Case Report
Catastrophic Antiphospholipid Syndrome Following Malaria in a Young Sudanese Female with Systemic Lupus Erythematosus: Case Report
4134
Views & Citations3134
Likes & Shares
Systemic lupus erythematosus (SLE) is a heterogeneous autoimmune rheumatological disorder manifested by several clinical presentations. It may coexist with catastrophic antiphospholipid syndrome (CAPS) which is a life-threatening unusual form of Antiphospholipid Syndrome (APL) with a high mortality rate and adverse sequels in survivors.
A 20-year-old Sudanese female diagnosed with SLE associated with APL and complicated with probable CAPS following malaria. The patient was treated with glucocorticoids, anticoagulants and supportive treatment. Due to the financial burden neither IVIG nor plasma exchange were administered- which are the standard of care. The end result was peripheral digital gangrenes with autoamputation of the second, third, fourth and fifth fingers.
This case report highlights the importance of early recognition of CAPS as a devastating form of APL which requires rapid intervention and management, we find the outcome in such patient is acceptable.
Keywords: Catastrophic antiphospholipid syndrome, Systemic Lupus erythematosus, Malaria, Proliferating cell nuclear antigen
Abbreviations: ANA: Antinuclear Antibody; AntiCCP: Anticyclic Citrullinated Peptide; ALT: Alanine Transferase; APL: Antiphospholipid Syndrome; APPT: Partial Thromboplastin Time; AST: Aspartate Transferase; CAPS: Catastrophic Antiphospholipid Syndrome; CRP: C-Reactive Protein; CT: Computed Tomography; C3: Complement 3; C4: Complement 4; CXR: Chest X Ray; DNA: Deoxyribonucleic Acid; DsDNA: Double Stranded Deoxyribonucleic Acid; DIP: Distal Interphalangeal; ECG: Electrocardiogram; ESR: Erythrocyte Sedimentation Rate; K: Serum Potassium; Na: Serum Sodium; MCP: Metacarpophalangeal; MCV: Mean Corpuscular Volume; MCH: Mean Corpuscular Hemoglobin; PT: Prothrombin Time; PCNA: Proliferating Cell Nuclear Antigen; PIP: Proximal Interphalangeal; RBG: Random Blood Glucose; SLE: Systemic Lupus Erythematosus; WBC: White Blood Cell
BACKGROUND
Systemic lupus erythematosus (SLE) is a multisystem, autoimmune disease affecting mainly those of childbearing age of Black and Hispanic origin [1]. It affects multiple organs and runs a variable course ranging from mild to life-threatening [2]. Antiphospholipid syndrome (APL) is an autoimmune syndrome that leads to thrombosis involving the arterial system as well as the venous system with morbidity in pregnancy [3]. Catastrophic antiphospholipid syndrome (CAPS) is the rarest form of it and it occurs in <1% [1,4].
The patient was diagnosed with severe SLE and probable CAPS following malaria which resulted in devastating sequelae of peripheral digital gangrenes. Despite this, the patient survived with what we conceive to be an acceptable outcome.
CASE PRESENTATION
A 20-year-old Sudanese female presented with two weeks history of intermittent fever associated with headaches which responded partially to analgesia. The patient did not experience any other neurological symptoms but complained of generalized fatigability and small joints pain that involved the metacarpophalangeal (MCP), proximal interphalangeal (PIP) and distal interphalangeal (DIP) bilaterally. She also experienced lower back pain that improved with rest, it was associated with morning stiffness mainly in the small joints lasting less than 30 min.
The patient was treated for malaria based on positive blood film for malaria (BFFM) with Artemether/lumefantrine according to the local protocol. The patient did not experience any improvement and 3 days prior to admission she experienced pain and itching with numbness and black discoloration of the fingertips and toes. The patient had no skin rashes, aphthous ulcers, eye symptoms, or other joint pain. She had dysuria and vomiting (twice) but no abdominal pain, diarrhea, or other symptoms.
Past medical history was significant for Raynaud’s phenomena and she was not known to be allergic to any medications. She had irregular menses for the past 3 years. Family history was positive for first degree relative with SLE (sister). Socially, the patient presented as a single, high school dropout female of low socioeconomic background.
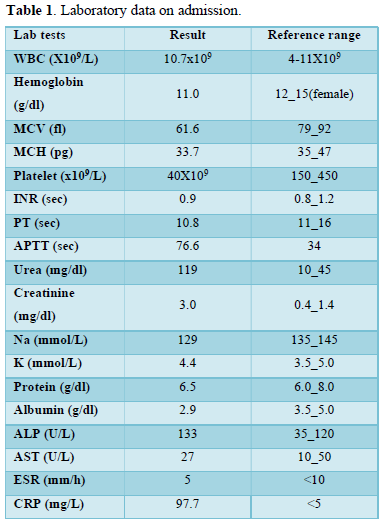
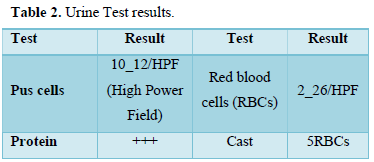
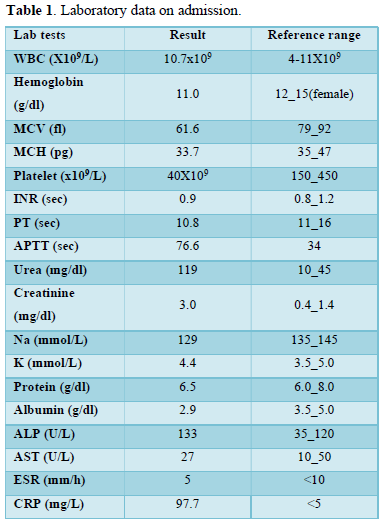
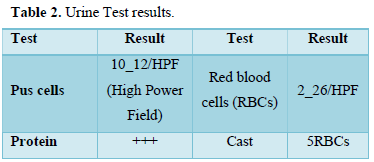
Clinical examination on admission revealed an ill-appearing, pale, underbuilt female with no jaundice and normal vital signs. Other clinical examinations were insignificant. Laboratory findings on admission are presented in Tables 1 & 2.
The patient was admitted for further workup. As her BFFM still positive she was treated with artesunate injection as per local policy, beside supportive management.
Three days later the patient’s condition deteriorated and developed subconjunctival hemorrhage in the left eye, vaginal and gum bleeding, dark urine and epistaxis from both nostrils of a minimal amount. Both hands showed dry gangrenous fingertips on all fingers and the second and third toes of both feet were tender over fingertips. Other musculoskeletal examinations were normal.
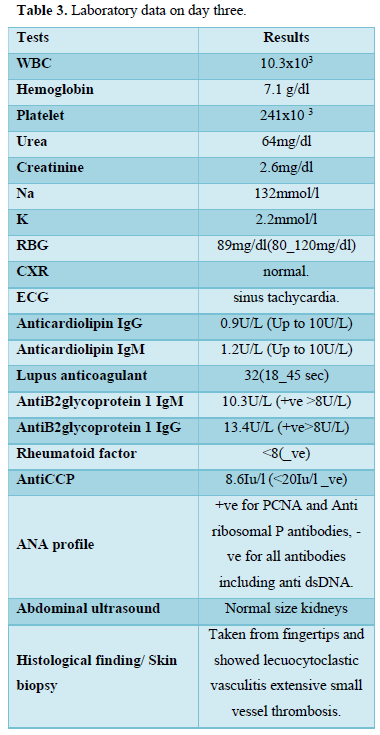
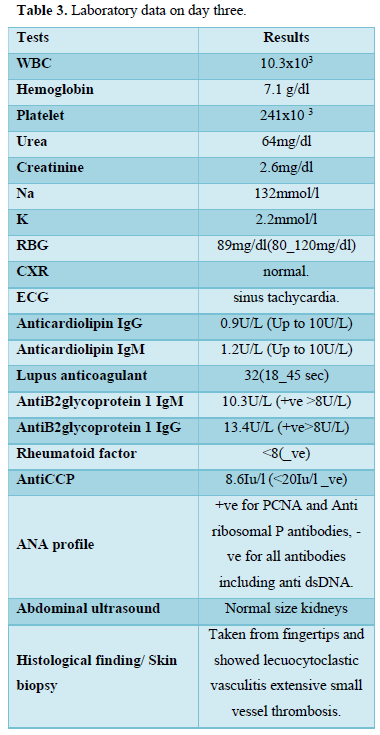
Vital signs were as follow Blood pressure (BP):100/60, Heart rate (HR): 112 beats/min, Respiratory rate (RR): 26/min, Oxygen saturation (SPO2) on room air: 94%. The patient was conscious and oriented with no focal neurological signs. The cardiovascular system/chest/abdomen examination was unremarkable. The workup is presented in Table 3.
The patient was monitored closely and received the best appropriate treatment (multiple pack red blood cells and fresh frozen plasma).
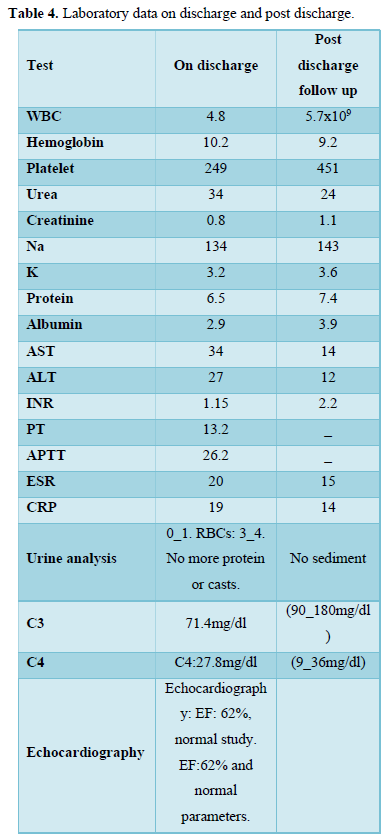
A diagnosis of SLE with probable CAPS following malaria was reached. 5 days later the patient improved dramatically. Following patient counselling treatment was commenced which included methylprednisolone 500mg infusion for 3 consecutive days followed by oral prednisolone 0.5mg/kg (30mg) that was tapered to a maintenance dose of 10mg, Hydroxychloroquine 200mg twice daily, warfarin 5mg bridged with low molecular weight heparin, bosentan 62.5mg twice daily, mycophenolate mofetil 1gm twice daily (chosen over cyclophosphamide by the patient and her family due to concern over fertility) and calcium supplement once daily. IVIG and plasma exchange was offered but were not affordable by the patient due to their financial burden. One week later, the patient was discharged in a clinically and lab-wise stable condition.
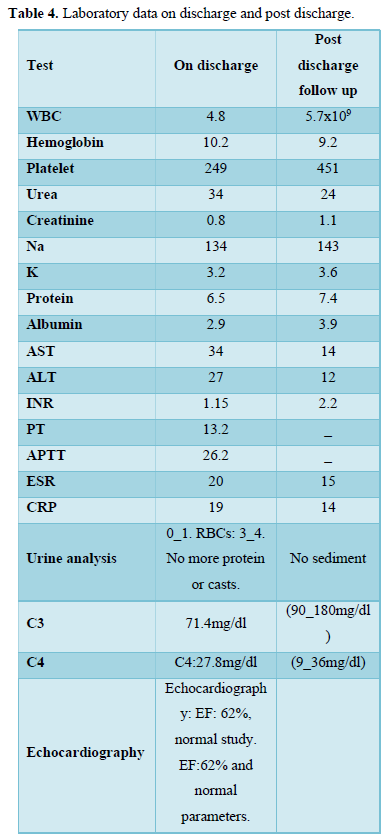
The patient was scheduled for follow up one month later but due to the COVID-19 pandemic, the patient was not seen for almost five months. Later, when she was seen in the post-discharge clinic, the second, third, fourth and fifth fingers were autoamputated respectively. Table 4 shows the lab investigations upon discharge and follow up visit.
DISCUSSION
Antiphospholipid syndrome (APL) is an acquired autoimmune disease characterized by the production of autoantibodies (anticardiolipin, lupus anticoagulant and B2 glycoprotein 1) that are primarily responsible for widespread thrombosis including arterial, venous and small vessels alongside pregnancy morbidity [1,3]. CAPS is a frightening, extremely rare type of APL syndrome that occurs rapidly and was first recognized in 1992 by Ronald Asherson [2,5,6]. Although rare, it affects multiple organs [2,5,7] and has high mortality which necessitates the early recognition and prompt accurate intervention.
CAPS is classified into definite and probable according to certain preliminary criteria [4,8] which are:
- Involvement of at least 3 organs or systems
- Rapid onset of clinical features in less than one week
- Histopathological confirmation of small vessels occlusion in at least one organ or tissue
- Presence of antiphospholipid antibodies
Definite CAPS requires the presence of all 4 criteria while probable CAPS requires 3 out of 4 criteria to be fulfilled. The exact cause of CAPS is still elusive but different mechanisms may play a fundamental role in the pathogenesis such as infections, endothelial damage with complement activation, upregulation of adhesion molecules and reduction of fibrinolytic factors which collectively lead to microthrombi formation and occlusion of small vessels resulting in tissue ischemia and release of many cytokines leading to a systemic inflammatory response which is the major culprit of inflammatory and clinical features [4,9,10]. CAPS is a fatal condition, early recognition and accelerated management is the cornerstone to safe life [11].
Infections such as malaria, which is caused by a parasitic infection and classified as an endemic disease in Sudan, was conceived to be the main causative agent in this case as it is considered to be a major precipitating reason for CAPS through immune system activation [6,12,13].
CAPS is treated with glucocorticoids, anticoagulants and antiplatelets while in severe cases, plasma exchange and intravenous immunoglobulin are best recommended alongside treating any infections or triggering factors. If there is no response, cyclophosphamide for SLE flare or Rituximab can be considered [2,5,14].
SLE is an autoimmune disorder that is associated with immune complexes deposition that can affect the kidneys badly and leads to lupus nephritis which is diagnosed by the presence of proteinuria >0.5gm/24h (urinary protein+++) or urine albumin/creatinine ratio >0.5 and active urinary sediment (RBCs cast >5, WBCs >5) after the exclusion of any underlying causes. A renal biopsy is considered an added criterion [14]. In this case, the patient fulfilled the criteria having >5 RBCs cast and urine albumin /creatinine ratio 1.2. A renal biopsy was requested but the patient refused to have it done.
PCNA is a protein that is essential for DNA repair and replication through its role in enhancing the action of DNA polymerase. It correlates with disease activity and associates with renal involvement [15,16] as presented in our patient’s case who was positive for PCNA.
SLE is a multisystem connective disease, associated with a myriad of clinical manifestations and associations, APL being one of the serious ones. CAPS is a lethal variant of APL that can be followed with sepsis as suspected in our patient [17].
Although the patient exhibited a fulminant clinical presentation, the patient’s clinical outcome is being satisfactory and acceptable given the resource and financial constraints that affected the patient’s care.
DECLARATIONS
Ethics approval and consent to participate
The patient in our case report has signed a written consent form and she has no concerns. A copy of the consent form is available upon request.
CONSENT TO PUBLISH
Written consent was obtained for publication and she reviewed all data included in the manuscript before submission.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
COMPETING INTERESTS
The authors declare that they have no competing interests.
FUNDING
The authors declare that no fund or financial support was received for this case report.
AUTHORS’ CONTRIBUTIONS
HA was involved in patient care and case selection. AR was involved in patient care, writing and reviewing the abstract, case description, discussion, and the conclusion of the manuscript. Both authors contributed to the planning of the case report, manuscript revision and final approval of the manuscript.
ACKNOWLEDGEMENTS
None.
- El Agib ENM, Eltahir NIA, Adam MEAE, Mahmoud ZIT, Yousif HHM, et al. (2019) Catastrophic Antiphospholipid Syndrome in Combination with SLE Treated by Rituximab: A Case Report and Literature Review. Lupus Open Access 4(1): 137.
- Bucciarelli S, Erkan D, Espinosa G, Cervera R (2009) Catastrophic antiphospholipid syndrome: Treatment, prognosis, and the risk of relapse. Clin Rev Allergy Immunol 36(2-3): 80-84.
- Harris EN, Pierangeli SS (2004) Primary, Secondary, Catastrophic Antiphospholipid Syndrome: Is there a difference? Thromb Res 114(5-6 SPEC. ISS.): 357-361.
- Ruffatti A, Calligaro A, Lacognata CS, D’Odorico A, Colpo A, et al. (2020) Insights into the pathogenesis of catastrophic antiphospholipid syndrome. A case report of relapsing catastrophic antiphospholipid syndrome and review of the literature on ischemic colitis. Clin Rheumatol 39(4): 1347-1355.
- Mesa CJ, Rife EC, Espinoza LR (2020) Catastrophic antiphospholipid syndrome: Is life-long anticoagulation therapy required? Clin Rheumatol 39(7): 2115-2119.
- Mendoza-Pinto C, García-Carrasco M, Cervera R (2018) Role of Infectious Diseases in the antiphospholipid syndrome (Including Its Catastrophic Variant). Curr Rheumatol Rep 20(10): 62.
- Skoczynska M, Crowther MA, Chowaniec M, Ponikowska M, Chaturvedi S, et al. (2020) Thrombotic microangiopathy in the course of catastrophic antiphospholipid syndrome successfully treated with eculizumab: Case report and systematic review of the literature. Lupus 29(6): 631-639.
- Liu L, Tsai HH, Lafian A, Sadeghi E (2019) A Feather in Your CAPS: Probable CAPS treated with rituximab. 3(2): 9-13.
- Triplett DA, Asherson RA (2000) Pathophysiology of the Catastrophic Antiphospholipid Syndrome (CAPS). 159: 154-159.
- Madkaiker S (2019) Catastrophic antiphospholipid syndrome - an unusual case report. Indian J Crit Care Med 23(6): 276-280.
- Singh S (2015) World Journal of Pharmaceutical Research. Age (Omaha) 20: 60.
- Trampuz A, Jereb M, Muzlovic I, Prabhu RM (2003) Clinical review: Severe malaria. Crit Care 7(4): 315-323.
- Rodríguez-pintó I, Moitinho M, Santacreu I, Shoenfeld Y, Erkan D, et al. (2016) Autoimmunity Reviews Catastrophic antiphospholipid syndrome (CAPS): Descriptive analysis of 500 patients from the International CAPS Registry. Autoimmun Rev 15(12): 1120-1124.
- Kalmanti L, Lindhoff-last E (2020) Treatment of Vascular Thrombosis in Antiphospholipid Syndrome: An Update. Hamostaseologie 40(1): 31-37.
- Maga G, Hübscher U (2003) Proliferating cell nuclear antigen (PCNA): A dancer with many partners. J Cell Sci 116(15): 3051-3060.
- Zhang M, Jie H, Wu Y, Han X, Li X, et al. (2020) Increased MLKL mRNA level in the PBMCs is correlated with autoantibody production, renal involvement and SLE disease activity. pp: 1-16.
- Unlu O, Erkan D (2017) Catastrophic Antiphospholipid Syndrome: Candidate Therapies for a Potentially Lethal Disease. Annu Rev Med 68: 287-296.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Chemotherapy Research Journal (ISSN:2642-0236)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Pathology and Toxicology Research
- BioMed Research Journal (ISSN:2578-8892)


