4298
Views & Citations3298
Likes & Shares
With these old mystical stories from ancient times human interest in the potentially healing power of blood became part of medieval and renaissance science.
Much research and experiments were done to solve the problem of transfer of blood from one healthy living individual into another diseased individual. Most likely the first public experimental demonstration was given by the English physician and anatomist Richard Lower [2] in 1665 in Oxford, connecting the venae jugularis of two dogs. Unfortunately, the blood clotted in the cannula. The observation led to a change in the methodology, connecting the coronary artery of the donor dog with the jugular vein of the recipient dog - the blood did not clot! He was then invited in 1665 by the Royal Society in London to demonstrate his design, which was published in the Philosophical Transactions of the Royal Society, December 1666. Lower [2] was also the first scientist who demonstrated that blood transfusion could be lifesaving. In the experiment he first almost exsanguinated a dog and then transfused the victim with blood from a healthy dog, causing complete recovery. A year later, 23 November 1667, Lower presented a first human experiment in which Arthur Coga was hired by the College for the sum of 20 Shillings to undergo within a month two intravenous transfusions with lambs’ blood, of which the latter did not provide a very cheerful outcome. At the same time in France at the court of Louis XIV the young court physician and “most able Cartesian philosopher” Jean Baptiste Denis from Montpellier together with the surgeon Paul Emmerez did quite some dog-to-dog transfusion experiments [3]. When he was presented a severely ill 15 years old boy with fever and weakness due to the many bloodlettings, he decided to transfuse the boy with lambs’ blood, which resulted in a miraculous curing effect! Shortly thereafter a second 45 years old healthy male was successfully transfused, followed by the son of the Minister of Foreign Affairs of the king of Sweden who fell seriously ill while in Paris. Denis decided to treat him with two subsequent transfusions, and with good success. The report was published in the Philosophical Transactions of the Royal Society of July 1667 (Figure 1) [4].
The following patient transfused by Denis was a 34 years old man Antoine Mauroy, who suffered from a tragic love affair. He received over a period of a couple of months several calf blood transfusions but started after the second transfusion to react with fever, pain in the lumps, increased pulse rate, sweating, and dyspnoea, excreting black urine. Denis has carefully documented the event, thereby uniquely describing for the first time in medical history a classical acute hemolytic transfusion reaction. He survived, but when a few month later his mental condition again deteriorated, Denis decided to treat Antoine Mauroy with another calf blood transfusion, which unfortunately caused his death due to acute lethal hemolysis. Denis was accused of murder but during the Châtelet trial in Paris plead not guilty. However, the conservative Paris University Sorbonne forbid further blood transfusion experiments. Following the enlightenment, beginning of the 19th Century, the progressive Scottish Gynaecologist and Obstetrician James Blundell from London, who did his medical education in Edinburgh, showed a deep interest in the potential of blood transfusion [5]. His interest was not only based on the personal experience with women in labour who postpartum bled to death, but also by the scientific experiments of John Leacock from Barbados. In 1816 John Henry Leacock reported systematic experiments in Edinburgh on dogs and cats that established that donor and recipient must be of the same species and recommended inter-human transfusion [6]. He then returned to Barbados and published nothing more. However, James Blundell, who extended Leacock's experiments and publicized the results widely, is credited with introducing transfusion into clinical use, but he always gave credit to Leacock for his initial work. In fact they were the founders of modern immunology and the principle of compatibility presenting scientific evidence for species specificity. The scientific and clinical value of these observations became much later understood and practiced. Blundell decided based on his animal experiments to apply the lessons learned in human pathology. A 35-year-old man with a terminal stomach cancer was successfully transfused directly. Most of his work was published in The Lancet (Figure 2) [7]. In an editorial of the 1825 Philadelphia Journal of Medicine, Physics and Science Blundell´s premiere has been debated in a footnote arguing that Dr. Philip Syng Physick did the same already in 1885. However, that practice was never published nor presented publicly. Blundell continued his work and managed to save the lives of dozens of women in labor and was frequently consulted about blood transfusion. He was indeed the first clinical specialist who deserved the classification of ‘Transfusion Medicine Specialist’. Despite the many opponents he continued. From time to time, he observed that the transfusion in certain women caused acute hemolysis but was unable to understand the underlying pathophysiology.
Although during the 19th century much scientific progress was made, blood transfusion as a supportive clinical intervention with a life-saving potential was still at square one. The real breakthrough came at the turn of the 19th century with the work of the Viennese physician, pathologist and scientist Landsteiner [8], who discovered the presence of specific antigens on the surface of red cells, genetically determined. He named them blood groups. Following the alphabet, he distinguished the groups A, B and AB besides individuals who did not express A or B antigens and called those O (actually zero because of the absence of A and/or B) [8]. He received in 1930 the Nobel-prize for his work that opened the gate to compatibility in blood transfusion, a major step forward in the safety of clinical transfusion practice [9].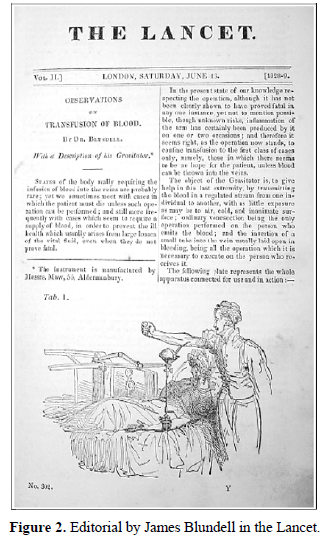
DISEASES - IS THERE A NEED FOR BLOOD TRANSFUSIONS?
Human body cells, tissues, organs and systems may become affected during life, either due to genetic discrepancies (inherited or acquired) or through external influences (acute or chronic). Such conditions may disturb the normal physiologic and homeostatic balances as well as the balances that have changed, but not disturbed through adaptation processes depending on environmental and habitational circumstances. Human blood as a fluid composite has a complex function to which also the protection of a number of physiologic and homeostatic balances are included. Supply of oxygen and removal of carbon dioxide, transportation of nutrients and metabolic waste materials, regulating and balancing substances like growth factors, cytokines and hormones, hemostatic capacity (cellular and coagulation factors), humoral and cellular defense capacity, circulatory system volume and many more. Indeed, the elixir of life or as Goethe made his Dr. Faust express ‘Blut ist ein ganz besonderer Saft’ is a special tissue.
When cell, tissue, organ or system failures start to develop and the natural body response is not sufficiently capable to bring the balance back to normality, a number of interventions may be applied such as medication, supplementary nutrients, limitation of physical activities (resting/relaxing), ventilation, volume and osmotic capacity, targeted irradiation, etc. Here, a specific need for oxygen carrying capacity, primary hemostatic capacity, humoral and cellular immune capacity, protein suppletion such as clotting factors, albumin, anti-thrombin III and C1-esterase inhibitor, support with specific immunoglobulins like anti-Rhesus D, and to a lesser extend circulating volume may develop, despite a normal pathophysiologic response of organs and tissues to increase cell and protein synthesis. Depending on the situation, an acute life-threatening depletion or loss of functions may occur justifying immediate intervention with targeting cellular elements such as red cells and volume with osmotic capacity to restore the homeostatic balance in case of threat of organ failure; or platelets and coagulation factors to support hemostasis and stop blood loss.
Most individuals with a disease have still a normal or subnormal protein and blood cell synthesis in their liver and bone marrow (hematopoiesis) and might just need a bridging of a temporary shortage. However, there are situations and conditions where the disturbed balance needs a support through either medication or intervention with a selected element of the composite blood-transfusion, to restore the balance and allowing the regular synthesis and hematopoiesis processes to gear up and take over. In those chronic situations, usually genetically determent, where organs do not have the capacity to synthesize missing proteins or blood cells, regular support is needed, such as in inherited bleeding disorders and hemoglobinopathies.
Currently science is providing a more detailed insight in both normal physiological processes as well as in the mechanisms at molecular level that cause disturbances of physiologic and homeostatic balances-molecular and even nano-pathophysiology. This development brings along possibilities for extremely precise targeting treatments or precision medicine, in which also human white cells, growth factors, cytokines and hormones play a supportive role. Chimeric Antigen Receptor or CAR-T and focused immune cell therapies such as adoptive immunotherapy using Dendritic and T-cells, have been introduced, engineered from human blood cells in particular autologous white cells like specific T-lymphocytes [10].
BLOOD TRANSFUSIONS – A MULTIFACETED AND DIVERSE TRANSPLANT PRACTICE?
Transfusion of blood and its elements is in principle supportive. Blood and its main cellular and plasma protein components do not cure disease but support a primary curative medical intervention. However, several of the elements of the composite may contribute to the restoration of disturbed physiologic and homeopathic balances like in a threat of organ failure and severe consumption coagulopathies due to massive bleeding, septicemia in agranulocytic newborns, and protein losing morbidities. Progressively ongoing pathophysiologic disease processes could be influenced to slow down and even brought to a complete interruption.
Cellular and immune therapies are increasingly used in cancer and leukemia patients to specifically target tumor cells, kill and eliminate through specific apoptotic mechanisms and capacities, and tip the disturbed balance to healing and even complete recovery. However, their immune capacities are now extended into debilitating autoimmune diseases, infectious diseases and even into organ transplantation.
In conclusion, the overarching and bridging science of transfusion medicine [11] may justify the use of the term ‘transfusions’ in relation to the support of treatment of a diverse variety of entities and stages of ‘diseases'.
- Lindeboom GA (1954) The story of blood transfusion to a Pope. J Hist Med Allied Sci 9(4): 455-459.
- Lower R (1666) Phil Tran R Soc London 1: 353.
- Hoff HE, Guillemin R (1963) The first experiments on transfusion in France. J Hist Med Allied Sci 18: 103-124.
- Denis JB (1667) A letter concerning a new way of curing sundry diseases by transfusion of blood, written to Monsieur de Montmor, Councellor to the French King, and Master of Requests. Phil Tran R Soc London 3: 489-504.
- Young JH (1964) James Blundell (1790-1878): Experimental physiologist and obstetrician. Med Hist 8: 159-169.
- Leacock JH (1816) On the transfusion of blood in extreme cases of haemorrhage. Med Chir J Rev 3: 276.
- Blundell J (1828) Observations on transfusion of blood. Lancet 2: 321-324.
- Landsteiner K (1901) Agglutination phenomena of normal human blood. Wien Klin Wochenschr 14: 1132-1134.
- Nobel Price Laureates (2020) Available online at: http://www.nobelprice.org
- Cellular Therapies (2016) Principles, Methods and Regulations. AABB Press, Bethesda, MD.
- Smit Sibinga CTh, Abdella YE (2018) Transfusion Medicine-A Bridging Science. Intern Med Rev 41: 1-30.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)




