4159
Views & Citations3159
Likes & Shares
DISCUSSION
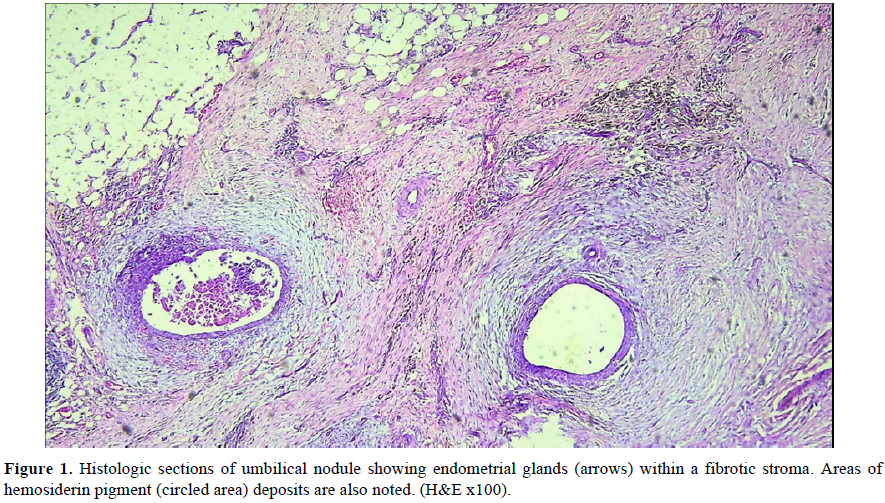
Any organ or tissue may be involved in extra-pelvic endometriosis. Endometriotic tissue has been found in the Colon and Rectum causing cyclical per rectal bleed, in the bladder, the Lungs and the Brain, resulting in catamenial hematuria, hemoptysis and seizure [12]. Primary cutaneous endometriosis, otherwise called spontaneous, is the one that developed denovo. A secondary endometriosis is said to follow iatrogenic or traumatic scar [13] a result of direct, iatrogenic, lymphatic or hematogenous spread from pelvic endometriosis [14] or a result of metaplasia [15]. Primary umbilical endometriosis is a rarity as noted earlier [1]. There is no consensus on its pathogenesis, as various theories are put forward to explain this bizarre phenomenon [12]. The Umbilicus is considered to be a physiologic scar, therefore, has tropism for endometriosis like other scar tissues [14]. This may be the case in our patient, because, no preceding history of pelvic surgery was obtained. The differentials for an umbilical nodule are numerous, the cyclical pain, variation in color or size that coincides with menstruation is often the only hint for a clinical diagnosis [16]. The index patient also presented with the monthly cyclical pain and the color and size variation. A constant pain in an umbilical Endometrioma has also been reported [16]. In the absence of pain, during pregnancy and menopause, establishing a clinical diagnosis may be difficult. It is therefore pertinent to keep in view other differentials such as: pyogenic granuloma, umbilical polyp, melanocytic nevus, seborrheic keratosis, epithelial inclusion cyst, desmoid tumor, hemangioma and granular cell tumor [17]. An incarcerated umbilical hernia, omphalitis, keloid and foreign body granuloma may also present as umbilical nodule [16]. As noted earlier, malignant lesions of the umbilical skin such as melanoma, squamous and basal cell carcinoma, and metastatic Mary Joseph’s nodules from the gastrointestinal tract may also be found [5,17].
Although majority is diagnosed based on clinical suspicion, radiological assessment could improve the chance of making the right diagnosis. An ultrasound evidence of an umbilical hypoechoic mass with foci of hyperechoic regions and evidence of increased vascular flow on Doppler interrogation is very helpful [18]. An ultrasound scan can also help the surgeon to estimate the size of the nodule, involvement of the parietum, pelvic organs and other viscera like the colon [18]. In difficult cases an MRI may be done, especially if a pelvic endometriosis is suspected and to rule out transcoelomic spread of metastatic nodules from the gastrointestinal tract. The MRI features of an umbilical endometriosis reported are the presence of a homogeneous hypointense lesion on T1-weighted sequence with low signals on T2 weighting [19,20].
The rarity of umbilical endometriosis has made its treatment to be mainly dependent on the experience of the surgeon. Medical treatment has been tried in some patients, but no randomized controlled trial has been done to assess its efficacy [14,16]. The drugs commonly used include progesterone, nor-ethysterone, androgens like Danazol and Gonadotrophin Releasing Hormone analogue, such as Goserelin and Boserelin. The most consistent effect reported is the symptomatic relief of pain and reduction in the size of the nodule after medical treatment [17]. Surgery has so far remained the most promising treatment for umbilical endometriosis [21]. The goal should be a complete resection with no recurrence, but, this is an uphill task in a disease with tropism for scar tissue like endometriosis. Surgical umbilical resection with or without repair of underlying fascia and peritoneum, or enucleation of the endometrial nodule with preservation of the umbilicus are mostly done. Total resection of umbilicus is however, preferred, as it carries low risk of recurrence [17].
CONCLUSION
A spontaneous umbilical Endometrioma is rare, high index of suspicion is required regarding any umbilical nodule with cyclical symptoms, and the possibility of sinister differentials like metastatic adenocarcinomatous nodules should always be entertained.
CONFLICT OF INTEREST
None
- The WT, Vollen hoven B, Harris PI (2006) Umbilical endometriosis, a pathology that a gynecologist may encounter when inserting the Veres needle. Fertil Steril 86(6): 1764.e1-2.
- Dorothy M, Timona O, Steve M, Felix O (2020) Umbilical endometriosis: A case series. J Med Case Rep 14: 142.
- Eskenazi B, Warner ML (1997) Epidemiology of endometriosis. Obstet Gynecol Clin North Am 24(2): 235-258.
- Audebert A, Petousis S, Margioula-Siarkou C, Ravanos K, Prapas N, et al. (2018) Anatomic distribution of endometriosis: A reappraisal based on series of 1101 patients. Eur J Obstet Gynecol Reprod Biol 230: 36-40.
- Giudice LC, Kao LC (2004) Endometriosis. Lancet 364: 1789-1799.
- Mustafa TB, Mehmet AA, Fatima AK, Mehmet AÇ, Ahmet S (2017) Primary umbilical endometriosis: Menstruating from the umbilicus. Turkderm-Turk Arch Dermatol Venereol 51: 101-103.
- Latcher JW (1953) Endometriosis of the umbilicus. Am J Obstet Gynecol 66: 161-168.
- Mann LS, Clarke WR (1964) Endometriosis of the umbilicus. IMJ III Med J 125: 335-336.
- Elias B, Adam E, Ziadeh H, Matta C (2017) Atypical clinical presentation of primary umbilical endometriosis. Clin Surg 2: 1635.
- Dessy LA, Buccheri EM, Chiummariello S, Gagliardi DN, Onesti MG (2008) Umbilical endometriosis, our experience. In vivo 22: 811-815.
- Fuminori T, Eriko H, Yukihiro A, Chihiro U, Keigo A, et al. (2016) Primary Umbilical Endometriosis: Unusual and Rare Clinical Presentation. Case Rep Obstet Gynecol 2016: 9302376.
- Dridi D, Chiaffarino F, Parazzini F, Donati A, Buggio L, et al. (2022) Umbilical Endometriosis: A Systematic Literature Review and Pathogenic Theory Proposal. J Clin Med 11(4): 995.
- Hirata T, Koga K, Kitade M, Fukuda S, Neriishi K, et al. (2020) A national Survey of Umbilical Endometriosis in Japan. J Minim Invasive Gynecol 27: 80-87.
- Jaime TJ, Jaime TJ, Ormiga P, Leal F, Nogueira OM, et al. (2013) Umbilical endometriosis: Report of a case and its dermoscopic features. Anais brasileiros de dermatologia 88(1): 121-124.
- Romera-Barba E, Ramón-Llíon JC, Pérez AS, Navarro GI, Rueda-Pérez JM, et al. (2014) Endometriosis umbilical primaria. A propósito de 6casos. Rev Hispanoam Hernia 2: 105-110.
- Seracettin E, Bedri Aras P¸ Semih H, Veli M (2016) Primary umbilical endometriosis: A painful swelling in the umbilicus concomitantly with menstruation. Int J Surg Case Rep 28: 78-80.
- Boccara D, Runz AD, Marco O, Chaouat M, Mimoun M (2016) Primary Skin Umbilical Endometriosis: About One Case. J Clin Case Rep 6: 742.
- Genovese G, Passoni E, Veraldi S, Nazzaro G (2018) Ultrasonographic findings in primary umbilical endometriosis. A Bras Dermatol 93(2): 297-298.
- Hartigan C, Holloway B (2005) MR imaging features of endometriosis at the umbilicus. Br J Radiol 78(932): 755-757.
- Yu CY, Perez-Reyes M, Brown JJ, Borrello JA (1994) MR appearance of umbilical endometriosis. J Comput Assist Tomogr 18(2): 269-271.
- Datta S, Basu R (2021) Spontaneous Primary Umbilical Endometriosis Preceding Severe Pelvic Endometriosis: A Case Report. J South Asian Feder Obst Gynae 13(5): 350-351.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Oncology Clinics and Research (ISSN: 2643-055X)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Journal of Spine Diseases
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- International Journal of AIDS (ISSN: 2644-3023)



