Case Report
Spontaneous Regression of Adenocarcinoma in Situ of the Uterine Cervix During Pregnancy, Initially Diagnosed Invasive Adenocarcinoma
965
Views & Citations10
Likes & Shares
Cervical adenocarcinoma represents 20% of all invasive carcinomas, the most common is epidermoid or squamous cell, adenocarcinoma in situ is less frequent and represents 2% of CIN3 lesions, high-grade intra-epithelial lesions, ages from 29 to 46 years. Among pregnant women, there is no published data on the frequency and isolated cases are reported. Among patients with any type of cervical cancer 1-3% were pregnant at the time of diagnosis. Recommendation of the International Federation of Gynecology and Obstetrics / TNM in reference to treatment in pT1a1G1 stage should be conservative conization using a diathermic loop, cold scalpel or laser. No publication or report on involution of adenocarcinoma in situ in the cervix was detected, whether or not it was associated with pregnancy.
Keywords: Endocervical Adenocarcinoma, Carcinoma in situ endocervix, Regression of adenocarcinoma
INTRODUCTION
Cervical adenocarcinoma represents 20% of all invasive carcinomas, the most common is epidermoid or squamous cell [1], adenocarcinoma in situ is less frequent and represents 2% of CIN3 lesions, high-grade intra-epithelial lesions, ages from 29 to 46 years [1]. Among pregnant women, there is no published data on the frequency and isolated cases are reported [2]. Among patients with any type of cervical cancer 1-3% were pregnant at the time of diagnosis [3]. Recommendation of the International Federation of Gynecology and Obstetrics / TNM in reference to treatment in pT1a1G1 stage should be conservative conization using a diathermic loop, cold scalpel or laser [2-4]. No publication or report on involution of adenocarcinoma in situ in the cervix was detected, whether or not it was associated with pregnancy.
CASE REPORT
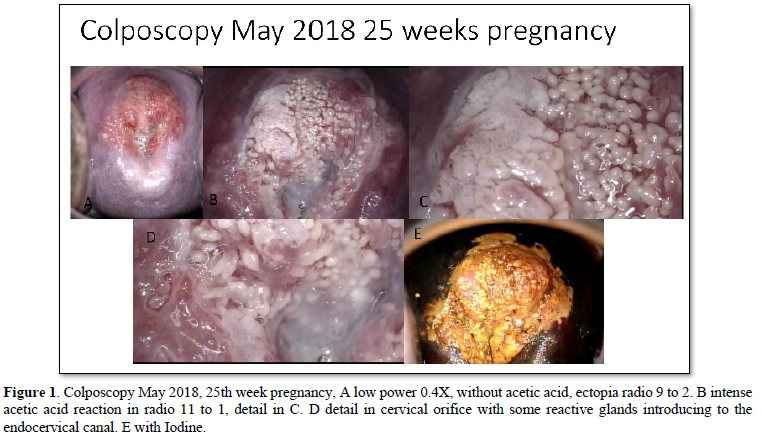
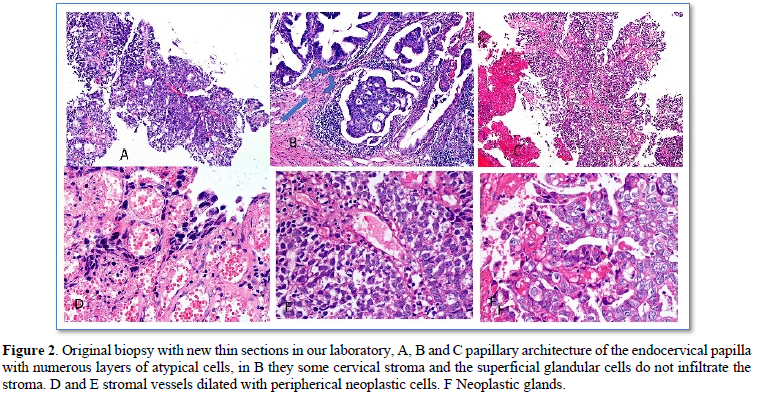
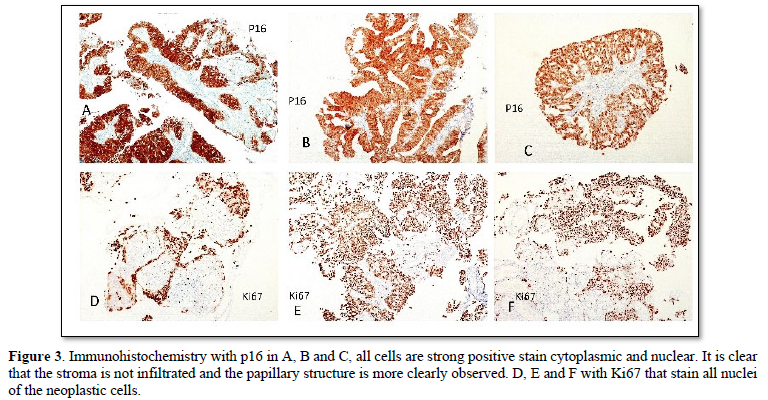
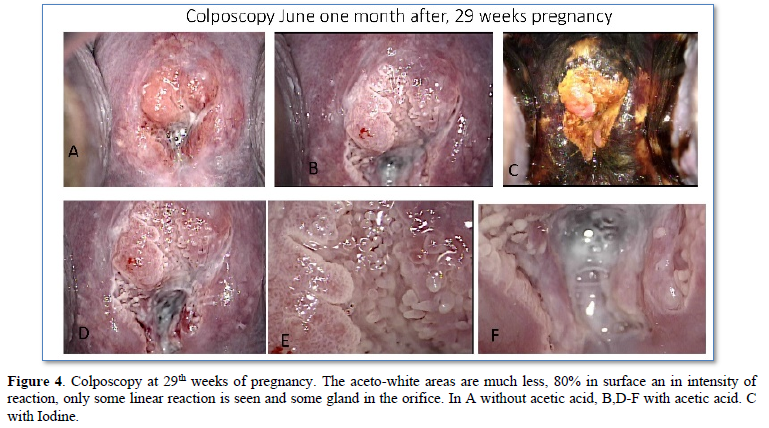
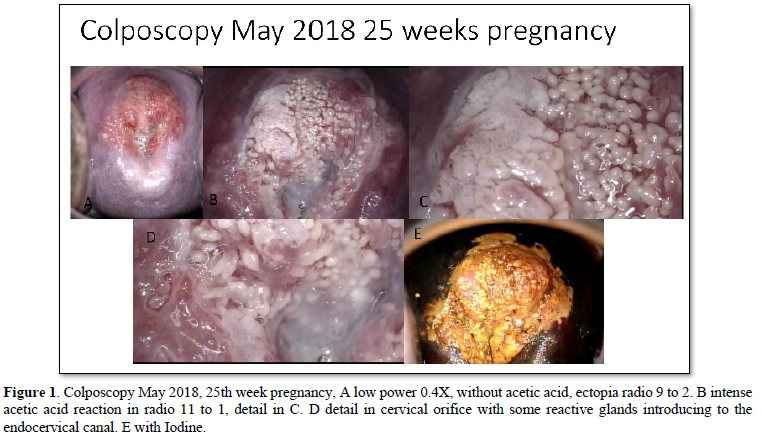
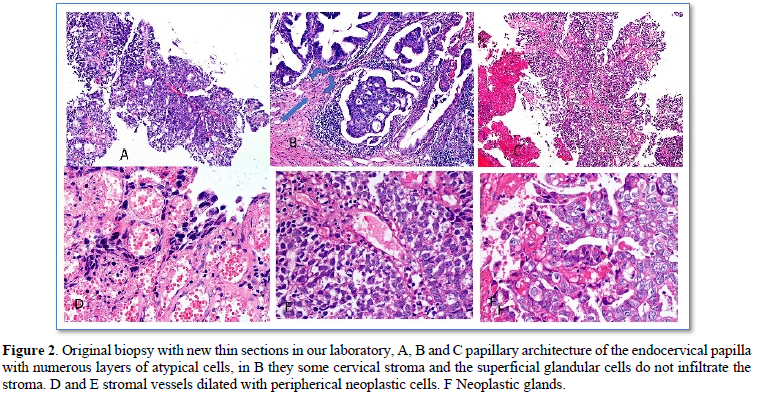
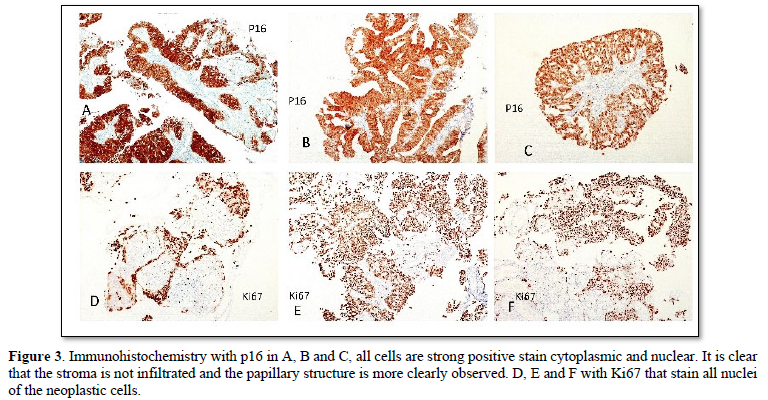
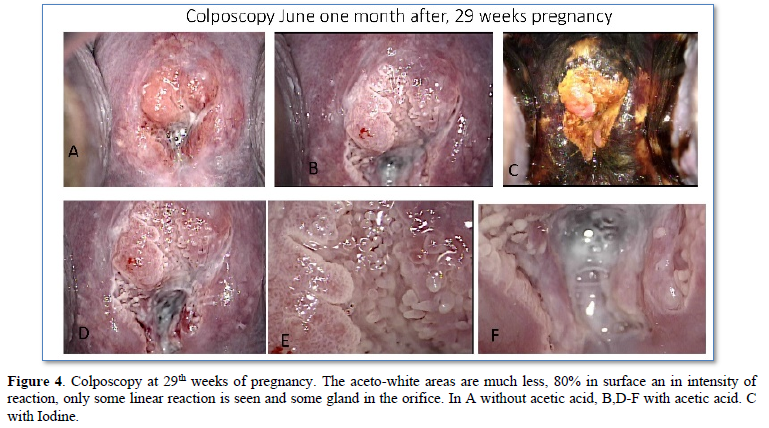
A 36-year-old woman with no significant history, G1, C1, who presented significant trans-vaginal bleeding in 22nd pregnancy week (March 2018), went to the gynecological specialty hospital “Gineco 4” of the IMSS in Mexico City, they found transvaginal bleeding and hemostasis was performed without success, so the patient went to a private hospital, in the cervical exploration a polypoid lesion protruding through the cervical os with significant active bleeding was found (Figure 1), hemostatic biopsy was taken which was diagnosed as invasive adenocarcinoma. A few days later, he went again to the specialty hospital “Gineco 4” of the IMSS for treatment and review of the case and the biopsy taken in the private hospital, corroborating the diagnosis of invasive adenocarcinoma. Pregnancy ending at 27 weeks was proposed by cesarean section and total hysterectomy with salpingo-oophorectomy. She was referred for a third opinion to our laboratory for colposcopy and review of the previous biopsy at 25th week of pregnancy (May 2018) (Figure 2). The new review of the biopsy with immunohistochemistry with p16 and ki67 showed exclusively adenocarcinoma in situ, without invasion and without squamous component (Figures 3 & 4). PCR detected HPV 18 type. With the new diagnosis to only in situ, without invasion, the treatment initially proposed was reconsidered and a new colposcopy was suggested in one month, on the 29th week of gestation, June 2018. In this new colposcopy the lesion had much less aceto white reactive areas, both in extension as in reactivity, only cytology was taken to avoid possible bleeding. The result showed mild atypia and fewer atypical cells. With the findings, it was proposed to wait until week 36 and a cesarean section was performed on July 31, 2018, with a cervical biopsy taken at that time, with a diagnosis of chronic cervicitis without evidence of neoplasia. She was reviewed again 3 months after the cesarean section, October 2018, where the colposcopy showed no lesion. The patient decided together with her oncologist to perform hysterectomy with unilateral oophorectomy on December 2018. The specimen was thoroughly reviewed in two independent pathology laboratories including the entire cervix and showed no residual neoplasia in the endocervix, exocervix.
DISCUSSION
Adenocarcinoma in situ is well defined cytologically and histologically as well as the invasion criteria and is considered to be the precursor of invasive adenocarcinoma and mostly associated with HPV type 18 [5-7]. The progression from in situ to invasive lesions is not well described since almost all of these lesions are not observed but treated so that it is not known how many of them progress to invasive lesion. In the literature reviewed in the ALTS study [8] refer involution of 60 and 33% in low and high-grade squamous lesions respectively, there is no reported data of involution in glandular lesions. Adenocarcinoma in situ lesions is associated to squamous lesion in 50% [8], which was not seen in this case. The use of p16 and Ki67 [8] are used to confirm a high-grade lesion and p16 is an indirect but very reliable evidence that links the damage of the cells to the VPH virus. The reported case, with the initial diagnosis of invasive adenocarcinoma, the treatment proposed in two different sites was the ending of pregnancy with cesarean section and hysterectomy and a premature birth, her first pregnancy. The patient asked for a third opinion, where the meticulous revision of the pathology slides (JJCV) with immunohistochemistry with p16 and Ki67 only found in situ lesion, with no evidence of microinvasion and no associated squamous lesion. The colposcopy at the 25th week of pregnancy included all 4 quadrants of the cervix and the external endocervical canal was included. The following observation at week 29th, the regression was 80% and gave the confidence to wait until term and have a precious, first pregnancy, without risk of prematurity as had been the initial approach. Review of the literature looking for cases of adenocarcinoma in situ with spontaneous involution in women with or without pregnancy was not documented. This case would apparently be the first documented case of spontaneous regression of adenocarcinoma in situ, with the particularity that it was initially mistaken as invasive adenocarcinoma.
- Wright VC. Chapter 11, In Modern Colposcopy Text book and Atlas 3rd ASCCP, Wolters Kluwer, Mayeaux an Cox editors. pp: 322.
- Griffin D, Manuck TA, Hoffman MS (2005) Adenocarcinoma in situ of the cervix in pregnancy. Gynecol Oncol 97(2): 662-664.
- Ma J, Yu L, Xu F, Yi H, Wei W (2019) Treatment and clinical outcomes of cervical cancer during pregnancy. Ann Transl Med 7(11): 241.
- Sopracordevole F, Rossi D, Giuseppe JD, Angelini M, Boschian-Bailo P, et al. (2016) Conservative Treatment of Stage IA1 Adenocarcinoma of the Uterine Cervix during Pregnancy: Case Report and Review of the Literature. Case Rep Obstet Gynecol 9: 539-544.
- Wright VC (2003) Cervical squamous and glandular intraepithelial neoplasia: Identification and current management approaches. Salud Publica Mex 3: S417-S429.
- Smith HO, Padilla LA (2002) Adenocarcinoma in Situ of the Cervix: Sensitivity of Detection by Cervical Smear. Will Cytologic Screening for Adenocarcinoma in Situ Reduce Incidence Rates for Adenocarcinoma? Cancer 96: 319-322.
- Kindelberg DW, Krane JF, Lee KR, Glandular neoplasia of the cervix in crumps Diagnostic Gynecologic and Obstetric Pathology. Elsevier Saunders 2nd edn Philadelphia PA pp: 338-339.
- Darragh TM, Colgan TJ, Cox JT, Heller DS, Henry MR, et al. (2013) The Lower Anogenital Squamous Terminology Standardization project for HPV-associated lesions: Background and consensus recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Arch Pathol Lab Med 32: 76-115.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- International Journal of Diabetes (ISSN: 2644-3031)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)





