiochemical sensitization. Radio-sensitization can be achieved by chemo-induced synchronization of the cell cycle, allowing the elimination of radioresistant clones in S-phase, potentiation of double-stranded DNA damage, inhibition of DNA repair system signals. Chemotherapy also allows to fight against radio resistance mechanisms by slowing down the repopulation phenomenon and by eliminating hypoxic tumor cells [14].
The radiation-induced increase in the permeability of the blood-brain barrier would favor the increase in intraparenchymal concentrations of cytotoxic agents [15].
Systemic treatment at the time of occurrence of brain metastases improves the prognosis, including in the case of solitary brain metastasis [8,9]. These results can be explained, on the one hand by the better systemic control of extracerebral metastases by chemotherapy drugs, and on the other hand by their contribution to the local cerebral control following a weakening of the blood-brain barrier after irradiation and by resulting in their better passage through the barrier [9,16].
Thus, brain radiotherapy and chemotherapy combinations have also been proposed. Preclinical data support a synergy between some cytotoxic agents, including capecitabine and brain RT. In a retrospective series of five patients recruited between 2003 and 2005 and treated concomitantly with capecitabine 2000 mg/m2 daily and RT 30 Gy in ten fractions followed by capecitabine, there was one complete response, two partial responses, and one stability. One patient was unevaluable due to early death in the setting of respiratory distress and sepsis. The median overall survival was 6.5 months, and the tolerance was good [17].
The use of trastuzumab after brain irradiation brings not only a gain in the overall survival of Her2 neu positive patients but also a gain in the local control of brain metastases [18]. Indeed, used concomitantly with WBRT (30 Gy in 10 sessions), overall radiological response rates of 74.2% were obtained in a retrospective series of 31 patients. A complete response with disappearance of brain metastases was obtained in 19.4% of the 23 responses observed. The safety was good in this series.
These encouraging results prompted the development of a phase II trial (NCT01363986) evaluating the impact of Trastuzumab concomitantly with WBRT of breast cancer brain metastases. This study was prematurely closed due to recruitment failure.
Lapatinib, a tyrosine kinase inhibitor, partially crosses the blood-brain barrier. The effect of Lapatinib, used after irradiation of brain metastases in HER2-negative breast cancer, was initially demonstrated in two phase II studies [19] using volumetric reduction of brain metastases as the response criterion. The response rate to the defined endpoint in the second trial was only 6% in a series of 242 patients after brain irradiation and pretreatment with Trastuzumab.
Overall survival ranged from 8 to 25 months for patients treated with Trastuzumab and from 5.5 to 10 months for patients treated with Lapatinib after brain metastases.
Chemotherapy is not a therapeutic standard and recommendations have been established essentially for patients with non-small cell lung carcinoma [20]. No therapeutic protocol has been proven in breast cancer since the studies in the literature are phase II studies and no molecule has proven its efficacy in these metastases.
According to LeScodan [9], the identification of prognostic factors makes it possible to estimate survival at the time of diagnosis of brain metastases according to prognostic indexes and to classify patients into different groups to guide therapeutic management.
CONCLUSION
Diagnostic and therapeutic advances in recent decades have changed the management of brain metastases, which is now tailored to the tumor type of the initial site and to prognostic factors.
WBRT is historically considered the reference treatment for most patients, especially those with extensive intracerebral progression. Advances in targeted therapies depending on the nature of the primary have complicated the question around the role and timing of RT, and discussion of the course of treatments in multidisciplinary meetings is becoming a difficult issue.
Although addressed to patients in palliative phase, RT of brain metastases is one of the locations for which technical reflexion is the most stringent. Currently several techniques are used in RT to minimize the side effects of WBRT to preserve cognitive function, such as stereotactic RT, or WBRT with hippocampal preservation [1].
Several studies have been conducted in recent years to identify key prognostic factors for survival after brain metastasis. These results have allowed to establish prognostic scores in order to identify subgroups of patients with different prognoses, with the aim of influencing the stratification and interpretation of therapeutic trials and to ensure a better selection of patients to whom could be proposed new therapeutic strategies.
The aim of our work was to analyze the interest of chemotherapy after total brain irradiation as a prognostic factor for brain metastases of breast cancer patients. Indeed, we found in univariate analysis that pursuit of chemotherapy after brain metastases is a prognostic factor for long survival (p=0.046).
Although our cohort included patients treated between 2007 and 2011, when stereotactic RT was not available yet at our department, and Trastuzumab was not as accessible as it is now, we emphasized the role of continued chemotherapy. Despite the existence of the physiological blood-brain barrier that theoretically limits its efficacy, some systemic treatments may have antitumor activity in the central nervous system.
The future development of specific recommendations for the multidisciplinary management of patients with brain metastases from breast cancer seems relevant in view of the stakes involved and the diversity of situations encountered.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Journal of Rheumatology Research (ISSN:2641-6999)




