5494
Views & Citations4494
Likes & Shares
Purpose: The purpose of this systematic review is to identify the prevalence of infertility among women with post-graduate education and the factors that contribute to infertility in female physicians including specialty/training, professional environment on fertility, and utilization of assisted reproductive technologies to conceive in comparison to the general female population.
Methods: By searching PubMed and EMBASE, we performed an extensive literature search to examine the prevalence of infertility in women with post-graduate education.
Results: Six papers were eligible for the study. In comparison to the general population, American female physicians are more likely to delay childbearing and experience more pregnancy complications. On average, female physicians' age at first attempt of conception was 30.6. It was found that female physicians, in particular surgeons, utilize assisted reproductive techniques more frequently than the general population. Female physicians also experience professional stressors including increased workload, shift work, variability in length of maternity leave, and perceived animosity towards pregnancy from other colleagues which may contribute further to fertility issues and pregnancy complications.
Conclusion: Female physician infertility is multifaceted, with the primary reason for delaying first attempt at conception being length of training. Stress from increased workloads and demands, shift work affecting hormones, and perceived stigmas of pregnancy and maternity leave during residency training impact fertility. By creating flexible workplace policies for parental leave and addressing the biased culture against childbearing in the medical system, we may begin to see a reduction in guilt/anxiety by female physicians and alleviate the tension among all physician colleagues.
Keywords: Physician infertility, Infertility, Female physicians, Family planning
BACKGROUND
With the increase of women in post-graduate education, more women face challenges with family planning and fertility due to the high demands of extensive schooling and training. Pursuit of advanced degrees has been linked to unintended childlessness [1]. Nearly 85% of female physicians want to start families of their own; however, many women in post-graduate education delay childbearing, which risks their fecundity as fertility declines with increasing age [2]. Around the age of 30, the rate of fertility decreases and higher risk of complications with maternal and fetal health during pregnancy arise past the age of 35[3]. During the most proximal age period for childbearing, female physicians are usually in the middle of their medical training. Although attention has been given to the reproductive health of women overall, there has been minimal attention to address the prevalence of reproductive struggles that female physicians encounter. The health of physicians themselves are overlooked because they are experts, themselves, towards their patients for family planning, conceiving, and delivering [4].
However, the perceived knowledge and experiences that female physicians have for themselves has not been assessed thoroughly.
Women have become increasingly involved in medicine and consist of more than half the population in medical school [5]. Female physicians have experienced a higher rate of infertility compared to the U.S. average of women in other post-graduate studies. The infertility rate is more than twice as high as 24.1% compared to 10.9% [6]. Female physicians experience impaired fertility because of contributing factors such as lack of support from residency programs and flexible workplace accommodations during pregnancy, for maternity leave, and for childcare support [7]. There are also negative attitudes towards women being pregnant during residency training and stronger stigmas against women in more male dominated specialties [8].
By delaying pregnancy, female physicians are confronted with the difficult decisions to consider using assisted reproductive techniques (ART) such as in vitro fertilization (IVF). Further clarification will be established by investigating the individual experiences and trends of women in male dominated, procedural, non-procedural, and surgical specialties. Our goal is to educate female physicians on the repercussions of delaying childbearing and to encourage training programs to provide support for residents and fellows aiming to conceive, accommodate reasonable maternity leaves and dedicate lactational space for pumping. Therefore, we aim to identify, evaluate, and summarize the findings of studies encompassing the reproductive challenges that U.S. female physicians are met with to bring more awareness towards physician infertility.
METHODS
This study was conducted as a systematic review utilizing PubMed and EMBASE databases. The search terms were: female infertility, lawyer infertility, physician infertility, higher education infertility, and post-graduate infertility.
These keywords were used to search for articles published after 2000 whose full-text were available in English.
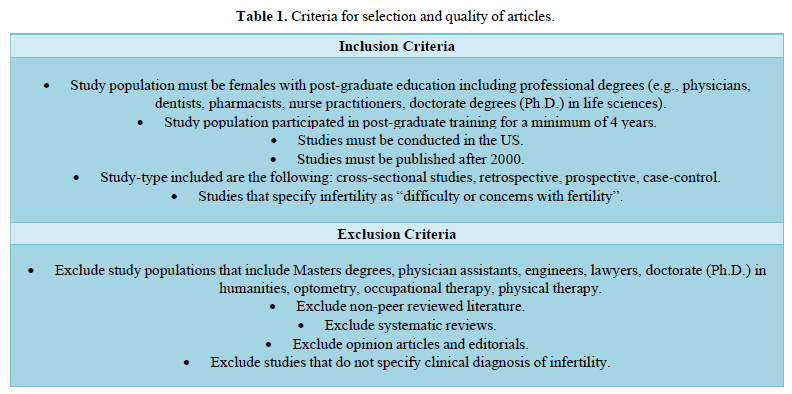
Seven authors independently screened the titles and abstracts. Abstracts from selected articles were carefully screened according to the inclusion criteria listed in Table 1. Articles that contained information about prevalence of infertility, experienced fertility complications and reasons for delaying child bearing among women with post-graduate education was included in the study. The quality of our systematic review was assessed by the AMSTAR checklist [9]. In this study, six articles were accepted for further screening and met all our inclusion criteria. Figure 1 shows article selection sequence. Article selection and elimination is displayed in Table 1.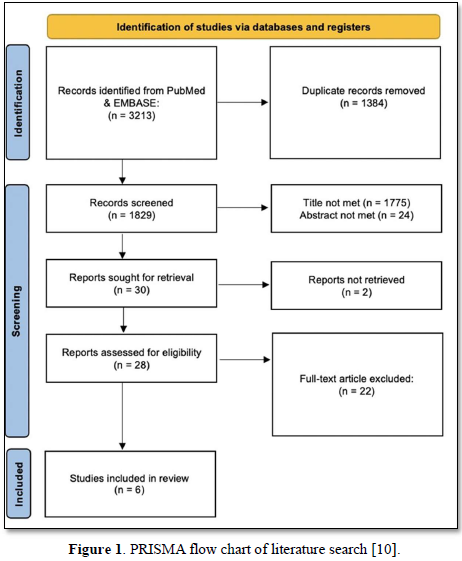
RESULTS
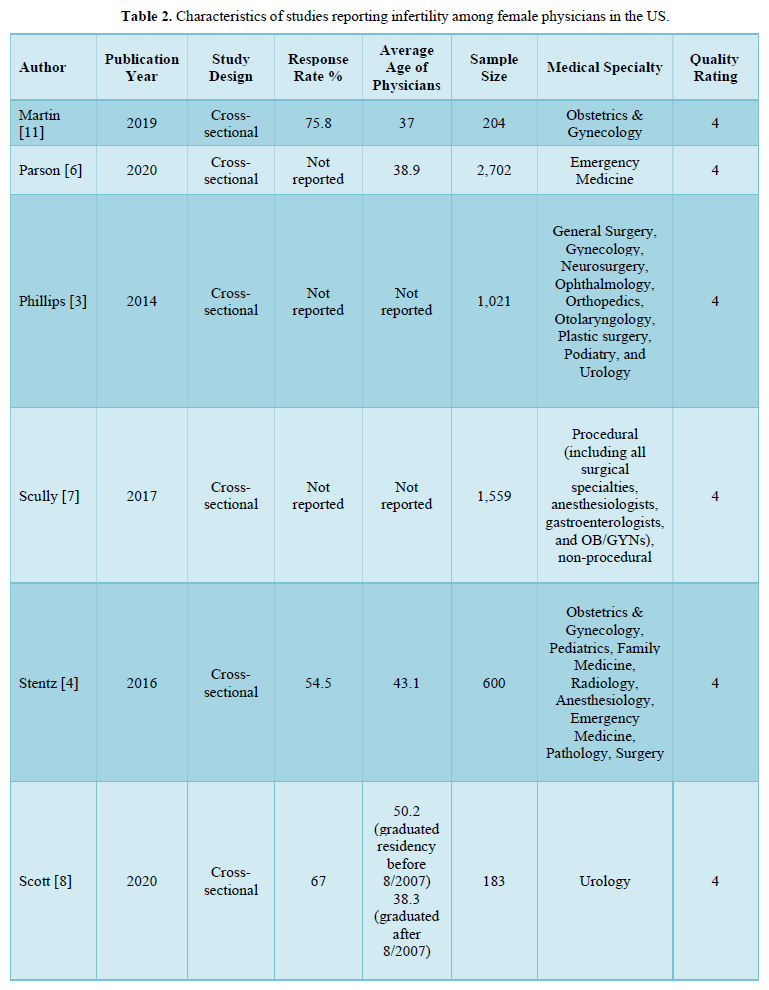
Of the 3,213 articles identified, 1,384 were removed as duplicates, and 1,829 were screened. Of these, 1,799 were excluded based on title and abstract review, and 30 were sought for full-text retrieval, with two reports unable to be acquired. 22 failed to meet inclusion criteria. Ultimately, 6 articles were selected. All 6 studies are cross-sectional studies that surveyed US female physicians in various specialties noted in Table 2.
STUDY AIMS AND DESIGN
All of the studies’ goals were to report problems that female physicians experienced in regards to fertility trends. They assessed characteristics that may affect decisions in delaying childbearing. Two of the studies compared the rate of infertility to the CDC’s National Survey for Family Growth (NSFG). One study compared proceduralists to non-proceduralists and another study compared the experiences of urologists who graduated before 2007 to those who graduated after 2007. Surveys were distributed through email or social media in all of the studies and included items such as demographics, fertility history, pregnancy complications, and attitudes towards work.
STUDY OUTCOMES
Infertility Rates, Causes, and Delayed Childbearing in Female Physicians
From the studies that compared physician infertility to the national average, Phillips [3] and Parsons [6] female physicians have their first pregnancies later and experience more complications. Phillips [3] reported that 32% of 784 female physicians, who attempted to be pregnant had difficulty with fertility. In contrast, only 10.9 % of the U.S. population had difficulty with fertility. In the cases of women who expressed difficulty with fertility, 33% of them had an unexplainable cause [6]. The remaining causes included anovulation, advanced maternal age or premature ovarian failure, polycystic ovarian syndrome (PCOS), endometriosis, recurrent miscarriages, uterine abnormalities, tubal factor, hyperprolactinemia, ovarian cancer, male infertility factor, low progesterone, and becoming pregnant at the time of workup [3]. Similarly, Parsons [6] reported female emergency physicians aged 35-39 had an impaired fertility rate of 28.1% compared to the NSFG rate of 15.2%. Additionally, physicians aged 40-44 also presented with a significant difference in impaired fertility rate of 33.7% to 16.2%. The average age of first pregnancy among female physicians is noted in Table 3.
Stentz [4] reported 24.1% of the participants who tried to conceive were diagnosed with infertility at the average age of 33.7 years. Unfortunately, 21.7% of those physicians were ultimately unable to conceive. The causes of diagnosed infertility are similar to causes presented in Phillips’ study. 29.3% of infertility cases were due to age or diminished ovarian reserve, 29.3% because of ovulatory dysfunction, and 17.2% to male factor infertility [4]. Even though these physicians did start childbearing at a later age, 43.1% expressed that they were shocked and surprised by their infertility diagnoses [4]. When asked to reflect on if they would make any changes through this fertility process, an overwhelming 56.8% stated that they would not do anything different [4]. However, 28.6% stated that they would have tried to start conceiving at an earlier age. Similarly, Martin et al. reported the average age of childbirth was 30.7 years for OBGYNs [11]. For those who had been diagnosed with infertility, the causes were similar to those of other studies [11]. 73% of the participants stated that they intentionally delayed childbearing and 65% stated it was due to their career [11].
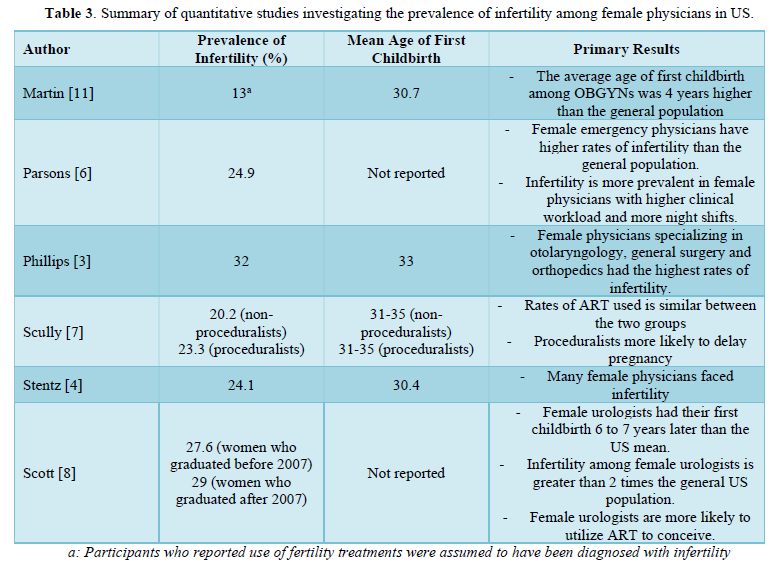
ART Use Among Female Physicians
Types of assisted reproductive technology (ART) used were discussed in three studies: Phillips [3], Scully [7], and Martin [11], Phillips [3] reported female surgeons use ART more than the U.S. general population [3]. Of the 784 women who reported attempting to achieve pregnancy, 84% underwent formal fertility workup [3]. 32% reported having difficulty with fertility [3]. Of that 32%, 76% used ART. The most commonly used types of ART were clomiphene (25%) and IVF (21.6%) [3]. Other techniques used included a combination of intracytoplasmic sperm injection (ICSI) and intrauterine insemination (IUI), injections and ICSI, injections, clomiphene and IUI, donor egg, donor sperm, or not specified [3]. The study found that overall, 23% of female surgeons use ART while the national average use is 5.2% [3]. Individuals using ART reported an increase in the average age of first pregnancy to 35.4 years [3]. As fertility issues and higher risk of complications increase with age, the study determined that the rate of congenital defects in the cohort was higher than, though similar to, the U.S. average; 4.5% as compared to 3.3% [3]. Although the types of ART used were not specified in Parsons [6] the trend of higher use of ART in female emergency physicians compared to the national average was supported. Female emergency physicians’ usage rate of ART was 15.4% while the U.S. rate was 12% [6]. Scully et al. determined there was no significant difference in the rate of ART used nor the frequency of types of ART used between proceduralists and non-proceduralists. 20.2% of non-proceduralists and 23.3% of proceduralists used ART [7]. Both groups used IVF most commonly, with 39.4% in the non-proceduralist group and 40% in the proceduralist group reporting use [7]. The use of clomiphene or its equivalent was 23.4% and 27.6%, respectively. IUI was used by 21.2% and 19.1% of the individuals in each group respectively [7]. Of the OBGYNs in Martin’s study, 13% reported using at least one fertility treatment: 9% used clomiphene or other controlled ovarian stimulation such as letrozole, or injectable gonadotropins. 6% used IUI, 5% used IVF, 2% used oocyte or embryo freezing, 2% used a donor sperm, and 6% did not specify [11].
Additionally, Martin [11] reported that 68% OBGYNs in Georgia who have not finished childbearing worried about infertility and 29% have considered oocyte or embryo cryopreservation. Similarly, Stentz [4] reported that for the 60% of those who were diagnosed with infertility, 16.7% of them would have used cryopreservation in their fertility experience. For those who did not have children, 17.9% of them reflected that they would have used cryopreservation to extend fertility [4].
Impact of Specialty and Workplace Conditions on Pregnancy/ Infertility
Specialty could be considered as a factor in higher rates of impaired fertility, as 17.1% of participants in Stentz’s study reported that they would consider going into a different specialty when asked about what they would change about their pregnancy experience [4]. Scully [7] determined that proceduralists were more likely than non-proceduralists to delay pregnancy. There was no significant difference determined in reported time to conception or pregnancy-related complications among proceduralists and on-proceduralists [7]. There was also no difference in the amount of missed work due to pregnancy complications that did not include maternity leave [7].
Workplace attitudes and accommodations during pregnancy during residency affect the decision of delaying childbearing and are contributing factors to these physicians' worries. It was reported in Martin’s study that only 35% of the participants who delivered during residency were able to exclusively breastfeed for more than 6 months [11]. Residents also experienced more postpartum depression than non-residents, 26% compared to 16%. More residents also had less than 6 weeks of maternity leave than non-residents, 53% compared to 29% [11]. In Parsons’ study, female emergency physicians also stated that their career and workload was a large factor in delaying childbearing. Of these physicians, those who reported impaired fertility worked on average 9.8 more hours per month and had 4.5 more-night shifts per month than those who did not report impaired fertility [6]. Scott [8] compared infertility rates between female urologists who graduated residency before and after 2007, which were 27.6% and 29% respectively. In 23% of all pregnancies at least one complication was reported [8]. Although 76% of both groups of female urologists noted that they were holistically satisfied with their pregnancy experience, it is important to note that the study found that overall satisfaction with pregnancy experience was not correlated to average hours worked nor the average number of days per week on call, nor was it associated with the physician’s stage in training [8]. Only 48% of both groups of urologists were satisfied with maternity leave duration, which was reported as being less than 7 weeks for 70% of participants [8]. 71% of female urologists who graduated before 2007 and 68% of those who graduated after expressed that their career highly affected and took over their personal lives [8].
DISCUSSION
There is an unprecedented level of physician burnout across multiple medical specialties [12]. Given the demands of medical training, many American female physicians face barriers regarding family planning and fertility, and 68% have concerns about infertility [11].
Infertility and ART use trends among female physicians
All six studies included in this review reported higher incidences of infertility among American female physicians. Emergency medicine physicians ages 35-44 had significant increases in impaired fecundity compared to the NSFG general population [6]. The average age of the first childbirth among female physicians was higher than that of the general US population: OBGYNs 4 years later, female surgeons later in life, and American female physicians 7.4 years later [3,4,11]. Proceduralists were slightly older at the time of their first pregnancy in comparison to non-proceduralists [7]. The pattern of female physicians having children at a later age and having impaired fertility persists even in studies that did not compare statistics to the national average. As the average age of graduation from medical school is 27.5 years and from residency is 31.6 years, it is expected that childbearing is delayed. The average age for first attempt of conception for these physicians was 30.6 years [4].
An increase in the use of ART was also found among urologists [13]. Surgeons were found to have fewer children (1.4 vs 2.6 children), higher incidence of infertility and higher use of ART (17% vs. 5.2%) when compared to the general US population [3,7]. Possible reasons for higher use of ART among surgeons are higher socioeconomic status, contacts with high-risk obstetricians and reproductive specialists, and better access to hospital treatment in comparison to other industries [14]. In addition, 34 years was the average age at the time of oocyte/embryo cryopreservation [11]. Stentz [4] reports 7% of female physicians wished they used ART. It can be postulated that female physicians starting families at later ages will lead to more widespread use of cryopreservation in the future.
Factors that contribute to infertility among female physicians
Career or education was the main reason for delaying childbirth among female physicians [8]. 73% of OBGYN physicians purposely delayed pregnancy due to educational, career, or financial reasons [11]. There are perceived threats to their careers and female resident physicians were less likely to marry and have children than their male counterparts [3,15]. Other studies have reported this population wanting to have children after the age of 30 [16]. Physical and psychological stress can affect pregnancy rates. Barzilai-Pesach and colleagues reported those who perceived their job as more demanding were less likely to conceive [17]. Further, pregnant physicians, mainly resident physicians, have higher workload and longer work hours, leading to physical and emotional stressors [3]. One proposed mechanism of infertility is a stress-exerted effect on the sympathetic medullary pathway leading to a reduction in conception probability [18].
One study reported an association between the number of night shifts and impaired fecundity. Female emergency medicine physicians who worked 11% more total clinical hours per month and 13% more-night clinical hours reported more occurrences of infertility. The proposed causal mechanism is that night shifts affect circadian rhythms which also alter hormonal concentrations and decrease oocyte maturation [6]. Further, minimizing variations in shift work may decrease the impact on female fertility.
Pregnancy complications in female physicians
Pregnancy complications among female physicians is multifactorial. Intentional delays in pregnancy increase age at time of conception as well as incidences of miscarriage and other adverse pregnancy outcomes. Reported pregnancy complications were significantly higher in proceduralists (82%) with some requiring bed rest postpartum [7]. 23% of female urologists and 30% of surgeons reported adverse pregnancy events [8,19]. The demands of residency training can conflict with the physical and psychological needs of pregnant women and increase the risk for complications (i.e., stressful work, excessive standing during the day, physically demanding work and night shifts [20,21]. Pregnancy complications such as preterm labor, gestational hypertension, placental abruption, intrauterine growth restriction, and preeclampsia were reported among female physicians, with preterm labor and preeclampsia being more prevalent in this population than the general US population [22,23]. Advanced maternal age is likely to contribute to these higher rates of pregnancy complications among female physicians.
It is possible that resident schedules and program cultures can contribute to higher depression rates, which has been linked to poor patient outcomes [24]. Programs can consider improving work environments that minimize risks to reproductive health.
Infertility education and maternity leave among female resident physicians
Approximately ⅓ of OBGYN trainees overestimated the age of fertility declination, nonfertility specialists are not aware of the rapid fertility declination, and many residents do not understand the limitations of ART and overestimate its success [4,25]. It is essential for women at all stages in their medical training to be aware of the risks of infertility. Educating female medical trainees about childbearing challenges and infertility early in their medical career can encourage more informed family planning.
Additionally, options for maternity leave vary by residency program and have changed over time, with some requiring extension of residency training. New resident mothers were more likely to take less than 6 weeks maternity leave compared to nonresident mothers [11]. Most female urologists were not satisfied with the duration of their maternity leave and those who took more than 8 weeks off reported a more positive experience [8].
Residents may have to pick up additional call shifts, have “make-up time,” or extend training post maternity leave [25,26]. Because of this, residents may choose to take shorter leaves to avoid missing cases or learning opportunities. Longer maternity leaves are associated with decreased infant morbidity, mortality, and overall better maternal mental health [27]. The implementation of new policies that allow more schedule flexibility has the potential to allow women to more effectively heal postpartum and care for their newborns.
Current state of parental leave in residency programs
Stigma surrounding pregnancy and maternity persists in medicine [28]. Significant concerns about workplace support of pregnancy during training have been reported among female physicians [4]. Residency programs are restricted in the parental leaves that can be offered to trainees due to required adherence of board and institutional policies in place to ensure adequate residency training. In the absence of policies surrounding leave and coverage, there is a necessity of relying on partners that can cause additional stress outside of work life. It is important that policies are established to promote resident wellness and support without placing burdens on other colleagues. These policies could alleviate the guilt pregnant physicians experience for taking leave to care for their newborns, as well as avoid any discontent harbored by colleagues who cover their shifts. One possible solution would be increasing shifts of fellows or mid-level practitioners or hiring temporary staff. Though conflicts among colleagues in regards to co-physicians’ pregnancies have improved since initial policies, it is important that we continue to provide support in an already underserved profession with a growing and aging population [29]. Scott and colleagues reported that none of the American Board of Medical Specialties organizations have a maternity or parenting leave policy [8]. However, full salary for pregnancy leave was on average 8.6 weeks for faculty members among 12 of the reviewed medical schools [30]. Many residency programs allow an average of 6 weeks leave in 1 year for any need [31]. To facilitate maternal and paternal leaves, another possible solution is alternative training schedules to address coverage issues.
Potential postponement of menopause
With the depletion of ovarian reserves beginning at 35 years of age, female physicians may be able to postpone menopause through ovarian cryopreservation [32-34]. 29% of OBGYNs have considered cryopreservation, with the average age of the participant at the time oocyte cryopreservation being 34 years of age [11]. Many female physicians wished they had used cryopreservation earlier in their medical training career [4]. Ovarian tissue cryopreservation may be an option for young female physicians to extend their fertility [34]. However, this solution has an associated high cost of not only the procedure but also the subsequent monthly cryopreservation storage costs of the harvested oocytes/embryos. With the growing costs associated with attending and completing medical school leaving many U.S. physicians in debt, as well as the minimum-wage pay they receive during residency, use of cryopreservation may further exacerbate financial hardships for female physicians. Financial support for the use of ART, such as cryopreservation, provided by training programs can be beneficial for female physicians looking to preserve their fertility as well as to programs who are unable or unwilling to provide comprehensive maternity leave to their female residents.
CONCLUSION
It is evident that infertility, use of ART, and pregnancy complications are more prevalent among American female physicians than the general population due to multiple factors (i.e., stress, work load, advanced age). Pregnancy, childbirth, and work-life balance are major issues among female physicians that require additional and continuous support from the profession. Creating sustainable and flexible workplace policies for parental leave, and recognizing the personal significance and reward of childbearing, within the physician medical culture can reduce guilt and anxiety experienced by female physicians and reduce tension among all resident colleagues. These modifications will promote a healthier, more sustainable, and more productive medical team.
- Sobotka T (2006) In pursuit of higher education, do we postpone parenthood too long? Gend Med 3: 183-
- Diamond P (1984) The private lives of women Medica 2: 40-45.
- Phillips EA, Nimeh T, Braga J, Lerner LB (2014) Does a Surgical Career Affect a Woman's Childbearing and Fertility? A Report on Pregnancy and Fertility Trends among Female Surgeons. J Am Coll Surg 219: 944-950.
- Stentz NC, Griffith KA, Perkins E, DeCastro JR, Jagsi R (2016) Fertility and Childbearing Among American Female Physicians. J Womens Health (Larchmt) 25(10): 1059-1065.
- Boyle P (2019) More women than men are enrolled in medical school. Association of American Medical
- Parsons M, Kalynych C, Johns TL, Scicchitano MJ, Lott M, et al. (2020) IMPACT survey: IMpaired fecundity in Physicians and Association with Clinical Time. J Am Coll Emerg Physicians Open 1(5): 1023-1029.
- Scully RE, Stagg, Amy R, Melnitchouk, Nelya, Davids, Jennifer S (2017) Pregnancy outcomes in female physicians in procedural versus non-procedural specialties. The American Journal of Surgery 214:599-603
- Scott VCS, Lerner LB, Eilber KS, Anger JT, Ackerman AL (2020) Re‐evaluation of birth trends and pregnancy complications among female urologists: Have we made any progress? Neurourol Urodyn 39: 1355-1362.
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, et al. (2017) AMSTAR 2: A critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both. BMJ 358: j4008.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et (2021) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372: n71.
- Martin CE, Hipp HS, Kottke M, Haddad LB, Kawwass JF (2019) Fertility, Pregnancy, and Postpartum: A Survey of Practicing Georgia Obstetrician Gynecologists. Maternal and Child Health Journa
- Pulcrano M, Evans SR, Sosin M (2016) Quality of life and burnout rates across surgical specialties: Asystematic JAMA Surg 151: 970-978.
- Lerner LB, Stolzmann KL, Gulla VD (2009) Birth trends and pregnancy complications among women J Am Coll Surg 208: 293e-297e.
- Feveile H, Schmidt L, Hannerz H, Hougaard KS (2011) Industrial differences in female fertility treatment rates--a new approach to assess differences related to occupation? Scand J Public Health 39: 164-171.
- Willett LL, Wellons MF, Hartig JR, Roenigk L, Panda M, et (2010) Do women residents delay childbearing due to perceived career threats? Acad Med 85: 640e-646e.
- Dunson DB, Colombo B, Baird DD (2002) Changes with age in the level and duration of fertility in the menstrual cycle. Hum Reprod 17: 1399-1403.
- Barzilai-Pesach V, Sheiner EK, Sheiner E, Potashnik G, Shoham-Vardi I (2006) The effect of women’s occupational psychologic stress on outcome of fertility treatments. J Occup Environ Med 48: 56e-62e.
- Louis GM, Lum KJ, Sundaram R, Chen Z, Kim S, et a (2011) Stress reduces conception probabilities across the fertile window: Evidence in support of relaxation. Fertil Steril 95: 2184e-2189e.
- Hamilton AR, Tyson MD, Braga JA, Lerner LB (2012) Childbearing and pregnancy characteristics of female orthopedic surgeons. J Bone Joint Surg Am 94: e77.
- Luke B, Avni M, Wolf FM (2000) Working conditions and adverse pregnancy outcome: A meta‐analysis. Obstet Gynecol 95: 623-635.
- Bonzini M, Coggon D, Palmer KT (2007) Risk of prematurity, low birthweight and pre‐eclampsia in relation to working hours and physical activities: A systematic Occup Environ Med 64: 228-243.
- Klebanoff MA, Shiono PH, Rhoads GG (1990) Outcomes of Pregnancy in a National Sample of Resident Physicians. N Engl J Med 323: 1040-1045.
- Grunebaum A, Minkoff H, Blake D (1987) Pregnancy among obstetricians: a comparison of births before, during, and after Am J Obstet Gynecol 157: 79-83.
- Mata DA, Ramos MA, Bansal N, Khan R, Guille C, et al. (2015) Prevalence of depression and depressive symptoms among resident physicians: A systematic review and meta-analysis. JAMA 314: 2373-2383.
- Davis JL, Baillie S, Hodgson CS, Vontver L, Platt LD (2001) Maternity leave: Existing policies in obstetrics and gynecology residency programs. Obstet Gynecol 98: 1093-1098.
- Gabbe SG, Morgan MA, Power ML, Schulkin J, Williams SB (2003) Duty hours and pregnancy outcome among residents in obstetrics and gynecology. Obstet Gynecol 102: 948-951.
- Van Niel MS, Bhatia R, Riano NS, de Faria L, Catapano-Friedman L, et al. (2020) The impact of paid maternity leave on the mental and physical health of mothers and children: A review of the literature and policy implications. Harv Rev Psychiatry 28: 113-126.
- Turner PL, Lumpkins K, Gabre J, Lin MJ, Liu X, et al. (2012) Pregnancy Among Women Surgeons: Trends Over Time. Arch Surg 147: 474-479.
- Franco K, Tamburrino M, Campbell N, Evans C, Jurs S (1994) Conflict with physician pregnancy Acad Psychiatry 18: 146-153.
- Riano NS, Linos E, Accurso EC, Sung D, Linos E, et al. (2018) Paid family and childbearing leave policies at top US medical schools. JAMA 319: 611-614.
- Varda BK, Glover M (2018) Specialty board leave policies for resident physicians requesting parental JAMA 320: 2374-2377.
- Hegazy AA (2020) Potentiality of postponing menopause through ovarian auto-graft transplantation. J Gynecol Reprod Med 4: 29-31.
- Hegazy AA (2020) Is There any Mean to Postpone the Menopausal Ovarian Senescence? Int J Fertil Steril 13: 346.
- Hegazy AA (2021) Postponing Menopause and Lengthening Fertile Age for Women’s Good Health: A Potential Hope. World J Gynecol Womens Health 5: 1-2.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)



