3666
Views & Citations2666
Likes & Shares
Jejunal diverticula are rare and remain mostly asymptomatic. However, it can present with acute life-threatening complications, such as gastrointestinal bleeding, bowel obstruction and perforation. We herein present a case of an elderly male who presented with life-threatening hematochezia secondary to jejunal diverticular bleed. While open surgery is the mainstay of management in an emergency setting this case was managed by combined laparoscopy and intra operative push enteroscopy.
CASE REPORT
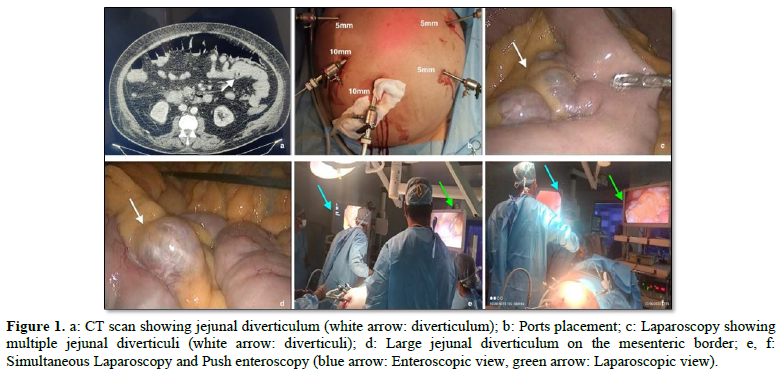
An 80-year-old gentleman, known diabetic and hypertensive with body mass index (BMI) of 44 presented to emergency department with large volume blood in stool. On examination, he was hypotensive and tachycardic. Per abdominal examination revealed mild gaseous distention with vague upper abdominal tenderness. Per rectal examination revealed malena. On evaluation his hemoglobin was 5gm/dL. He was admitted to the intensive care unit and was transfused packed red blood cells. After stabilization, Contrast Enhanced Computed Tomography (CECT) scan abdomen done showed jejunal diverticuli (Figure 1a).
Colonoscopy with terminal ileoscopy done showed entire colon and ileum filled with fresh and altered blood coming from proximal bowel segments. Endoscopy till 2nd part of duodenum did not show any features of bleed. Push enteroscopy using a colonoscope showed multiple jejunal diverticula with one diverticulum showing large clot and active oozing.
Informed written consent was obtained for emergency surgery. He underwent emergency laparoscopic resection and anastomosis of diseased jejunal segment with intra operative push enteroscopy guidance to locate the exact site of bleed under general anesthesia.
Patient was placed in French position and monitor at the head end. Ports were placed as shown in Figure 1b. Duodenojejunal (DJ)flexure was identified, and the bowel loops were walked to identify the affected jejunal segment. From 15 cm from DJ flexure multiple jejunal diverticuli were noted (Figures 1c,1d). Intra operative push enteroscopy with a colonoscope was performed simultaneously to localize the exact site of bleed from the diverticulum (Figures 1e,1f).
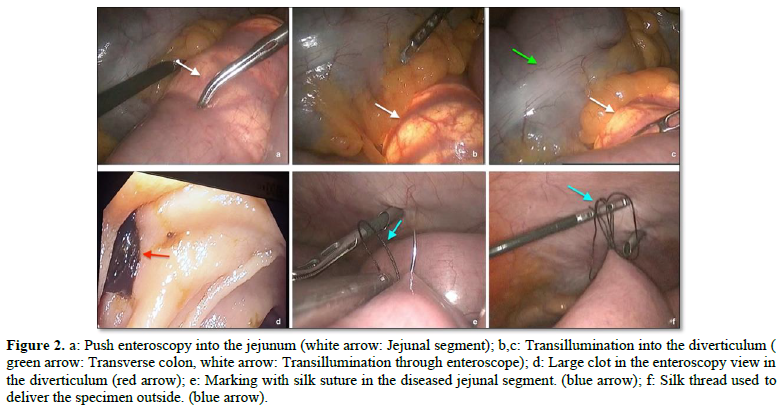
The loop was identified by the transillumination of the colonoscope in the affected diverticula (Figures 2a-2c). The bleeding diverticula was identified by a large clot in the diverticulum (Figure 2d). The identified bleeding and diseased segment of jejunum was marked laparoscopically by silk suture (Figures 2e,2f).
A 4 cm transverse incision was made over the upper abdomen (Figure 3a) and the marked segment of jejunum delivered out. (Figures 3b,3c) The bleeding segment of jejunum along with the adjacent diverticula was resected (Figure 3d), isoperistaltic side to side jejuno-jenunal anastomosis was performed using GIA staplers. (Figure 3e) Mesenteric defect was closed and the bowel was returned to peritoneal cavity and abdomen closed in layers. Nasojejunal tube was passed beyond the anastomosis. Relook laparoscopy was done, and 26 Fr drain placed below the transverse mesocolon just above the anastomosis.
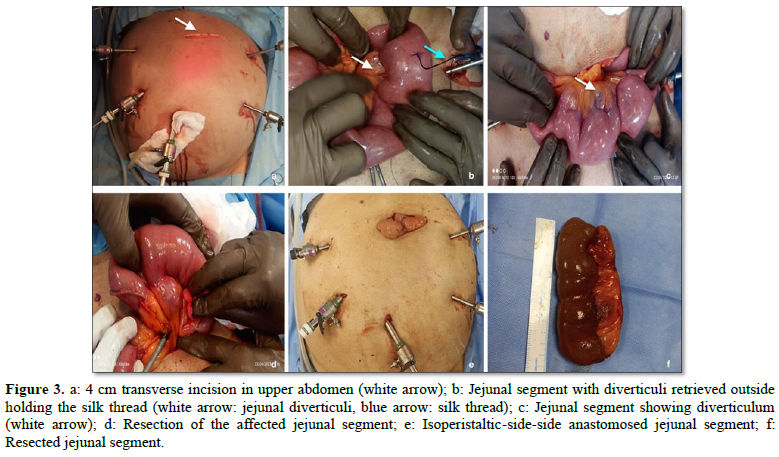
Nasojejunal feeds were started on 2nd post-operative day (POD). Check Contrast Tomography scan of abdomen with oral contrast was done on the 3rd POD which revealed smooth transit of oral contrast through the anastomotic site with no leak. He was started on oral liquids and gradually soft diet. He was discharged on the 5th POD and abdominal drain was removed on the 7th POD. The histopathogy of the resected jejunal segment (Figure 3f) was consistent with diverticular disease. At one year follow up he did not have any episodes of GI bleed.
DISCUSSION
Jejunal diverticular disease is rare and believed to develop because of abnormalities in peristalsis, intestinal dyskinesia, and high-segmental intraluminal pressures [5] These pulsion-type false diverticula occur along the mesenteric border of the intestine, where blood vessels pierce the muscularis layer of the bowel wall, causing weak areas to develop. It is usually asymptomatic but may rarely present with life-threatening complications including massive GI bleeding [2,3]. There have been less than 60 case reports in the English literature describing massive hemorrhage from jejunal diverticula [6]. Bleeding is caused due to acute erosive diverticulitis and mucosal ulceration, which compromise the mesenteric blood supply causing hemorrhage [7].
In the study by Rodriguez [8] bleeding jejunal diverticula account for 2% of symptomatic cases. Other complications such volvulus, diverticulitis with or without perforation or abscess occur in 10-30% of patients [1,9]. Although jejunal diverticulosis can be diagnosed by endoscopy, abdominal CT, barium follow through, enteroclysis is the investigation of choice [3,10,11]. In cases of jejunal diverticular bleeding, selective mesenteric angiography or CT angiogram can be used to localize active bleeding if renal profile is within normal limits [6]. Emergency surgical intervention is indicated in the presence of acute complications of jejunal diverticula including diverticulitis, massive bleeding or bowel perforation both as a diagnostic and therapeutic measure [3,6,10].
Laparoscopy has many advantages in treatment of bleeding jejunal diverticula. It can be rapidly converted to mini laparotomy, with clear pinpoint at the area of the affected segment guiding the surgeon to the ideal incision site on the abdominal wall, minimizing the operative time and postoperative pain. It also reduces the morbidity of large exploratory laparotomy incision. Nadarajan AR [12] in their case report stated the advantage of intra operative enteroscopy to identify the exact bleeding diverticula in the event of multiple diverticula and blood-filled bowel loops. Intra operative enteroscopy helped to identify and mark the bleeding jejunal diverticula in our case as well which presented with multiple jejunal diverticula and blood-filled bowel loops which posed a diagnostic challenge by laparoscopy alone.
While many types of investigations are available to localize the site of bleed, they have the limitations of cost and availability. Intraoperative enteroscopy is a useful, easily performed, and generally available facility. A good endoscopist is of prime importance to localize the bleeding diverticula as it requires entry into multiple diverticula and bowel loops that are filled with blood in an emergent setting. Additionally, a team of well-trained anesthesiologists and intensivists are of vital importance in managing geriatric patients with hemodynamic instability in an emergency setting by laparo-enteroscopic approach.
Yaqub [6] in their study have similarly managed a case of massive rectal bleed from acquired jejunal diverticula with emergency laparotomy, on table enteroscopy to locate the exact site of bleeding diverticula and resection of the diseased bowel segment. Abegunde [13] have reported a case wherein push enteroscopy with a pediatric colonoscope was used to visualize the site of jejunal bleed and was tattooed. The patient then underwent emergency laparotomy and resection of the tattooed diseased segment of jejunum. Ming Chen Ba [14] in a case series of 22 patients with small intestinal bleed due to benign and malignant causes have enumerated the use of perioperative enteroscopy and endo laparoscopy in the diagnosis and treatment of small intestinal bleed.
Radionuclide imaging and angiography may be appropriate in patients with massive gastrointestinal hemorrhage in whom the bleeding source has not been identified through colonoscopy and gastrointestinal endoscopy. However, the angiography might identify a hemorrhage site only when the rate of ongoing arterial bleeding is more than 1 ml/min [15]. Angiographic localization also allows for embolization for the patients with acute arterial bleeding. Angiography requires a bleeding rate > 1 ml/min for accurate detection of extravasation of contrast into the bowel lumen through radionuclide imaging using technetium tagged red blood cells.
CONCLUSION
Bleeding jejunal diverticulum is rare and can be safely and efficiently managed by emergency combined laparoscopy guided by intraoperative push enteroscopy to locate the exact site of bleeding in case of multiple diverticuli.
- Kassahun WT, Fangmann J, Harms J, Bartels M, Hauss J (2007) Complicated small bowel diverticulosis: A case report and review of the literature. World J Gastroenterol 13: 2240-2242.
- Ferreira-Aparicio FE, Gutiérrez-Vega R, Gálvez-Molina Y, Ontiveros-Nevares P, Athie-Gútierrez C, et al. (2012) Diverticular disease of the small bowel. Case Rep Gastroenterol 6: 668-676.
- Nejmeddine A, Bassem A, Mohamed H, Hazem BA, Ramez B, et al. (2009) Complicated jejunal diverticulosis: A case report with literature review. North Am J Med Sci 1: 196-19
- Krishnamurthy S, Kelly MM, Rohrmann CA, Schuffler MD (1983) Jejunal diverticulosis. A heterogenous disorder caused by a variety of abnormalities of smooth muscle or myenteric plexus. Gastroenterology 85: 538-5
- Kumar M, Vallence K (2005) Small Intestinal Diverticulosis (SID). Internet J Gastroenterol 3(2): 1-3.
- Yaqub S, Evensen BV, Kjellevold K (2011) Massive rectal bleeding from acquired jejunal diverticula. World J Emerg Surg 6: 17.
- De Freitas GP, Lima H, Borges A (2013) Uncommon cause of gastrointestinal hemorrhage: Jejunal diverticula. Int J Surg 9: 2.
- Rodriguez HE, Ziauddin MF, Quiros ED, Brown AM, Podbielski FJ, et al. (2001) Jejunal Diverticulosis and Gastrointestinal Bleeding. J Clin Gastroenterol 33(5): 412-414.
- Woods K, Williams E, Melvin W, Sharp K (2008) Acquired jejunoileal diverticulosis and its complications: A review of the literature. Am Surg 74: 849-8
- Butler JS, Collins CG, McEntee GP (2010) Perforated jejunal diverticula: A case report. J Med Case Rep 4: 172.
- Fintelmann F, Levine MS, Rubesin SE (2008) Jejunal diverticulosis: Findings on CT in 28 patients. AJR Am J Roentgenol 190: 1286-12
- Nadarajan AR, Rymbai ML, Chase S, Nayak S (2018) Jejunal Diverticulosis Presenting as an Obscure Gastrointestinal Bleed a Challenge in Diagnosis and Management. Indian J Surgery 81: 86-88.
- Abegunde AT, Christman E, Hassell LA, Kastens D (2016) Rare Jejunal Diverticular Bleeding. ACG Case Rep J 3(4): e146.
- Ba MC, Qing SH, Huang XC, Wen Y, Li GX, et al. (2006) Application of laparoscopy in diagnosis and treatment of massive small intestinal bleeding: Report of 22 cases. World J Gastroenterol 12(43): 7051-7054.
- Edelman DA, Sugawa C (2007) Lower gastrointestinal bleeding: A review. Surg Endosc 21: 514-520.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Journal of Alcoholism Clinical Research
- Ophthalmology Clinics and Research (ISSN:2638-115X)





