Case Report
A Rare Serous Papillary Cystadenofibroma of the Fallopian Tube
3988
Views & Citations2988
Likes & Shares
Tumors of the fallopian tube consist an uncommon and rare entity of the female genital tract. The benign tumors of the fallopian tube are endometrioid polyp, metaplastic papillary tumor, cystadenofibroma, adenofibroma, cystadenoma and papilloma, according to the classification held by the World Health Organization (WHO). It is essential we report that the great majority of women with these tumors are asymptomatic and these tumors are mostly diagnosed incidentally during a gynecological examination or a pelvic ultrasound scan or during an operation for other surgical reasons.
INTRODUCTION
Serous papillary cystadenofibroma is an extremely rare benign tumor of the fallopian tube. Until now, only 19 cases in the world literature have been described [1-5] The focus of this paper is a case study concerning a 37-year-old woman with pelvic pain, whose gynecological examination revealed a pelvic tumor confirmed with transvaginal ultrasound and further assessed with magnetic resonance imaging. At that point the differential diagnosis included para-ovarian tumor or a GIST tumor and subsequently was scheduled for surgical management. A histopathological exam revealed a serous papillary cystadenofibroma of the fallopian tube.
CASE REPORT
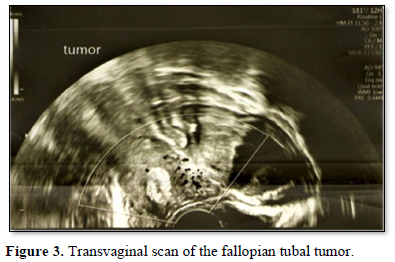
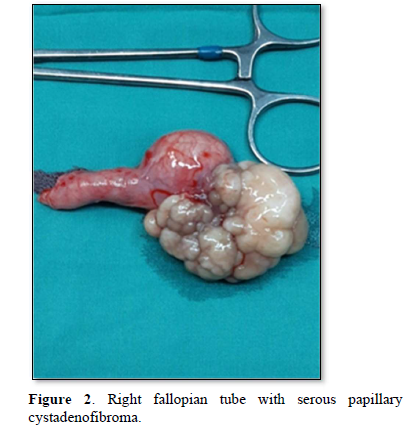
A 37-year-old Caucasian female, presented to the Outpatient Clinic complaining of intermittent pelvic pain, located on the right iliac fossa and radiating to the right abdomen and lumbar area. It occurred every other month for a year, with no alleviation of the symptoms, which lasted 24 h despite positioning or the use of common analgesics. Her menstrual history was regular and she had two full-term caesarian deliveries with the last childbirth 2 years ago. Speculum examination did not demonstrate any vaginal discharge and bimanual examination revealed a small mass arising from the pelvis. The cervix was not sensitive on her bimanual examination, while there was discomfort in the right adnexa. The transvaginal ultrasound demonstrated a mass arising from the right adnexa having a size of 5.3cm x 2.2cm. The uterus and the left adnexa have no pathology at the moment. There was no free fluid in the pouch of Douglas. Magnetic resonance imaging showed a small oval structure of mixed magnetic signal comprising both of cystic and compact areas, but also islets of fat with a size of 4,5 cm x 6cm, which required differential diagnosis between a para-ovarian tumor and a stromal GIST tumor.
Patient’s surgical history included a right ovarian cystectomy 3 years ago. Hypothyroidism treated with T4 100μg and a mild Von Willebrand's deficiency was reported from the patient, but not requiring any further treatment at the time.
The blood test exams were normal and the tumor markers were: cancer antigen - 125 = 7.6 u/ml (normal 0-35 u/ml), lactate dehydrogenase = 155 u/l (normal 135-214 u/l), carcinoembryonic antigen = 0.69 ng/ml (normal 0-5 ng/ml), cancer antigen - 19.9 = 23.1 u/l (normal < 37 u/l), and alpha-feto protein = 2.3 ng/ml (normal 0-6 ng/ml).
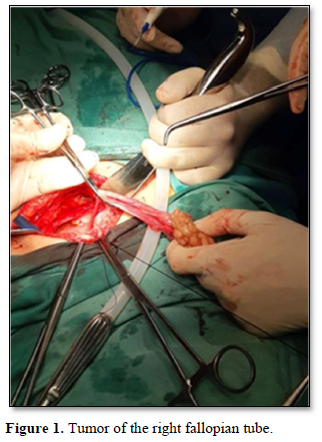
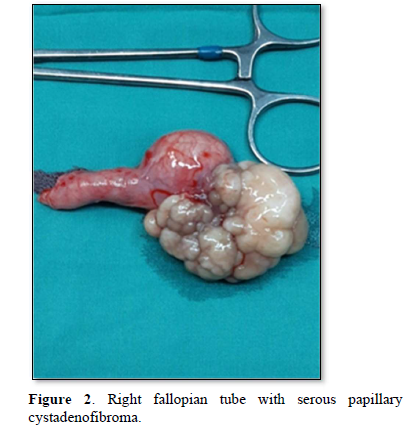
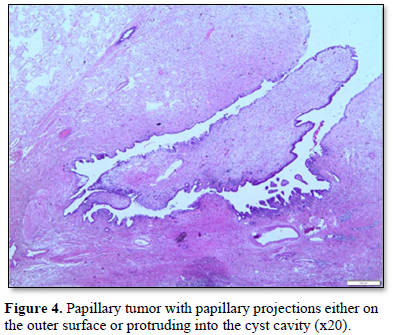
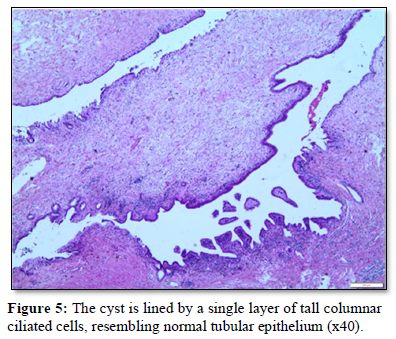
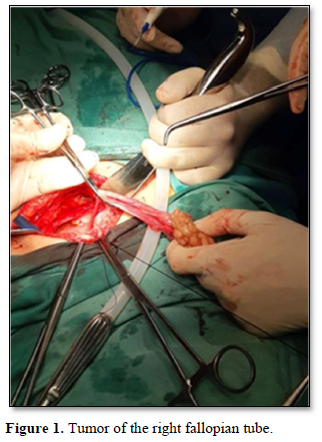
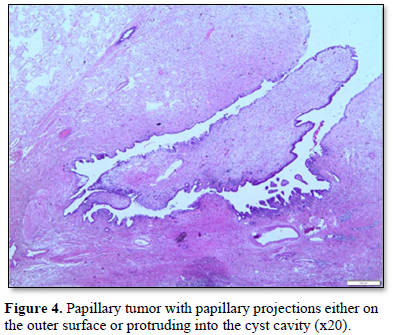
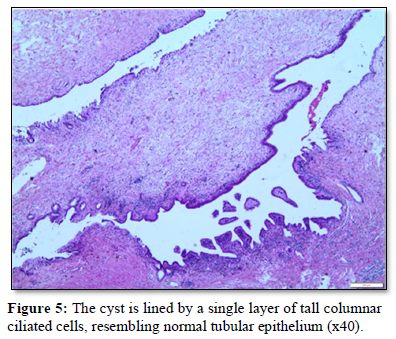
She was scheduled for admission to the hospital. A decision for an exploratory laparotomy was made. Intraoperative findings revealed a firm tumor with a cauliflower-like surface arising from the right fallopian tube (Figure 1). The right ovary was found completely separate from the tumor. A right tubal cystectomy was performed (Figure 1) and a cold biopsy, consisting of the fallopian tube and the mass, was sent for further evaluation. The results were negative for malignancy. Furthermore, the complete histological analysis revealed a serous papillary cystadenofibroma (SPACF) with collagenization of the substrate, which was in contact with a simple epidermoid cyst (mature cystic teratoma). Postoperatively, the patient’s recovery was without incident and she was thereafter discharged within four days [6].
DISCUSSION
The differential diagnosis for a tumor of tubal origin includes tubal carcinoma (primary or metastatic), serous tumor of low malignant potential (STLMP) and borderline papillary serous tumor of the fallopian tube. Malignant neoplasms of the fallopian tube are rare, accounting for 0.18% to 1.6% of all malignant neoplasms of the female reproductive tract. They most commonly appear in post-menopausal women, usually in the sixth decade of life. However, histological, molecular and genetic evidence seems to indicate that these rates are underestimated, because as well as over 40-60% of high grade serous ovarian carcinomas appear to originate from the Fallopian tubes. These findings, once confirmed in larger studies, will have a decisive impact on prevention, early diagnosis and treatment of malignant tumors of the female genital track. Serous papillary cystadenofibromas of the fallopian tube are rare tumors with a faint possibility for malignant development [7].
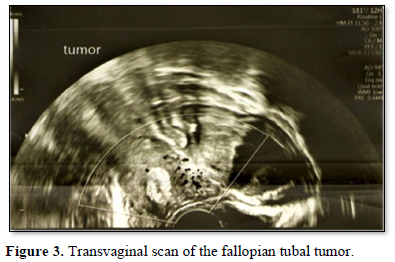
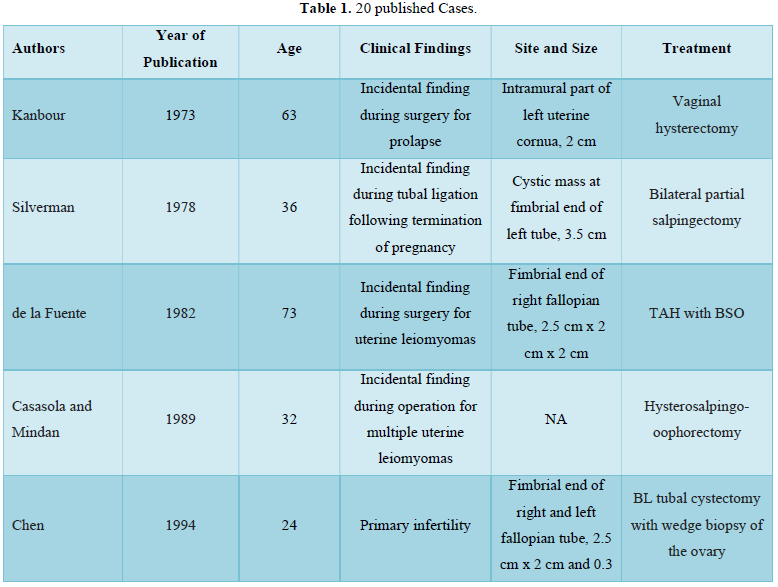
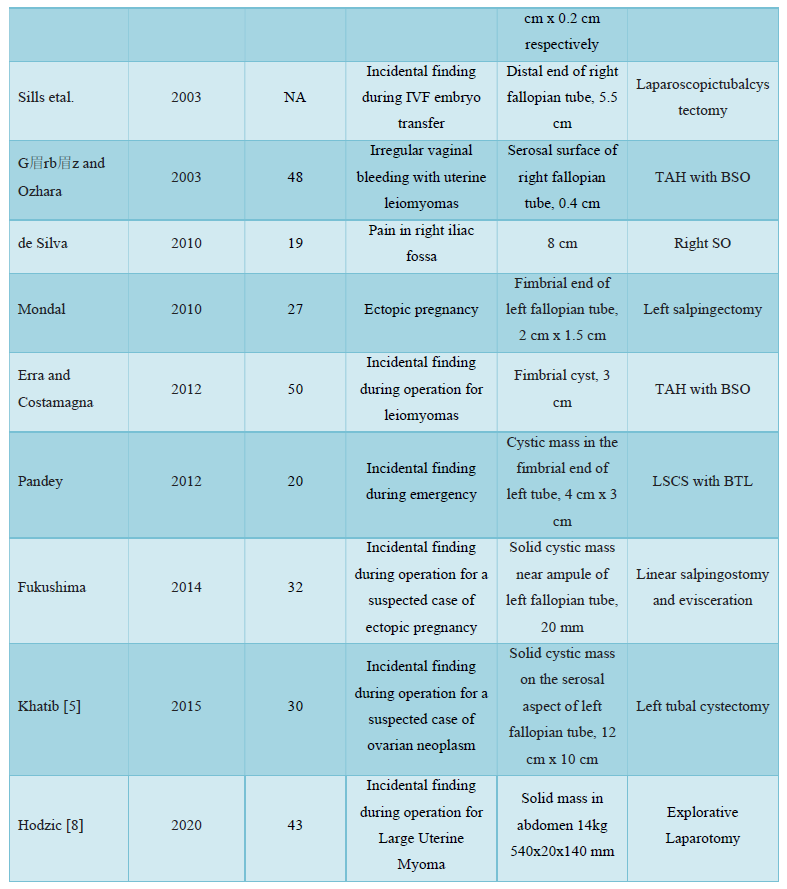
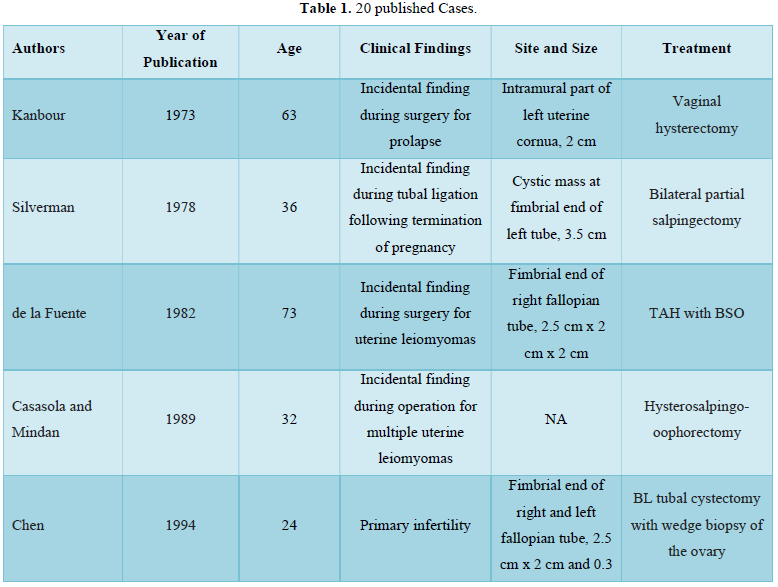
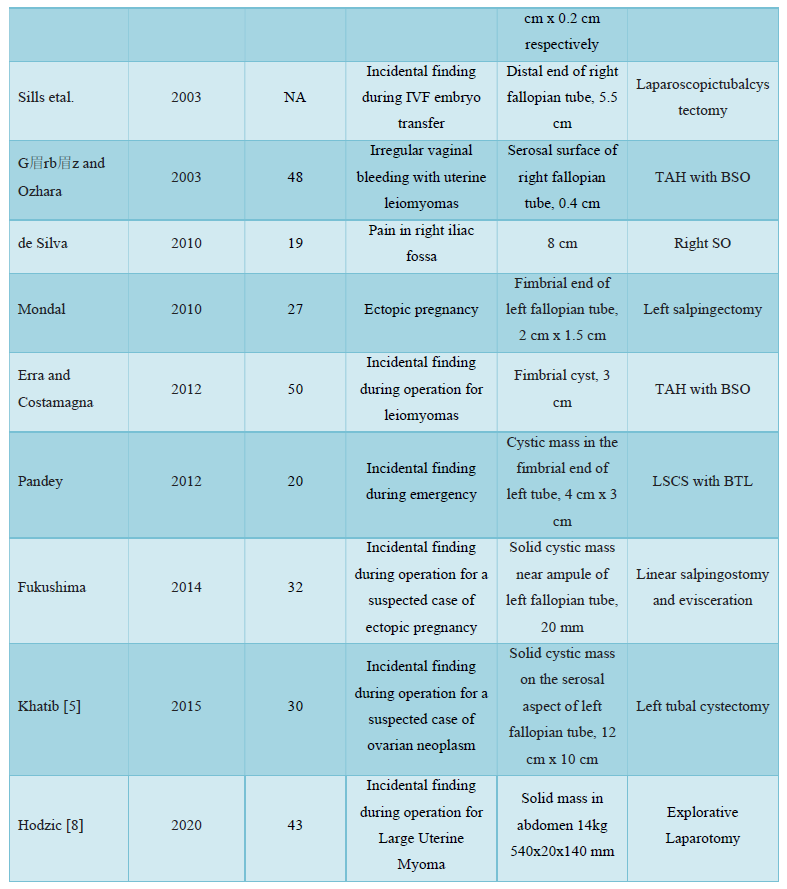
The tumor is considered an embryologic remnant rather than a proliferating neoplastic process. Only a few cases have been reported in world literature. The age of presentation showed a wide range from 19 to 73 years. Mean age reported is 49 years and clinical presentation was variable including extreme diversity in size. Most are present at the fimbrial end. They are usually small in size and measure about 0.5-3 cm in diameter, cystic with coarse papillary excrescences as seen in the present case. Histologically, two components are present, a connective tissue stroma without nuclear pleomorphism or mitosis and papillary structures or tubal structures lined by epithelial cells. The epithelial cell type has been serous in most cases but occasionally may be endometrioid. The tumor seems to have a benign course and most are seen in postmenopausal women. Microscopy shows cellular pleomorphism with nuclear atypia. STLMP and borderline tumors show stratification with nuclear atypia. Hence, histology is necessary to confirm the diagnosis. Also, cystadenofibromas can be one of the causes of infertility in reproductive-aged women. In most cases, the recommended treatment is a unilateral salpingectomy/cystectomy, without the need for any further treatment. However, long-term follow-up of more cases is required to draw more definitive conclusions and consultations from the clinicians. Table 1 describes the previous 20 published worldwide cases. It is modified from the one published by Hodzic [8].
CONCLUSION
In conclusion, serous papillary cystadenofibroma is a rare entity, usually small in size presented as adnexal tumor incidentally found in ultrasound examination. It is difficult to make the differential diagnosis based on ultrasound findings. Other imaging modalities such as CT or MRI of lower abdomen are not usually conclusive and clinicians must always be aware of this condition. The prognosis is excellent and the treatment of choice is surgical, including either removal of the lesion with or without the fallopian tube or salpingoophorectomy depending on the patient’s age and desire of preserving fertility.
- Alvarado-Cabrero I, Cheung A, Caduff R (2003) Tumors of the fallopian tube. In: world health organization classification of tumors: Tumors of the breast and female genital organs. Lyon, France. pp: 206-211
- de la Fuente AA (1982) Benign mixed Müllerian tumor-adenofibroma of the fallopian tube. Histopathology 6: 661-666.
- Gürbüz Y, Ozkara SK (2003) Immunohistochemical profile of serous papillary cystadenofibroma of the fallopian tube: A clue of paramesonephric origin. Appl Immunohistochem Mol Morphol 11: 153-155.
- Erra S, Costamagna D (2012) Serous cystadenofibroma of the fallopian tube: case report and literature review. G Chir 33: 31-33.
- Khatib Y, Patel RD, Kashikar AS, Chavan K (2015) Serous papillary cystadenofibroma of the fallopian tube: A case report and short review of literature. Indian J Pathol Microbiol 58: 524-527.
- de Silva TS, Patil A, Lawrence RN (2010) Acute presentation of a benign cystadenofibroma of the fallopian tube: A case report. J Med Case Rep 4: 181.
- Chen KT (1981) Bilateral papillary adenofibroma of the fallopian tube. Am J Clin Pathol 75: 229-231.
- Hodzic E, Pusina S, Bajramagic S, Salibasic M, Holjan S (2020) Papillary Cystadenofibroma of Fallopian Tube: Case Report with a Literature Review. Med Arch 74: 73-76.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Chemotherapy Research Journal (ISSN:2642-0236)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Allergy Research (ISSN:2642-326X)
- International Journal of Diabetes (ISSN: 2644-3031)







