1971
Views & Citations971
Likes & Shares
Patient satisfaction is a key indicator of healthcare quality and hospital performance. This study underscores the critical role of effective nurse–patient communication in enhancing patient satisfaction within medical and surgical wards. Despite its importance, many patients report poor experiences with nursing communication, often citing a lack of empathy, clarity, and engagement factors that contribute significantly to dissatisfaction. The findings point to the need for improved communication strategies that prioritize patient-centeredness and emotional responsiveness. Additionally, fostering supportive work environments for nurses is essential to enabling consistent, meaningful interactions with patients. By aligning organizational values and promoting cohesive efforts across staff and management, healthcare institutions can create a culture that supports high-quality communication and, in turn, improved patient satisfaction.
Measuring patient satisfaction can be regarded as a therapeutic intervention and a crucial criterion for formulating and assessing organizational policies and decisions [13]. Health service quality positively influences patient satisfaction. The primary determinants of patient satisfaction include demographic characteristics, patient expectations, and their experiences. Additionally, communication plays a significant role in influencing patient satisfaction. Quality nursing care fulfills the needs and expectations of patients, and patient satisfaction is influenced by their expectations [14]. Patients tend to prioritize aspects such as communication, attentive listening, kindness, and responsiveness from their nurses [7]. As patient satisfaction is regarded as one of the indicators of nursing care quality, the sense of satisfaction derived from communication with the nurse is considered a fundamental right of every patient [15]. Hospital infrastructure does not impact the quality of service, whereas hospital facilities significantly affect service quality. Both medical and non- medical personnel behavior within the hospital also significantly influences service quality. Additionally, the cost is not a determining factor in selecting hospital facilities that impact service quality. And due to this reason, there have been considered the plans of creating, maintain and enhancing patient satisfaction in recent years [16]. There was and is still a plan that communication skills should be taught during undergraduate education and training in the health professions [1]. Patient express the dissatisfaction with services particularly with long time waiting time poor staff attitudes, lack of respect for patient rights, and inadequate information sharing. Patients' perceptions of the quality of healthcare they receive are heavily influenced by the quality of their interactions with healthcare providers [17,18]. Consequently, patient satisfaction with nursing communication and palliative care may be influenced by various factors including the patient's level of knowledge about effective communication, their expectations, past experiences with hospitalization, perceptions, gender, and individual characteristics [19]. Those in need of healthcare aspire for excellence in nursing services, which is also the primary goal for those who provide care [20] It suggests that patients' needs are essentially a demand for high-quality nursing care, which nurses strive to fulfill [20]. Negative perceptions from patients can exacerbate the stress they already experience due to their medical condition [21].
It has been observed that patient ward services, food services, reception staff services, and welfare services significantly impact patients' satisfaction. However, in some cases, certain factors such as physical appearance, pharmacy services, laboratory services, blood bank services, x-rays, ultrasound services, billing services, outpatient department (OPD) services, emergency services, and housekeeping services showed no significant impact on patient satisfaction. Continuous improvement in the system can have an overall impact on the level of patient satisfaction in any hospital. Other factors play a crucial role in determining patient satisfaction with healthcare services in private hospitals in Karachi. While the strengths of healthcare organizations, as highlighted by patients, should be maintained, there is a need for more focused planning and management of certain services. Therefore, it is not only the respect and time nurses spent with patients that would determine patients’ satisfaction but also kindness and adequate information about their condition and treatment [22].
In the study conducted in Spain by Lotfi and his colleagues in 2019 about “nurse-patient communication and patient satisfaction from nursing care”, they discovered in their results that patient’s satisfaction was low from nurses’ services. Most of patients did not know their nurse, and nurses were only on the patient’s bedside when there were taking medications and dressing wounds. It was conducted to assess the satisfaction of patients with burns in a Spanish burn unit [15].
In Rwanda, a significant gap has been identified in the healthcare system where patients have expressed the need for interactions with caring and empathetic providers. These patients desire healthcare professionals who can freely share all necessary information and actively involve them in their own care decisions. This need is particularly pronounced among patients with limited literacy and financial resources, who heavily rely on healthcare providers for managing their health and making informed decisions [23]. As nurses spend the majority of their time with patients, they play a critical role in determining patient satisfaction with communication. Therefore, dissatisfaction with nursing care can sometimes indicate poor healthcare quality, particularly in terms of communication [4]. This study seeks to assess thematic areas that have received limited attention, particularly patients' expectations and perceptions regarding communication.
PROBLEM STATEMENT
When patients and healthcare providers listen and communicate effectively with each other, they are likely to develop a shared understanding. This mutual understanding can significantly enhance future decision-making and improve the quality of care that patients receive. Effective communication fosters trust, ensures that patients' needs and preferences are understood, and enables providers to offer more personalized and appropriate care. This collaborative approach not only empowers patients but also leads to better health outcomes and increased patient satisfaction. The problem of substandard communication between nurses and patients is a common issue worldwide. Despite the prevalence of this problem, previous research often reveals a scarcity of requisite statistics or evidence. The research industry has also identified nurse-patient communication as a significant challenge in the Saudi Arabian health system. This challenge is exacerbated by the fact that many of the nurses are expatriates, which can lead to language barriers and cultural differences that hinder effective communication in Saudi Arabia [24]. This issue is not unique to Saudi Arabia; it is a growing concern in many countries due to increasing levels of immigration. The influx of expatriate healthcare workers can lead to communication barriers and cultural differences that affect the quality of nurse-patient interactions. These challenges underscore the need for improved communication strategies and cultural competence training to ensure effective and empathetic care across diverse populations [24].
In a previous study conducted in South Africa on the reasons for nursing staff abusing patients, many patients reported instances of clinical neglect, as well as verbal and physical abuse from nursing staff. This highlights the importance of addressing communication issues, as poor interactions can lead to more severe problems, including neglect and abuse. Effective communication training for healthcare providers, along with stricter enforcement of professional conduct standards, is essential to improve patient care and safety.
Ineffective communication is a major cause of critical medical incidents during hospitalization and is responsible for a significant number of patient grievances. Many of these events could have been easily prevented with proper communication skills. Improving communication between doctors and patients is paramount to avoid such life-threatening events. Effective communication ensures that patients understand their diagnoses, treatment plans, and care instructions, which can prevent misunderstandings and errors. Enhanced communication training for healthcare providers, clear communication protocols, and encouraging a culture of openness and empathy can significantly improve patient safety and satisfaction. Recent research demonstrates that communicating care is as important as delivering medication to patients [17]. Though, some studies conducted in Jordan communicated that majority of participants had positive experiences regarding respect and time nurses spent with patients, there were still reports of patients’ dissatisfaction with information offered because they believed the information given was inadequate [14]. This can also be supported by another study conducted in Ethiopia. It revealed that patients had lowest satisfaction with nursing care in the quality and quantity of information nurses gave them [25]. Various studies have highlighted communication problems between patients and nurses. These studies report that nurses often do not make sufficient efforts to establish positive interactions with patients. Many issues stem from a perceived lack of interest and selfless concern for patients' well-being among hospital staff, including nurses. This decreased sense of empathy and engagement can lead to misunderstandings, patient dissatisfaction, and lower quality of care. Improving communication skills and fostering a culture of compassion and empathy are essential steps to address these issues [10,11]. Studies reveal that nurses have been trained to establish effective communication; however, they often do not utilize these skills when interacting with patients in clinical settings. This disconnects between training and practice contributes to misunderstandings and patient dissatisfaction. Addressing this issue requires not only continuous communication training but also measures to ensure that these skills are consistently applied in real-world interactions [2]. And consequentially, these substandard relationships have not led to personal satisfaction [4, 25].
- The aim of this study is to assess patient satisfaction with nurses' communication for patients with medical surgical conditions in the surgical service at Kibogora District Hospital.
- Objective is to evaluate the level of patient satisfaction with nurse-patient communication in the surgical service at Kibogora District Hospital.
METHODOLOGY
This study employed a quantitative approach as defined by Gerrish and Lacey (2010), focusing on research designs and methods that yield numerical data. The methodology utilized a descriptive cross-sectional design and was conducted between September 14th and 18th, 2023, at Kibogora District Hospital in Nyamasheke district, which provides both secondary and tertiary healthcare services to patients of all age groups, both inpatient and outpatient.
Participants were selected based on predetermined inclusion and exclusion criteria. Adult patients aged 18 and above, admitted to either the medical or surgical ward for palliative care during the data collection period, were included. The inclusion criteria specified that patients must be in stable general condition, fully conscious, able to communicate, and have stayed in the ward for two or more days. Exclusion criteria included patients who did not consent to participate, those who had stayed in the ward for less than two days, patients in a comatose state or with critical illness, and those with cognitive impairment affecting judgment or communication.
Given the fluctuating population size, convenient sampling was employed, resulting in a sample size of 53 participants.
RESULTS
Demographic Factors
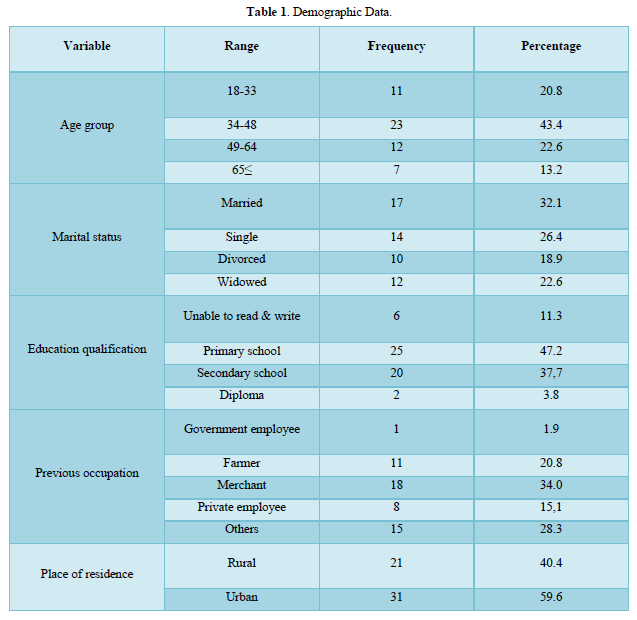
A total of 53 adult medical and surgical palliative patients were approached and 99.8% (n=53) fully filled questionnaires with incomplete response rate of 0.2%. Most of the participants were: male (56.6%), age group of between 34 and 48 with mean age of 41 years (43.4%) Most participants were married (32.1%), merchant as their previous occupation (34.0%), and had attended only primary education (47.2%), most participants live in urban area (58.6%). Most of participants were admitted in medical ward (50.9%), spent more than one year in the hospital (47.1%), were hospitalized more than two times (45.3%), had other disease(s) in addition to current health problem (58.5%) and (96.2%) were admitted in common room (Table 1).

Hospitalization Data
Most of participants were admitted in medical ward 27(50.9%), have stayed in the hospital for years 24(47.1%), has been hospitalized for more than two times 24(45.3%). Most of them have other diseases in addition to current one 31(58.5%), were admitted in common room 51(96.2%), most of them have family support/companion possession 35(66.0%).
Patients Expectations from Nursing Communication
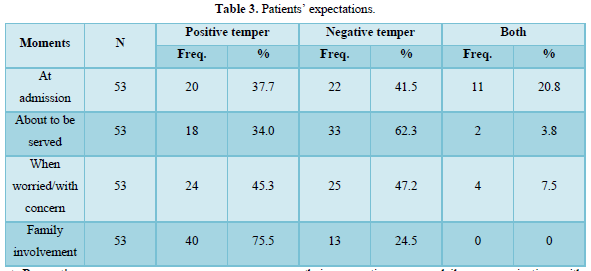
Almost in all moments, the findings indicate that most of participants expected negative expressions and negative responses whereby at the time of admission, when patient was ready to be served and when patient had worries/concerns, majority of participants 22(41.5%), 33(62.3) and 25(47.2) respectively, had negative expectations except when it cames to the family involvement here most of participants expected positive outcomes.
The Table 3 below shows participants’ responses on their expectations from their communication with nurses.
Patients Perceptions
In almost all characteristics, participants perceived nurses negatively as it is systematically mentioned in the chart. The characteristic with long peak is the response of the majority. The chart below properly displays participants’ responses on their perceptions upon daily communication with their nurses in nursing palliative care.
As it is mentioned in Figure 1, among the population of 53 participants, the majority agreed that nurses never welcome palliative patients at admission 25(47.2%), rarely inform patients on procedure or treatment to be done and rarely ask for permission 20(37.7%), rarely maintain individual respect 17(32.7), sometimes express willingness to help when asked 26(49.1%), sometimes give patients opportunity to express their worries and concerns 21(39.6%), rarely listen to patients carefully 20(37.7%), never interrupt patient while speaking 23(43.4%), patients sometimes feel like not understood 29(54.7%), rarely cares and reply to patients’ questions 28(52.8%), are always responsible for their communication with patients 39(73.6%), never communicate friendly with patients 24(45.3%), sometimes it is easy for patients to understand what nurses say 20(37.7%), rarely spend enough time with patients 25(47.2%), never provide enough information 19(35.8%), are rarely knowledgeable 22(41.5%), never explains drug indications and its side effects 41(77.4%), patients are rarely informed on danger signs of illness to watch out 18(34.0%), nurses never show contradictions among them 24(45.3), nurses do not (never) involve family in patient care 24(45.3%).

Patients’ Satisfaction
Respondents did their own rating basing on the way they perceive their communication with nurses. As it is illustrated in Figure 2, among 53 respondents, 6(11.3%) their satisfaction was below 25%; 21(39.6%) their satisfaction was between 26% - 50%; 16(30.2%) their satisfaction was between 51%-75% then finally 10(18.9%) their satisfaction was above 76%.

DISCUSSION
This study is particularly unique in its focus on evaluating nurse-patient communication from the perspective of patient expectations, perceptions, and satisfaction in the context of nursing palliative care. While numerous studies globally have explored nurse-patient communication, few have delved into the specific impact of patients' expectations and perceptions on their satisfaction with communication.
By examining patients' expectations upon admission and comparing them with their perceptions after experiencing nurse-patient communication, this study provides valuable insights into how these factors influence patient satisfaction. Understanding patients' perspectives is essential for optimizing communication practices and enhancing the quality of care provided.
The discussion of the study findings likely drew upon existing literature in the field and was guided by the research objectives. By synthesizing the study results with relevant theoretical frameworks and previous research findings, the discussion would have provided a deeper understanding of the implications of the findings and their significance in the broader context of healthcare communication.
From research findings, patients’ expectations with nurse-patient communication in Kibogora level 2 Hospital, it was found that more patients expected negative temper than positive. On admission, respondents (41.5%) expected just to be shown the bed and leave, no welcoming, no orientation or explaining the reason for Cleary admission due to the reason If the patients have had bad times with nurses, no way they could expect positive output from nurses. Almost the same as the findings from 2017 study conducted in UK whereby participants replied that “I expected to be in and out in sort of a minute rather than, “I was quite pleased because they done everything thoroughly so you know. I didn’t expect them to be saying what they did” [26]. These findings are also highly supported by the study conducted in Australia that was looking for patients’ experiences in Australian hospital. It revealed that there is a great impact of patient’s hospital experience to his/her expectations at future admissions [27,28]. At the time actual care/ nursing procedure when the patient was ready to be served, patients expected (62.3%) only being served immediately without being told nurse’s name, being asked for permission or being explained the procedure and need for care. Contrary, more than half of the patients (58%) in the university hospital and 42% of the patients in the state hospital expected greetings, concern, understanding and benevolence from the nurses, most of the patients (90%) expected that their nurses would pay attention to them in order to relieve their pain [27]. At the time when patient was worried or having a certain concern by which he wished to express, the majority of respondents (47.2%) expected carelessness and rude expressions of the nurses whereas (45.3) expected nurses to listen to them carefully and offering psychological and emotional support. Contrary, in Ethiopia, participants’ expectations of nursing care were found to be kind, understanding, concern and benevolent due to the experience [20]. These expectations of nursing care were not related to the nurse’s knowledge and competence. In addition, patients expected just to be informed by the nurses about their medication and treatment [20].Patients perceived the quality of their communication with nurses depending on various aspects such as: being welcomed on admission, informed consent before each nursing intervention, maintaining individual respect, exhibition of willingness to help once asked, offering opportunities for patients to express worries, careful listening, whether nurses interrupt during conversation or whether they care and reply to patients, spending enough time with patients as well as providing adequate information regarding illness and treatment. At each of the above aspects, respondents gave their views of the way it goes in medical and surgical ward at Kibogora Level 2 Teaching hospital as it is well illustrated in the Table 3 and its corresponding chart. Briefly, the results of this assessment are neither pleasant nor enjoyable.
45.3% of respondents responded that nurses never communicate friendly but only 5.7% said that they do, the same as the findings from the study done in Hiwot Fana specialized University Hospital about patients’ expectation strongly associated with patients’ perception to nursing care, it found poor perception (54.8%). Whereas most of participants in the study done in UK on patient expectations of first contact care consultations with nurse and general practitioners responded that on first contact, they had good interaction with nurses. They said “she went into a lot more detail than I thought she was going to …. I expected to be in and out in sort of a minute rather than, I think it took about ten or twelve minutes. I didn’t expect her to listen to my chest properly during nurse consultation.”; “I was quite pleased because they done everything thoroughly so you know. I didn’t expect them to be saying what they did. But once they got the issues out of the way sort of thing during nurse consultation, they just gave me right information” [26].
Some participants (37.7%) wished that as they stay longer, they would develop a stronger relationship with the nurses and hence able to communicate their needs and wishes more freely. Contrary, only 3.8% of respondents responded that nurses always allow patients to express their concern and worries, whereas other 30.2% responded that nurses never allow patients to express their worries and concern only 9.4% of nurses always express willingness to help. The results of this study suggest that length of hospital stay and patient disease condition influence patients’ perception of communication with nurse whereby the longer patients stayed in palliative care at the hospital; the more they had poor perception as evidenced by a reaction patient had when asked, he said “ this is my third year lying on this hospital’s bed, I know the attitudes and names of each and every nurse who attends this ward even though I can count on my finger the number of times when they tried to ask me how I feel”. These results are opposite to the findings from studies conducted in Germany by Stefan Köberich, Johanna and Erik Farin (2016) and in Turkey by Dilek and Dikmen (2016) [29]. They found that the longer patients stayed, the more individualized than those whose stay was shorter. Köberich and his colleagues suggested that a patient discharged early worries about continuity of his care or lacks information about self-care behavior at home [29,30].
Respondents were asked to do general evaluation of their communication with nurses and base on that in order to rate their own level of satisfaction. As it illustrated in Table 4, among 53 respondents, 49% had satisfaction level which is below 50% whereas 51% respondents had satisfaction level of above 50%. The level of patient satisfaction was low. The same in Ethiopia that of the total respondents, only 52.5% of them were found to be satisfied with general nursing care [31] and another study again from Ethiopia found that only 49.2% were satisfied with nursing care [4]. Contrary to the study conducted at a large University Hospital in Switzerland which revealed that satisfaction levels were high even though the author did not define the precise level but mentioned that patients with private insurance generally rated their satisfaction as being slightly higher [32].
CONCLUSION
The results highlight the critical role of effective communication in addressing the complex needs of patients in medical and surgical wards. However, many patients reported poor perceptions of nursing communication, often citing negative experiences such as a lack of courtesy, failure to introduce themselves, insufficient explanations about treatments, and substandard care environments. These shortcomings point to clear areas for improvement in nurse patient interactions. Enhancing communication through empathy, clarity, and patient-centered approaches is essential for improving patient satisfaction and care quality. Furthermore, improving nurses’ working conditions may support more meaningful and consistent patient engagement.
- Boggs EAK (2019) Professional Communication Skills for Nurses (8th). Saunders.
- Dithole KS, Thupayagale-Tshweneagae G, Akpor OA, Moleki MM (2017) Communication skills intervention: Promoting effective communication between nurses and mechanically ventilated patients. BMC Nurs 16(1): 1-6.
- Terrill AL, Ellington L, John KK, Latimer S, Xu J, et al. (2019) Positive emotion communication: Fostering well-being at end of life. Patient Educ Couns 101(4): 631-638.
- Sharew NT, Bizuneh HT, Assefa HK, Habtewold TD (2018) Investigating admitted patients’ satisfaction with nursing care at Debre Berhan Referral Hospital in Ethiopia: A cross-sectional study. BMJ Open 8(5): 1-8.
- Aiken LH, Sloane DM, Ball J, Bruyneel L, Rafferty AM, et al. (2018) Patient satisfaction with hospital care and nurses in England: An observational study. BMJ Open 8(1): 1-8.
- Holm A, Dreyer P (2018) Nurse-patient communication within the context of non-sedated mechanical ventilation: A hermeneutic-phenomenological study. Nurs Crit Care 23(2): 88-94.
- Smith LRJSM (2019) Effective Communication.
- Nilsen ML, Sereika SM, Hoffman LA, Barnato A, Donovan H, et al. (2014) Nurse and patient interaction behaviors’ effects on nursing care quality for mechanically ventilated older adults in the ICU. Res Gerontol Nurs 7(3): 113-125.
- Sibiya MN (2018) Effective Communication in Nursing.
- Fang J, Liu L, Fang P (2019) What is the most important factor affecting patient satisfaction-A study based on gamma coefficient. Patient Prefer Adher 13: 515-525.
- Kraska RA, Weigand M, Geraedts M (2017) Associations between hospital characteristics and patient satisfaction in Germany. Health Expect 20(4): 593-600.
- Omorogbe CE, Amiegheme FE (2016) Nurses’ communication and patient satisfaction in a tertiary hospital in Benin City, Nigeria. J Med Biomed Res 15(2): 47-56.
- Kargar Jahromi M, Ramezanli S (2014) Evaluation of barriers contributing in the demonstration of an effective nurse-patient communication in educational hospitals of Jahrom, 2014. Global J Health Sci 6(6): 54-60.
- Heidari M, Pour H, Norouzzadeh R, Temel E, Şahin B (2017) Assessment Patients’ Satisfaction Related on Quality of Care: A Cross-sectional Descriptive Study. Asian J Med Health 5(4): 1-8.
- Lotfi M, Zamanzadeh V, Valizadeh L, Khajehgoodari M (2019) Assessment of nurse–patient communication and patient satisfaction from nursing care. Nurs Open 6(3): 1189-1196.
- Dudo A, Besley JC (2016) Scientists’ prioritization of communication objectives for public engagement. PLoS One 11(2): 1-18.
- Pun JKH, Matthiessen CMIM, Murray KA, Slade D (2015) Factors affecting communication in emergency departments: doctors and nurses’ perceptions of communication in a trilingual ED in Hong Kong. Int J Emerg Med 8(1): 1-12.
- Sekse RJT, Hunskår I, Ellingsen S (2018) The nurse’s role in palliative care: A qualitative meta-synthesis. J Clin Nurs 27(1-2): e21-e38.
- Lam WWT, Kwong A, Suen D, Tsang J, Soong I, et al. (2018) Factors predicting patient satisfaction in women with advanced breast cancer: A prospective study. BMC Cancer 18(1): 1-7.
- Girmay A, Marye T, Haftu M, Dawit G, Brhanu T, et al. (2018) Patients expectation strongly associated with patients perception to nursing care : hospital based cross sectional study. BMC Res Notes pp: 1-6.
- Adigwe P, Okoro E (2016) Human Communication and Effective Interpersonal Relationships: An Analysis of Client Counseling and Emotional Stability. Int J Econ Manag Sci 05(03): 3-6.
- Kleefstra SM, Zandbelt LC, De Haes HJ, Kool RB (2015)Trends in patient satisfaction in Dutch university medical centers: Room for improvement for all. BMC Health Serv Res 15(1): 1-9.
- Cubaka VK, Schriver M, Kayitare JB, Cotton P, Maindal HT, et al. (2018) He should feel your pain’: Patient insights on patient-provider communication in Rwanda. African J Primary Health Care Family Medicine pp: 1-11.
- Alshammari M, Duff J, Guilhermino M (2019) Barriers to nurse-patient communication in Saudi Arabia: An integrative review. BMC Nurs 18(1): 1-10.
- Will KK, Johnson ML, Lamb G (2019) Team-Based Care and Patient Satisfaction in the Hospital Setting: A Systematic Review. J Patient Cent Res Rev 6(2): 158-171.
- Redsell S, Jackson C, Stkoes T, Hastings A, Baker R (2017) Patient expectations of “first-contact care” consultations with nurse and general practitioners in primary care. 15: 5-10.
- Chan EA, Wong F, Cheung MY, Lam W (2018) Patients’ perceptions of their experiences with nurse-patient communication in oncology settings: A focused ethnographic study. PLoS One 13(6): 1-17.
- Check AE (2015) Patients’ experiences in Australian hospitals.
- Dikmen Y, Yılmaz D (2016) Patient’s Perceptions of Nursing Care-A Descriptive Study from Turkey. Ann Nurs Pract 3(3): 1-5.
- Köberich S, Feuchtinger J, Farin E (2016) Factors influencing hospitalized patients’ perception of individualized nursing care: A cross-sectional study. BMC Nurs 15(1): 1-11.
- Haile Eyasu K, Adane AA, Amdie FZ, Getahun TB, Biwota MA (2016) Adult Patients’ Satisfaction with Inpatient Nursing Care and Associated Factors in an Ethiopian Referral Hospital, Northeast, Ethiopia. Adv Nurs 2016: 1-7.
- Pelletier D, Green-Demers I, Collerette P, Heberer M (2019) Modeling the communication-satisfaction relationship in hospital patients. SAGE Open Med 7: 205031211984792.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Journal of Spine Diseases
- Journal of Alcoholism Clinical Research
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Ophthalmology Clinics and Research (ISSN:2638-115X)




