10757
Views & Citations9757
Likes & Shares
Material and Methods: A review of recent literature published between 2015 and 2024 was conducted, focusing on high-evidence articles related to tissue expansion.
Conclusion: Tissue expansion, now combined with innovative strategies, yields improved results. Success depends on comprehensive patient management.
Keywords: Tissue expansion, Innovation, Tissue, Diagnosis, Treatment, Complications, Reconstructive surgery
Radova and Austad pioneered the modern use of tissue expansion [2]. The primary goal of tissue expansion is to obtain additional tissue that matches the original in quality and quantity (color, texture, hair growth, sensory quality) with minimal donor site morbidity [3]. The advantages and disadvantages of tissue expansion are outlined in Table 1. Key factors include mechanical creep, biological creep, and stress reduction [4].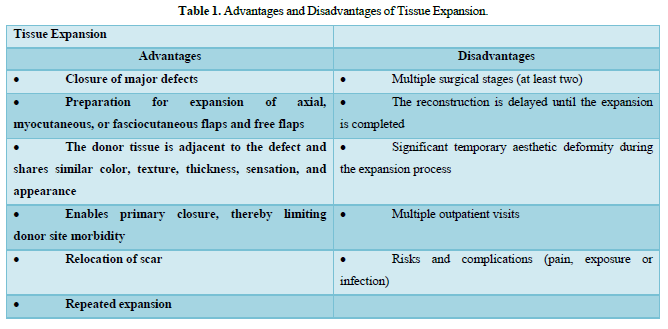
Mechanical Cree: This occurs when tissue is acutely stretched, resulting in collagen fiber alignment, micro-fragmentation of elastic fibers, and redistribution of water within the tissue's elastic fibers [5] (Figure 1).

Biological Creep: This occurs with chronic stretching, initiating cellular growth and tissue regeneration, increased collagen production, angiogenesis, and activation of growth factors and kinases.
Understanding the tissue expansion process offers a practical guide based on scientific research.
MATERIALS AND METHODS
The force required to maintain tissue elongation decreases over time [5]. Applying a constant force for a certain period reduces tissue resistance, increasing the amount of expanded tissue and requiring less force (stress force) to continue the process. Gradual force application is crucial to avoid altering tissue elasticity patterns and causing quality alterations (striae, tissue thinning) or rupture, which could expose the expander. The biological effects of tissue expansion are observed at the epidermis, dermis, muscle, fat, capsule, and blood vessel levels (Table 2). Mechanical stretching and biological growth occur during tissue expansion, reaching histological normality up to two years post-expander removal [6,7].

Expanders are silicone balloons molded into preformed prostheses, filled with saline solution through an integrated or remote port. Tissue expanders are classified based on shape into non-differential, differential, and customized. Standard tissue expanders (non-differential) are generally circular, rectangular, or crescent-shaped (Figure 2).

Differential expanders produce more expansion in specific parts. Customized expanders are tailored for specific defects [8]. Rectangular expanders gain 38% of the calculated expander surface area, round expanders gain 25%, and crescent expanders gain 32% [9].
PLANNING THE EXPANSION
This is a complex process involving a multidisciplinary team and family support. Emotional stability is crucial due to temporary aesthetic disfigurement. There are absolute and relative contraindications for expander use (Table 3). Size, shape, and volume selection must consider defect size, donor site, and expected flap advancement [10]. Several theories exist for choosing an expander; one suggests the expander's base should match the defect size. However, the expander's base should ideally be 2.5-3 times the defect width [11,12] (Figures 3 & 4). To estimate the tissue needed, use: defect area + expander area + 20%.



AREA "A" AND "C": SIDE 1 X HEIGHT AREA "B" AND "D": SIDE 2 X HEIGHT
Surgical Technique
The incision should be perpendicular to the expansion direction to avoid tension and possible dehiscence during expansion. It can be made in previous scars or at the defect edge [10] (Figure 5). The pocket's size should match the expander's size to avoid deformation or displacement. Hemostasis and meticulous dissection preserve overlying vascularization. Closed drains combat dead space [13-15]. The expander is partially filled (10-20% capacity) for proper positioning. Expansion typically starts 2 to 3 weeks post-placement [3].

Expansion is performed on an outpatient basis, usually without anesthesia. The area is examined for inflammation and sensitivity. The expander and valve are palpated for folds and accessibility [16]. After cleaning and preparation, the valve is located with a magnetic device, and the dome is pierced with a syringe. Gentle aspiration confirms system continuity. Expansion is done with 0.9% saline, avoiding air introduction [17]. Each session's volume is recorded. Expansion lasts 6 to 12 weeks, after which the expander is removed and the final reconstruction is performed [18] (Figure 6). The formed capsule is dissected perpendicular to the advancement direction to increase flap mobilization.
Complete capsule removal is generally unnecessary and potentially harmful [19,12].

APPLICATIONS BY ANATOMICAL REGION
Scalp: Approximately 50% of the scalp can be reconstructed without significant thinning of the remaining hair.
Location: Subcutaneous or subgaleal plane.
Duration: Expansion can occur 2-3 times per week [20].
Considerations: Incisions are camouflaged in the hairline, eyebrow line, midline, or tension lines.
Head and Neck: Flaps are designed considering vessel branches. Special care must be taken with aesthetic units and flap tension.
Location: Subcutaneous plane, superficial to SMAS. In the neck, the expander can be placed superficial or deep to the platysma [18].
Considerations: Avoid facial nerve branches and Stenon duct [21].
Ears: Used for microtia corrections and auricular wound coverage.
Location: Respect the superficial temporal fascia in the supra- and preauricular region [22].
Considerations: Typically involves three stages: 1. Expander placement, 2. Expander removal, 3. Auricular remnants and scar remodeling.
Chest and Breast: Thoracic and abdominal defects are better managed with multiple expanders.
Location: Submuscular plane (pectoralis major), with inferolateral pole covered by serratus anterior fascia [23].
Considerations: Respect the nipple-areola complex (NAC). In radiated tissues, complications include infection and extrusion [24].
Abdomen: Advantages include low neurovascular damage risk and better expansion potential.
Location: Plane between internal and external obliques. Duration: 4 weeks to 3 months.
Considerations: Avoid pressures exceeding 30-40 cmH2O to prevent complications like abdominal compartment syndrome [25].
Extremities: Expansion is associated with higher complication rates, requiring careful technique selection.
Location: Supramuscular plane.
Considerations: Avoid superficial vessels or sensory nerves. The expander should not cross or interfere with joint mobility.
COMPLICATIONS
The success rate of tissue expansion ranges from 84-97%. However, complications can occur, related to the expander, the patient, or the surgical technique (Table 4). Factors associated with these complications include improper expander selection, inadequate patient evaluation, and technical errors during the expansion process. Common complications are hematoma, infection, exposure, and extrusion. To mitigate these risks, careful planning, meticulous surgical technique, and diligent postoperative care are imperative.

Unfavorable Results and Complications: Tissue expansion is a multi-stage process that necessitates careful patient selection, meticulous planning, precise execution with attention to detail, sterile techniques, and three-dimensional skin movement throughout the treatment course. Due to these complexities, certain complications and unfavorable outcomes may arise during the process. Complications can occur during the insertion of the expander, after its placement, during the tissue expansion period, and at the time of its removal. Therefore, special attention is required throughout this procedure [10].
TISSUE EXPANSION AND CURRENT ADVANCES
In recent years, tissue expansion has seen several improvements, including new expansion systems, optimization of the expansion process, and reduction of radiation effects through fat grafting and neoformation of fat tissue post-expansion.
The CO2 expander system, already FDA-approved, allows patients to control their expansion safely and conveniently without punctures and remotely, with minimal clinic visits. This system is primarily used for breast reconstruction [2].
Regarding tissue expansion and fat, experimental and clinical studies have demonstrated that tissue expansion has positive effects on fat tissue. Rigotti et al. showed that creating internal tensile force through an expander induces the proliferation of newly formed adipose tissue, both by the tensile force generated by the expander and by pro-adipogenic factors contained in the edema generated during the expansion process [29]. He et al. demonstrated that dissection of fat tissue prior to the placement of the negative pressure expander increases contact between adipocytes and induces the proliferation of adipose-derived stem cells. These stem cells undergo adipogenesis in the adipogenic environment created by external volume expansion, leading to better adipose regeneration.
Using expansion to prepare perforator flaps is a novel technique to shape the tissue according to specific needs. Reconstruction with pre-expanded flaps is one of the highest rungs of the reconstructive ladder. Expanded flaps are preferred over non-expanded perforator flaps for four main reasons: larger flap size, thinner flap, smaller donor site scar and deformity, and a more reliable flap.
CONCLUSION
Tissue expansion is a valuable tool within the reconstructive arsenal. It requires proper patient selection, meticulous planning, and precise execution at each stage, generating gratifying outcomes by enabling the reconstruction of complex lesions and defects resulting from trauma and congenital anomalies. Currently, tissue expansion has been combined with various innovative strategies to achieve better results. The success of tissue expansion depends on comprehensive patient management, care provided throughout the process, and the support of the patient’s family network to optimize results.
- Gosain AK, Turin SY, Chim H, LoGiudice JA (2018) Salvaging the Unavoidable: A Review of Complications in Pediatric Tissue Expansion. Plast Reconstr Surg 142(3): 759-768.
- Morrison KA, Ascherman BM, Ascherman JA (2017) Evolving Approaches to Tissue Expander Design and Plast Reconstr Surg 140: 23S-29S.
- Lee H, Eom Y, Oh KS (2019) Management of Congenital Melanocytic Nevus on Face Using Multiple Re-expansion Method: Aesthetic and Psychosocial J Craniofac Surg 30(8): 2385-2389.
- Yu Z, Liu S, Cui J, Song Y, Wang T, et (2020) Early histological and ultrastructural changes in expanded murine scalp. Ultrastruct Pathol 44(1): 141-52.
- Lee T, Vaca EE, Ledwon JK, Bae H, Topczewska JM, et (2018) Improving tissue expansion protocols through computational modeling [Internet]. J Mech Behav Biomed Mater 82: 224-234.
- Lujan-Hernandez J, Chin MS, Perry DJ, Chappell A, Lancerotto L, et (2020) N Increasing Fat Graft Retention in Irradiated Tissue after Preconditioning with External Volume Expansion. Plast Reconstr Surg 145(1): 103-112.
- Arain AR, Cole K, Sullivan C, Banerjee S, Kazley J, et al. (2018) Tissue expanders with a focus on extremity reconstruction. Expert Rev Med Devices 15(2): 145-155.
- Durgun M, Aksam E (2019) Choosing the right rectangular expander and maximizing the benefits from expanded tissue [Internet] J Wound Care 28: 416-422.
- Janis JE (2014) Essentials of Plastic Surgery, Second CRC Press pp: 1367.
- Karimi H, Latifi NA, Momeni M, Sedigh-Maroufi S, Karimi AM, et al. (2019) Tissue expanders; review of indications, results and outcome during 15 years’ Burns 45(4): 990-1004.
- Tepole AB, Gart M, Purnell CA, Gosain AK, Kuhl E (2016) The Incompatibility of Living Systems: Characterizing Growth-Induced Incompatibilities in Expanded Ann Biomed Eng 44(5): 1734-1752.
- Öksüz S, Alagöz MŞ, Ülkür E (2015) Changing the Donor Site Selection Concept of Facial Skin Expansion from Pure Healthy Tissue to Defect and Healthy Tissue Aesthetic Plast Surg 39(5): 745-751.
- Radwan AM, Zide MF (2019) Tissue Expansion in the Head and Atlas Oral Maxillofac Surg Clin North Am 27(2): 167-173.
- Gonzalez Ruiz Y, López Gutiérrez JC (2017) Multiple Tissue Expansion for Giant Congenital Melanocytic Nevus. Ann Plast Surg 79(6): e37-40.
- Zhu L, Mohan AT, Abdelsattar JM, Wang Z, Vijayasekaran A, et (2016) Comparison of subcutaneous versus submuscular expander placement in the first stage of immediate breast reconstruction. J Plast Reconstr Aesthet Surg 69(4): e77-86.
- Braun TL, Hamilton KL, Monson LA, Buchanan EP, Hollier LH Jr (2016) Tissue Expansion in Children. Semin Plast Surg 30(4): 155-161.
- Kolasinski J (2019) Total Breast Reconstruction with Fat Grafting Combined with Internal Tissue Expansion. Plast Reconstr Surg Glob Open 7(4): e2009.
- De La Cruz Monroy MFI, Kalaskar DM, Rauf KG (2018) Tissue expansion reconstruction of head and neck burn injuries in pediatric patients - A systematic JPRAS Open 18: 78-97.
- Lim YM, Park KH, Lee DW, Lew DH, Roh TS, et al. (2019) Characteristics of adhesion areas between the tissue expander and capsule in implant-based breast reconstruction. Arch Plast Surg 46(4): 330-335.
- Altamirano C, Chávez E, Iñigo AF, Andrade L, Apellaniz A, et al. (2019) Reconstrucción de piel cabelluda (SCALP) con injerto de espesor parcial y expansor tisular secundario a mordedura de perro en paciente pediátrico. Revista Argentina de Cirugía Plástica. Enero - Marzo de 25(1): 21-27.
- Azzi JL, Thabet C, Azzi AJ, Gilardino MS (2020) Complications of tissue expansion in the head and neck. Head Neck 42(4): 747-762.
- Chen Q, Zhang J, Wang B, Wang Y, Kang C, et al. (2020) Total Auricular Reconstruction Using a Single Extended Postauricular Flap Without Skin Grafting in Two Stages: Experiences of 106 Cases. Aesthetic Plast Surg 44(2): 365-372.
- Bellini E, Pesce M, Santi P, Raposio E (2017) Two-Stage Tissue-Expander Breast Reconstruction: A Focus on the Surgical Technique. Biomed Res Int 2017:
- Hoejvig JH, Pedersen NJ, Gramkow CS, Bredgaard R, Kroman N, et al. (2019) Delayed two-stage breast reconstruction: The impact of J Plast Reconstr Aesthet Surg 72(11): 1763-1768.
- Wooten KE, Ozturk CN, Ozturk C, Laub P, Aronoff N, et al. (2017) Role of tissue expansion in abdominal wall reconstruction: A systematic evidence-based review. J Plast Reconstr Aesthet 70(6): 741-751.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- International Journal of AIDS (ISSN: 2644-3023)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Journal of Spine Diseases
- Journal of Cell Signaling & Damage-Associated Molecular Patterns








