Case Report
Reversion of the Clinical Picture of a Patient with Normal Pressure Hydrocephalus
4198
Views & Citations3198
Likes & Shares
Normal Pressure Hydrocephalus is a clinical condition characterized by the urinary incontinence, gait disturbance and dementia. It is very common in the elderly, and the diagnosis is made by clinical, physical and imaging examination, having as the gold standard tool, the tap test.
Objective: Report a clinical case of a patient with idiopathic Normal Pressure hydrocephalus whose symptoms were dramatically reduced after treatment with LiquoGuard.
Method: The study information was obtained through literature review, patient’s medical record associated with patient interview, photographic records of patient examinations and imaging exams performed. A 72-year-old was patient was introduced, presenting specific symptoms and signs characterizing the triad and magnetic resonance imaging findings compatible with normal pressure hydrocephalus.
Final Considerations: The patient underwent to a modified surgical treatment with severe reduction of symptoms before the procedure over the CSF removal through LiquoGuard to minimize the risk of complications in the surgical procedure.
Keywords: Normal pressure hydrocephalus, Dementia, LP shunt
INTRODUCTION
Idiopathic Normal Pressure Hydrocephalus (NPHi) is a syndrome characterized by the Adams-Hakimtriad (urinary incontinence, gait disorder and dementia), which can be diagnosed through clinical findings associated with brain imaging, with dilation findings ventricular, distortion of the fibers of the corona radiata and by the normal pressure of the cerebrospinal fluid during the lumbar puncture [1,2].
Among the most affected groups, adults and the elderly tend to concentrate cases of NPHi, being one of the few treatable etiologies of dementia. Above 80 years of age, it has a higher prevalence, and its incidence is increasing worldwide [3], however under diagnosis is expected, mainly because the main findings are very non-specific, especially in the older population [2]. It is estimated that approximately 5.7% of the elderly over 70 years old meet criteria for PNH in the Norwegian population, and in Brazil the prevalence is approximately 5.38% of the total of patients with dementia [4].
The increase in intracranial pressure results in stretching and compression of the fibers of the corticospinal tract in the corona radiata, which are responsible for the innervation of the lower limbs, due to the proximity to the lateral ventricles, causing the gait disorder. In addition, impaired cerebral perfusion, as well as prefrontal regions, and brainstem compression (such as the pedunculopontine nucleus) also contribute to it [5].
Gait disorders are usually the first or most characteristic symptom of the syndrome. The gait of a patient with PNHi is scrambled, magnetic and broad-based. With the progression of the disease, it becomes wide, slow, with short steps and with difficulty in starting (a finding of gait of the astasia-abasia type). The gait of a patient with NPHi has typical findings that consist of an external rotation of the foot, difficulty in rotating the body on its own axis and difficulty in starting to walk, with the possibility of its freezing [6].
Urinary incontinence is the result of stretching the sacral fibers of the periventricular corticospinal tract culminating in loss of voluntary control of bladder contraction. Dementia, on the other hand, results from ventricular enlargement, causing the cortex to displace the internal table of the calvary and the radial shear forces cause dementia [7].
On clinical examination, not all signs and symptoms of the Adams-Hakimtriad can be found, and similarly, other pathologies are usually associated with NPHi, and because of this, the diagnosis has both clinical and imaging criteria from divisions between probable, possible and improbable of the diagnosis, but in Brazil there is no agreement on the diagnostic criterion using associated imaging tests [6]. Among the most important differential diagnoses are Alzheimer’s disease and vascular dementia [8].
The treatment is mostly surgical, in many cases the Lombo-Peritoneal Derivation (DLP) with valve is the first line of resolution of the condition due to minimizing the complications of an intracranial procedure [9], however there are other forms of treatment, such as other leads and ventriculostomy, as well as non-surgical forms such as carbonic anhydrase inhibitors and serial lumbar punctures for non-surgical patients.
OBJECTIVE
To report a clinical case of a patient with idiopathic Normal Pressure hydrocephalus who had his symptoms drastically reduced after treatment.
METHODOLOGY
The work information was obtained by reviewing the literature, the patient’s record associated with the patient’s interview, photographic records of the patient’s examinations and the examinations performed.
CLINICAL CASE
A healthy 72-year-old patient, born and living in Sao Paulo, he started to experience gait apraxia, dementia and urinary incontinence, with a time to progress until seeking medical care of 6 months, denied comorbidities. An MRI scan was performed that showed bilateral ventricular dilation compatible with normal pressure hydrocephalus.
Based on the diagnostic hypothesis, a Tap Test was programmed and, for greater patient safety, a CSF drainage device called LiquoGuard was used after examinations, which was installed on the patient for 48 h with a total drainage of 120 ml. After the drainage of the cerebrospinal fluid, the patient improved his symptoms and, through the patient’s positive response, a lumbar-peritoneal shunt with a valve was indicated (Figure 1).


CASE DISCUSSION
Being one of the few treatable causes of dementia, the diagnosis of normal pressure hydrocephalus is of great importance in the case and in the patient’s quality of life. Among the Adams-Hakim criteria, the three symptoms are found in the clinical case, which helps to formulate the diagnostic hypothesis, however the triad is not pathognomonic, in addition to the signs and symptoms of the syndrome being non-specific and common due to several comorbidities at older ages. advanced, which leads to the need for complementary exams.
The association with comorbidities is also of great importance at the time of diagnosis. A Brazilian study carried out with a survey of medical records at the Hospital das Clínicas of the Ribeirão Preto Medical School showed that 40% of the patients had systemic arterial hypertension, and 32.3% already had some previous involvement of the central nervous system [4]. This shows that even with great suspicion of the diagnosis, it is necessary to exclude other causes of neurological deficits due to causes such as stroke, or more common causes of dementia such as Alzheimer’s disease and vascular dementia [8].
The imaging exam of best choice to diagnose NPHi is magnetic resonance, being the best method of visualizing altered structures, and to support the diagnosis, CSF flow studies and magnetic resonance spectroscopy [10]. Magnetic resonance findings consist of:
- Ventricular increase, calculated by the Evans Index and suggesting an increase if it is greater than or equal to 0.3;
- Callous angle between 40° and 90°;
- Dilation of the temporal horn sun related to hippocampal atrophy;
- Narrow medial cisterns and subarachnoid space;
- Dilatation of Sylvian fissures;
- Groove dilation showing disproportionately increased subarachnoid hydrocephalus;
- Periventricular hypodensities on CT or T2 or hyperintensities of recovery from liquid-attenuated inversion on MRI;
- Bulging of the lateral ventricular roof making it possible to visualize, in this case, an upward curvature and elongation of the corpus callosum [11].
In the study of the flow in the CSF, a flow greater than 24.5 ml / min has a high specificity for NPHi, however the finding of emptying of the aqueductal flow observed in the T2-weighted images is not useful. In addition to the above findings through MRI, nuclear medicine studies have shown some non-specific signs seen in NPHi, which are:
- Lateral ventricles usually in the form of a “trident”, but they can appear in the form of a “heart”;
- Tracer remains in the ventricular system for more than 24 to 48 h due to absorption deficiency;
- Absence of tracer extension in the upper aspect of the lateral ventricles;
- CSF reflux into the lateral ventricles [12].
The tap test, or examination of the lumbar puncture, has an effect equivalent to an acute treatment for the patient, often already showing signs of improvement of the condition, and in the same way, the patient had acute improvement of the condition due to the decrease in the amount circulating cerebrospinal fluid, which further corroborates the PNH picture, both of motor functions, but mainly of cognitive functions [13] (Figure 2).
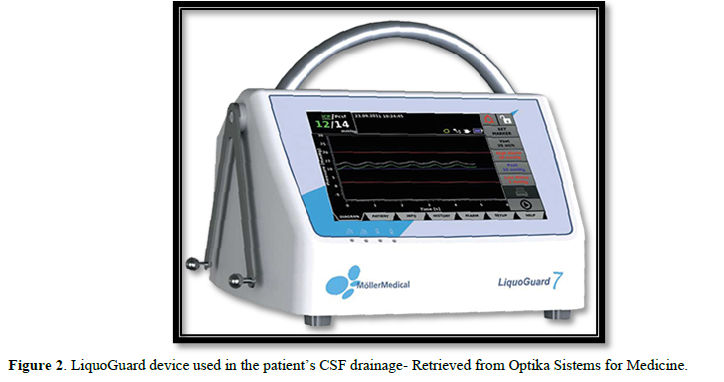
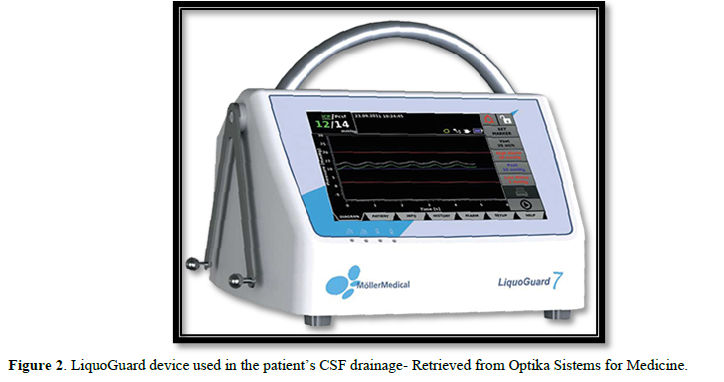
LiquoGuard was used as a form of treatment in order to reduce the risk of hemorrhage due to sudden decompression or obstruction of the catheter due to the monitoring of CSF pressure in real time, being a new treatment method with less risk of complications and with the associated advantages of improving the condition acutely, with some studies showing its advantages in studies of increased intracranial pressure [15]. After the procedure, the procedure performed was the lumbar-peritoneal shunt with a valve.
FINAL CONSIDERATIONS
Among the differential diagnoses of dementias associated with gait disorders and urinary incontinence, normal pressure hydrocephalus is highlighted because it is an easily treatable etiology, both palliative and therapeutic, being more common in the elderly and an important differential diagnosis of other comorbidities that cause such symptoms, and dementias, in diagnoses such as Alzheimer’s and vascular dementia. Due to the lack of consensus in Brazil on which criterion to use, understanding the pathophysiology of the disease and looking for complementary exams is necessary when evaluating this pathology. A modified surgical treatment was performed on the patient with a severe reduction of the symptoms he had before the procedure, and the LiquoGuard is safer than the tap test, having the same amount of CSF removed in 48 h, but with less associated risk hemorrhage by sudden decompression.
- Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH (1995) Symptomatic Occult Hydrocephalus with Normal Cerebrospinal-Fluid Pressure-A Treatable Syndrome. N Engl J Med 273: 117-126.
- Brean A, Eide PK (2008) Prevalence of probable idiopathic normal pressure hydrocephalus in a Norwegian population. Acta Neurol Scand 118: 48-53.
- Jaraj D, Rabiei K, Marlow T, Jensen C, Skoog I, et al. (2014) Prevalence of idiopathic normal-pressure hydrocephalus. Neurology 82(16): 1449-1454.
- Melato L, Bigal ME, Speciali JG (2000) Hidrocefalia de pressão normal: avaliação de cinco anos de experiência e revisão de literatura. Medicina (Ribeirão Preto) 33(4): 499-505.
- Mongin M, Hommet C, Mondon K (2015) Hydrocéphalie à pressionnormale: miseau point et aspects pratiques [Normal pressure hydrocephalus: A review and practical aspects]. La Revue de medicine interne 36(12): 825-833.
- Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM (2005) Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57(3 Suppl): S4-S5.
- Williams MA, Malm J (2016) Diagnosis and Treatment of Idiopathic Normal Pressure Hydrocephalus. Continuum (Minneapolis, Minn.) 22: 579-599.
- Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, et al. (2013) The global prevalence of dementia: A systematic review and meta-analysis. Alzheimers Dement 9(1): 63-75.e2.
- Aoki N (1990) Lumbo-peritoneal shunt: Clinical applications, complications, and comparison with ventriculo-peritoneal shunt. Neurosurgery 26(6): 998-1004.
- Bradley WG Jr (2016) Magnetic Resonance Imaging of Normal Pressure Hydrocephalus. Semin. Ultrasound CT MR 37(2): 120-128.
- Hashimoto M, Ishikawa M, Mori E, Kuwana N, Study of INPH on neurological improvement (SINPHONI) (2010) Diagnosis of idiopathic normal pressure hydrocephalus is supported by MRI-based scheme: A prospective cohort study. Cerebrospinal Fluid Res 7: 18.
- Graff-Radford NR, Jones DT (2019) Normal Pressure Hydrocephalus. Continuum (Minneapolis, Minn.) 25(1): 165-186.
- Rocha S, Almeida SM, Pizzanni L, Romero B, Perboni T, et al. (2016) Melhora cognitiva durante taptest em pacientes com hidrocefalia de pressão normal. Psicologia, Saúde e Doenças 17(1): 67-73.
- LiquoGuard System. Optika Systems for Medicine. Accessed on: September 14, 2019. Available online at: http://www.optikasp.com.br/sistema-liquoguard.html
- Linsler S, Schmidtke M, Steudel WI, Kiefer M, Oertel J (2013) Automated intracranial pressure-controlled cerebrospinal fluid external drainage with LiquoGuard. Acta Neurochir Suppl 155(8): 1589-1595.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Spine Diseases
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- International Journal of AIDS (ISSN: 2644-3023)




