3341
Views & Citations2341
Likes & Shares
The superficial circumflex iliac artery perforator (SCIP) flap is supplied by only a perforator of the superficial circumflex iliac system and has a short segment (3 to 4 cm in length) [4].
CASE
Our case is 76-year-old woman with, skin phototype 4, who presented with a lesion affecting the left temporal region since 2-3 years. Clinical and dermoscopy exams were suggestive of basal cell carcinoma which progressed to squamous cell carcinoma over the edges (Figures 1 & 2).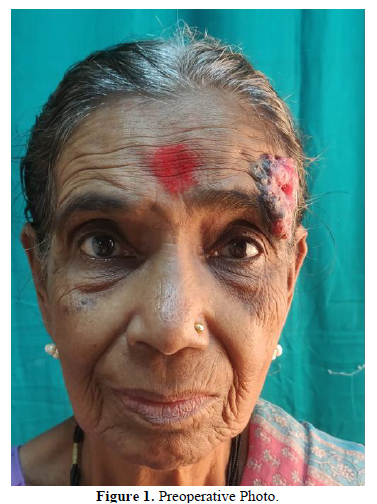

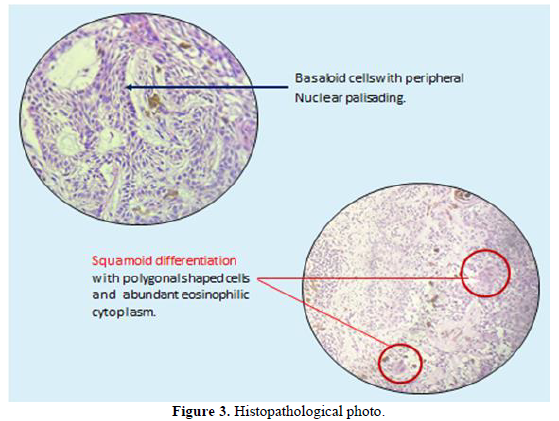
On assessment, she had no significant co-morbities and the lesion did not invade the underlying bones. Other examination was within normal limits. The patient was placed in a supine position with a head ring to stabilize the head and shoulder roll to extend the neck. Patient had a wide local excision plus reconstruction under general anesthesia. Microscopic examination revealed nodular basal cell carcinoma and poorly differentiated squamous cell carcinoma areas, significantly compromising the resection’s deep margin. The next phase obtained free margins, with an intense inflammatory infiltrate. Again a revised margin was done and all the deep as well as the circular boundary became free of tumor cells and inflammatory infiltrate (Figure 3). A local cervicofacial advancement and rotation flap could not be done. Finally decision was made to go ahead with reconstruction using SCIP flap (Figure 4).

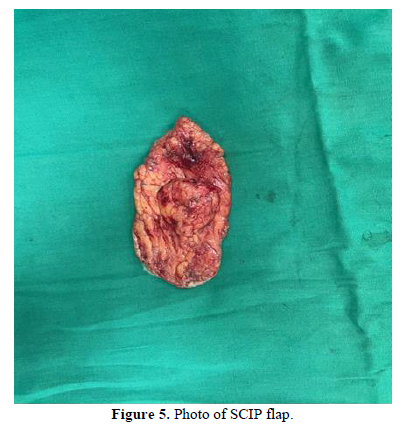
And it gave a good pliable cover, contour and skin match (Figure 5). The flaps were closed in single layer with sutured with 3-0 nylon (Figure 6).

The recipient vessel used for the flap was eternal carotid with end to side anastomosis and the vein was facial vein.
The patient had an excellent aesthetic and functional result on the reconstructed temporal skin, with no complications. The patient is undergoing dermatological follow up postoperatively for period of 1 year (Figures 7a & 7b).


Patient was satisfied with the cosmetic outcome with no flap necrosis, complications, complaints or tumor recurrence. She has been advised flap debulking procedure to enhance outcome.
DISCUSSION
BSC is a rare, aggressive non-melanoma skin cancer with no clarity existing around the classification, pathogenesis, histologic morphology, biologic behavior, prognosis and management of this tumor [5]. Rotational flap is one of the best approaches for reconstruction of facial defects and gives good cosmetic result [6]. Free flaps require expertise and do not provide color and texture match. Modified cervicofacial flaps provide an excellent color and texture match and reduce operative time and surgical complications and can be performed under local anesthesia with less donor site morbidity [7]. The SCIP flap is widely used since it was first described in 2004 by Koshima [4]. Later Lita and his colleagues demonstrated success of the SCIP flap in reconstructive of head and neck defects [8].
Although rare, BSC has diagnostic challenges and metastatic ability. While there are many approaches to reconstructing midfacial defects, none of them are fully satisfactory. The literature is also limited. Our case report shows that the SCIP flap plays an important role due to its outstanding esthetic and functional merits and does not need deeper and longer dissection for the pedicle vessel, a shorter flap elevation time, possible thinning of the flap, a hidden donor site, less donor-site morbidity, and the availability of a large cutaneous vein as a venous drainage system.
CONCLUSION
The main aim of surgery is to surgically remove the tumor with wide marginal excision and reconstruct the deformity with minimal scarring to achieve a better cosmetic result and using SCIP flap can be seen as one of the best approaches and gives good aesthetic results.
- Fotiadou C, Apalla Z, Lazaridou E (2021) Basosquamous Carcinoma: A Commentary. Cancers (Basel) 13(23): 6146.
- Garcia C, Poletti E, Crowson AN (2009) Basosquamous carcinoma. J Am Acad Dermatol 60(1): 137-143.
- Lee DM, Bae YC, Nam SB, Bae SH, Choi JS (2017) Reconstruction of Large Facial Defects via Excision of Skin Cancer Using Two or More Regional Flaps. Arch Plast Surg 44(4): 319-323.
- Koshima I, Nanba Y, Tsutsui T, Takahashi Y, Urushibara K, et al. (2004) Superficial circumflex iliac artery perforator flap for reconstruction of limb defects. Plast Reconstr Surg 113(1): 233-240.
- Fotiadou C, Apalla Z, Lazaridou E (2021) Basosquamous Carcinoma: A Commentary. Cancers (Basel) 13(23): 6146.
- Malipatil SR, Jonnalagadda SV (2019) Surgical Excision with Rotational Flap Reconstruction for Basosquamous Cell Carcinoma in Xeroderma Pigmentosa: A Case Report. Indian J Otolaryngol Head Neck Surg 71(Suppl 1): 702-705.
- Ogunkeyede A, Solagbade R, Lawal A (2023) Versatility of cervicofacial flap in management of cutaneous cheek defects post tumor excision: A report of two cases. Afri Health Sci 23(1): 511-514.
- Li Z, Zheng D, Zheng J, Qi W, Qi Q, et al. (2020) Free superficial circumflex iliac artery perforator flap with a single-pedicle bilobed design for pediatric multi-digit defect reconstruction. J Orthop Surg Res 15(1): 216.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Spine Diseases
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Alcoholism Clinical Research
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)










