1038
Views & Citations38
Likes & Shares
Lipomas of GI tract are rare tumors and even rarer in stomach. In this location they grow to large sizes and present as upper gastrointestinal bleeding. We present a similar case of a 15year old boy who presented with massive upper GI bleed and was diagnosed to have a submucosal gastric lipoma in the body of stomach on CT. Laparotomy with gastrotomy and enucleation of a giant 13.5 cm lipoma with primary closure of the stomach was done. Post-operative recovery was uneventful. Giant lipomas are rare in literature and enucleation with preservation of stomach is an acceptable modality in these cases.
At gastric location these mechanisms are rare and they grow much larger in size causing symptoms. Massive upper gastrointestinal hemorrhage has been reported in many cases especially in these giant lipomas where the blood supply of the overlying mucosa becomes tenuous and ischemic ulcers forms [2]. Cross sectional imaging confirms the diagnosis with characteristic features and the surgical intervention results in cure. Malignancy in gastric lipoma has not been reported and enucleation of the tumor is sufficient [3].
We present a similar case of 15year old boy who presented to us with massive upper gastrointestinal bleed and upper GI endoscopy and CT abdomen were rapidly able clinch the diagnoses of a giant gastric lipoma in the body of stomach. Patient underwent laparotomy with enucleation of the tumor, excision of redundant serosa and adherent mucosa with primary closure thus preventing a gastrectomy in a giant lipoma. This case report reviews the literature and highlights the fact that enucleation can easily be achieved in giant gastric lipomas preserving the stomach with excellent outcomes and low morbidity especially where the patient has suffered a massive upper GI bleed which is a common scenario with giant gastric lipomas.
CASE IN MENTION
A 15year old young boy with no comorbidities presented to our institute with sudden onset massive hematemesis on 2/4/2019. Patient had consequent 2-3 episodes of hematemesis, each consisting of basin full of fresh blood and clots; within the past 2 days and had a single episode of malena. No history of trauma, blood transfusion, loss of appetite, early satiety, epigastric fullness, weakness or previous similar episode was elicited. On evaluation patient was conscious, afebrile with tachycardia of 110 and stable blood pressure 100/ 60 mm hg. Patient had deep tenderness in the epigastrium. Patient had low hemoglobin of 5.8 and raised transaminases(440/300-AST/ALT) and alkaline phosphatases (180) with preserved renal function and coagulation parameters. Patient was managed conservatively with blood transfusions (total 2), IV fluids, nil per oral and was evaluated with early endoscopy. Endoscopy revealed a large adherent clot in the stomach associated with a 5-6 cm subepithelial lesion in the body of stomach with surface ulceration. No active bleed was visualized. The patient improved clinically, hematemesis subsided and the hemoglobin levels were stable over the period of 2 days (Figures 1 & 2).


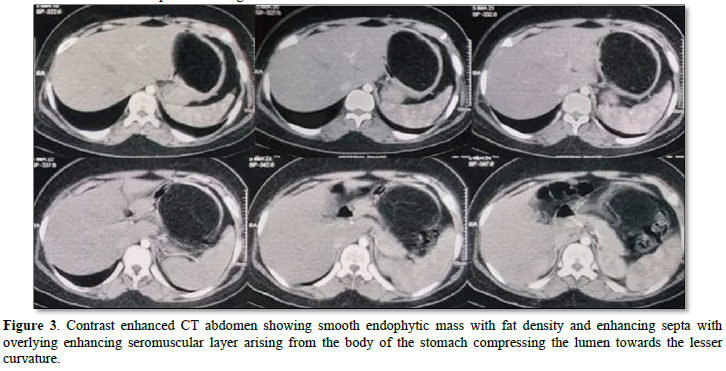
CECT abdomen revealed a large hypoattenuating, non-enhancing mass arising from the posterior wall of the stomach with ill-defined septa and having Hounsfield unit in the range of -110 to -120 thus essentially confirming the diagnosis of a gastric lipoma (Figure 3).
 After preoperative optimization the patient underwent midline laparotomy. The bulge in the posterior wall of the stomach was visualized after entering the lesser sac and gastrotomy was made at the edge of the mass where it was adherent to the stomach wall. The stomach lumen was empty; a well-defined punched out ulcer of ~1cm at the upper end of the mucosal surface of the lesion was present. The submucosal plane was entered and the lipoma was discovered and enucleation was initiated. At multiple places the lipoma was densely adhered to the overlying mucosa in view of ischemic changes. An ellipse of mucosa along with the lipoma and serosa was excised in view of the large size of the tumor (Figures 4 & 5) A 13 * 10 cm lipoma was enucleated along with an ellipse of adherent mucosa and the redundant serosal layer was trimmed and refashioned.
After preoperative optimization the patient underwent midline laparotomy. The bulge in the posterior wall of the stomach was visualized after entering the lesser sac and gastrotomy was made at the edge of the mass where it was adherent to the stomach wall. The stomach lumen was empty; a well-defined punched out ulcer of ~1cm at the upper end of the mucosal surface of the lesion was present. The submucosal plane was entered and the lipoma was discovered and enucleation was initiated. At multiple places the lipoma was densely adhered to the overlying mucosa in view of ischemic changes. An ellipse of mucosa along with the lipoma and serosa was excised in view of the large size of the tumor (Figures 4 & 5) A 13 * 10 cm lipoma was enucleated along with an ellipse of adherent mucosa and the redundant serosal layer was trimmed and refashioned.
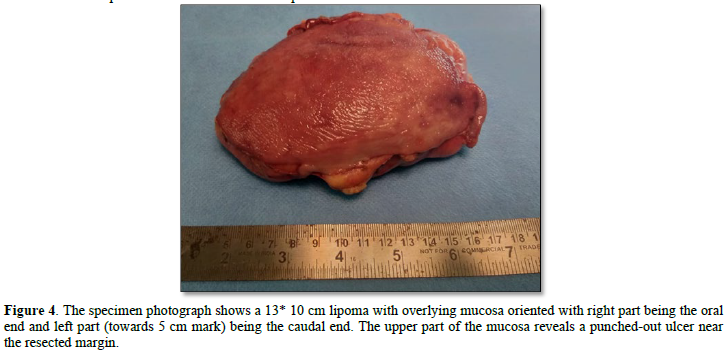
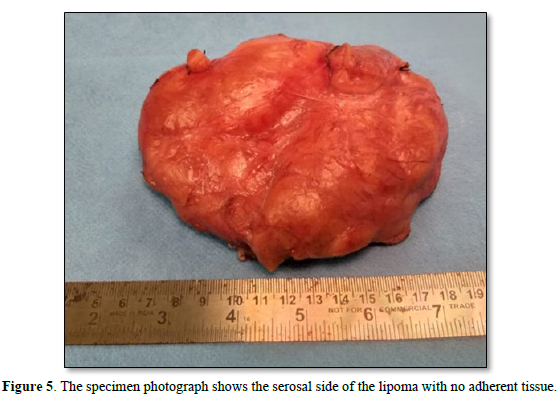
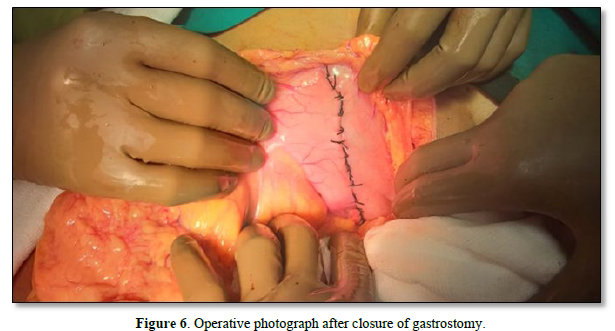
The resultant defect was closed in 2 layers and abdominal closure was done (Figure 6). No intraabdominal drains were placed. Post-operative period was uneventful with Ryles tube being removed on postoperative day 3 oral diet being resumed on post-operative day 4 and patient discharged on postoperative day 5. Biopsy revealed a 13.5 X 9 X 5 cm submucosal lipoma consisting of mature adipocytes with no evidence of dysplasia.
 DISCUSSION
DISCUSSION
Lipomas of the gastrointestinal tract are rare, occur most commonly in colon and are usually solitary. Stomach as a site for lipoma comes after colon and small bowel with around 5% of GI lipomas occurring at this site. These are mainly found in the 5th to 6th decade age group with preponderance to female gender [1]. The presented case depicts the other end of the spectrum with a large gastric lipoma in a young male boy and similarly limited pediatric cases are present in the literature [4,5].
They produce symptoms based on their size and location. Most commonly they are present in the submucosal location and are very rarely found in the subserosal location with a single case report in literature of one being symptomatic and surgically managed [2]. The submucosal lipomas are subjected to inward push by regular contractions in the muscularis layer. With small bowel they commonly cause intussuseption and pain even with smaller sizes. In colon they commonly present as pedunculated polyps where the normal mucosa forms the stalk after prolonged elongation. Generally, in stomach they grow in size and stretching the mucosa and causing ischemic ulcers and bleeding. Other mechanisms including polyp formation and gastric outlet obstruction have also been reported [6]. This phenomenon of increased size and bleeding is also found in other GI tract lipomas when size starts to exceed more than 2 cms. Bleeding is rarely massive but has been reported in literature as case reports in gastric lipomas similar to this case [4]. Gastric lipomas tend to increase in size and generally range up to 2-6 cms. Giant gastric lipomas have been described as more than 8 cm in size by some authors [7] and more than 10 by other [8] and thus have reported 12 giant lipomas and 6 giant lipomas respectively in literature; largest being around 18 cms. These are most commonly present at the antral region. We feel the presentation and mechanism of ulcer formation was typical as described in literature in form of a giant 13.5 gastric lipoma causing mucosal ulceration and massive upper gastrointestinal bleed with having no previous history of recurrent pain or early satiety.
With increased advancements in imaging many of these are detected incidentally and diagnosed small, asymptomatic lipomas are not considered for surgical intervention. Symptomatic lipomas on other hand require intervention and thus establishing diagnosis preoperatively is helpful to plan surgery. Earlier the role of rectal and oral contrast studies was well established with multiple signs described in literature especially for colonic polyps [9]. With the increased availability and use of CT and MRI, cross sectional imaging-based signs are more specific in establishing the diagnosis. CT establishes the site and size of the tumor with comments upon local invasion, preserved planes and presence or absence of lymphadenectomy which acts as surrogate markers for establishing the diagnosis. Most important is the attenuation of the tumor which lies in the range of -80HU and -120HU in view of high fat content and clinches the diagnosis of a lipoma. Septations can also been seen it CT. In general MRI is the modality of choice in diagnosing lipomas depicting high signal intensity on T1 weighted sequences typical of a lipoma, with higher sensitivities and specificities and better comment on possible lipo sarcomatous elements. But in the scenario of gastrointestinal, and more so for gastric lipomas MRI use has been rare in the literature [10]. Also, malignant changes in gastric lipoma have never been reported, though associated synchronous malignancies in gastrointestinal lipomas at other sites have been reported [11].
Upper GI endoscopy usually depicts well defined signs such as tenting sign, the naked fat sign, and the cushion sign. But these are not very specific and the lesion might be confused with GIST. Endoscopic biopsies might or might not help as the lesion in commonly submucosal. In view of these findings the role of endoscopic ultrasound comes into play and Intensely hyperechoic, homogeneous, well-circumscribed lesions arising from the 3rd layer are characteristic features of a gastric lipoma and requires no further investigations for diagnosis if present [12,13]. In our case endoscopy was doubtful for a GIST owing to its much more frequent prevalence at our institute in form of a submucosal tumor presenting with upper GI bleed. Generally, these cases go EUS examination with FNAC but in view of severity of presentation and chance of hemodynamic instability a quick early endoscopy and CT abdomen was performed and as CT clinched the diagnoses EUS was not deemed necessary.
In view of their benign nature, enucleation of these gastric lipomas is a well-accepted surgical treatment and has been well documented in literature in form of case reports [3]. Cases where preoperative diagnosis is not clear and resecting a specimen would not result in added morbidity, resection is also acceptable as in small bowel and colonic lipomas. But in case of gastric lipomas where they reach massive sizes and comparison of morbidity of a gastrectomy and enucleation is not equivalent; enucleation seems to be a valid alternative. Most of the case reports mention resection as their treatment modality [5], but this is perhaps in view of their size which requires excision of serosa and resection of adhered mucosa as done in this case and hence terming it as resection rather than enucleation. For smaller sized lipoma (~2cm) endoscopic polypectomy is an acceptable treatment and even larger size lipomas upto 6cm can well treated with a laparoscopic approach [13,14]. We similarly were able to preserve the lesser curvature of the stomach in this process and prevented a gastrectomy which has both short term and long-term implications especially in a pediatric case; where lifelong issues related to biliary reflux, stomal ulceration and chances of malignancy ensues. For a well-established benign lesion like gastric lipoma, where possible enucleation should be attempted with preservation of the stomach.
CONFLICT OF INTEREST
None declared.
- Fernandez MJ (1983) Gastrointestinal Lipomas. Arch Surg 118: 1081.
- Krasniqi AS, Hoxha FT, Bicaj BX, Hashani SI, Hasimja SM, et al. (2008) Symptomatic subserosal gastric lipoma successfully treated with enucleation. World J Gastroenterol 14 (38): 5930-5932.
- Termos S, Reslan O, Alqabandi O, AlDuwaisan A, Al-Subaie S, et al. (2017) Giant gastric lipoma presenting as GI bleed: Enucleation or Resection? Int J Surg Case Rep 41: 39-42.
- Ramdass MJ, Mathur S, Seetahal-Maraj P, Barrow S (2013) Gastric Lipoma Presenting with Massive Upper Gastrointestinal Bleeding. Case Rep Emerg Med 2013: 1-3.
- Kanojia R, Rao KLN, Menon P, Zameer M, Samujh R, et al. (2010) Gastric lipoma. J Indian Assoc Pediatr Surg 15(2): 64-66.
- Pandey MK, Priyadarshi RN, Anand U, Chaudhary B, Kumar R (2015) Giant Gastric Lipoma Presenting as Gastric Outlet Obstruction-A Case Report. J Clin Diagn Res 9(10): PD03- PD034.
- Cappell MS, Stevens CE, Amin M (2017) Systematic review of giant gastric lipomas reported since 1980 and report of two new cases in a review of 117110 esophagogastroduodenoscopies. World J Gastroenterol 23(30): 5619-5633.
- Amundson JR, Straus D, Azab B, Liu S, Buitrago MGT, et al. (2018) Giant symptomatic gastric lipoma: A case report and literature review. Int J Surg Case Rep 51: 313-317.
- Taylor AJ, Stewart ET, Dodds WJ (1990) Gastrointestinal lipomas: A radiologic and pathologic review. Am J Roentgenol 155: 1205-1210.
- Thompson WM (2005) Imaging and Findings of Lipomas of the Gastrointestinal Tract. Am J Roentgenol 184: 1163-1171.
- Siegal A, Witz M (1991) Gastrointestinal lipoma and malignancies. J Surg Oncol 47: 170-174.
- Gong EJ, Kim DH (2016) Endoscopic Ultrasonography in the Diagnosis of Gastric Subepithelial Lesions. Clin Endosc 49: 425-433.
- Suekane H, Iida M, Yao T, Matsumoto T, Masuda Y, et al. (1993) Endoscopic ultrasonography in primary gastric lymphoma: Correlation with endoscopic and histologic findings. Gastrointest Endosc 39(2): 139-145.
- Lacy AM, Tabet J, Grande L, Fuster J, Visa J, et al. (1995) Laparoscopic-assisted resection of a gastric lipoma. Surg Endosc 9(9): 995-997.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns








