Review Article
Surgical Management of the Descending Aorta Coarctation Secondary to Takayasu’s Disease
4336
Views & Citations3336
Likes & Shares
Takayasu’s disease is a chronic nonspecific inflammatory vasculitis that mainly affects the aorta and its main branches. Stenotic involvement of the descending aorta is very uncommon, and the clinical expression may mimic an aortic coarctation.
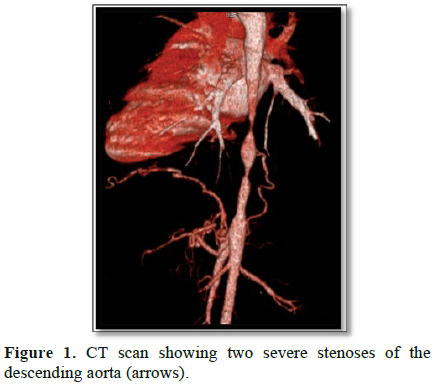
We report the case of a 25-year-old woman, treated with corticoids for Takayasu’s disease, who consulted for lower limb claudication with non-controlled hypertension. Pulses in the lower limbs were absent without signs of limb ischemia. An aortic stenosis was highly suspected. The CT scan showed two severe stenoses on the descending thoracic aorta above the diaphragm.
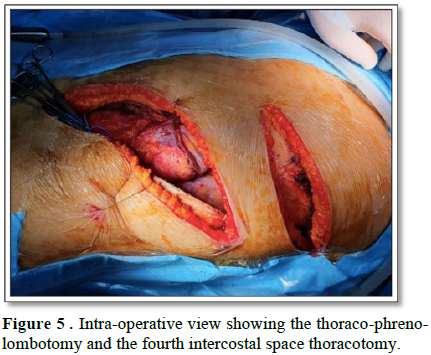
The surgery was performed under general anesthesia and thoraco-phreno-lombotomy, without extra corporeal circulation.
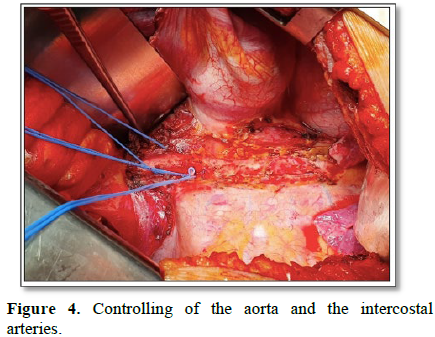
After controlling the thoraco-abdominal aorta and the intercostal arteries just above the coeliac trunk, we were not able to control the upper neck so we performed a second thoracotomy in the 4th intercostal space.
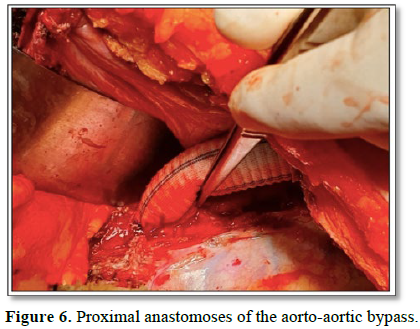
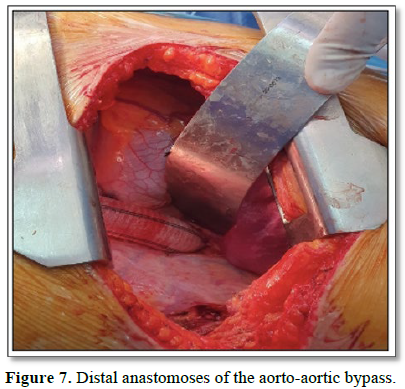
Via lateral clamping of the aorta, we performed an aorto-aortic bypass with a tubular Dacron graft. No complications were noted after the surgery, and we noted the reappearance of lower limb pulses.
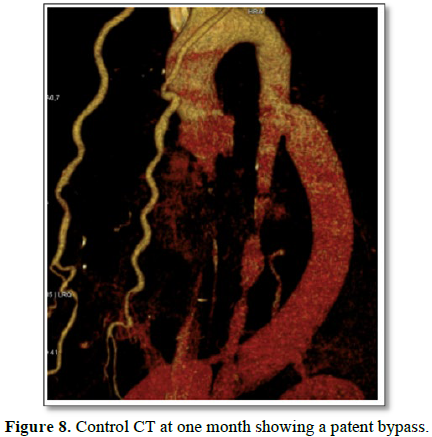
One month later, we noted that blood pressure was less elevated, and there was a decrease on number and dose of anti-hypertensive drugs by the cardiologist. The lower limb claudication also disappeared. The CT Scan control showed a patent bypass.
Descending thoracic aortic stenosis secondary to Takayasu’s disease remains a rare event. Renovascular hypertension is the main indication for aortic repair. Surgical repair is safe and is considered the best choice of treatment.
Keywords: Artic coarctation, Takayasu’s disease, Surgery, Bypass
INTRODUCTION
Takayasu’s arteritis was first described in 1908 by Mikito Takayasu in Japan [1]. It is a chronic nonspecific inflammatory vasculitis of unknow etiology that mainly affects the aorta and its main branches. The inflammatory process results in structural changes that lead to vascular wall fibrosis and stenosis[2,3]. Stenosisis the most common vascular lesion [3,4], but aortic aneurysms are also described in the literature. Stenotic involvement of the descending aorta is very uncommon, and the clinical expression may mimic an aortic coarctation.
We report the case of a successful surgical management of an aortic coarctation secondary to Takayasu’s disease.
CASE REPORT
A 25-year-old woman, treated with corticoids for Takayasu’s disease since the age of 18, consulted in our institution for lower limb claudication with non-controlled hypertension under 3 different antihypertensive drugs. On physical examination, there was a pulse and blood pressure asymmetry between the left and right arms. The blood pressure on right arm was 180/100 mmHg and 140/85mmHg on the left arm. Pulses in the lower limbs were absent without signs of limb ischemia. The walking perimeter was 200 m. In laboratory tests, erythrocyte sedimentation rate was 2.9 mg/dL. Echocardiography showed signs of (ESR) was 40 mm/Hour and the C-reactive protein (CRP) hypertensive cardiopathy but no signs of heart failure.
Due to the absence of lower limb pulses and non-controlled hypertension, an aortic stenosis was highly suspected. The CT scan showed two severe stenoseson the descending thoracic aorta just above the diaphragm (Figure 1). The distal aorta after the stenosis was hypoplastic and there was no sufficient lower neck length to allow a proper landing zone for an endovascular repair. In addition, the risk of post TEVAR paraplegia was very high due to the coverage of well-developed intercostal collaterals.
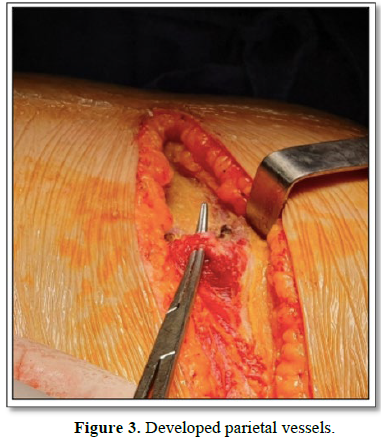
The surgical procedure was performed under general anesthesia and without extra corporeal circulation. We decided to perform a thoraco-phreno-lombotomy (Figure 2) in order to access the thoraco-abdominal portion of the aorta. From the cutaneous incision, there was a very developed parietal collateral circulation (Figure 3).
After controlling the thoraco-abdominal aorta and the intercostal arteries just above the coeliac trunk (Figure 4), we were not able to control the upper neck. So, we performed a second thoracotomy through the 4th intercostal space (Figure 5). We administrated a 1mg/kg bolus of heparin, andvia lateral clamping of the aorta, we performed an aorto-aortic bypass with a 20 mm tubular Dacron graft (Figures 6 and 7). No complications were noted after the surgery, and we noted the reappearance of lower limb pulses.
One month later, we noted that blood pressure values were less elevated and there was a decrease on the number and the doses of anti-hypertensive drugs by the cardiologist.
The lower limb claudication also disappeared. The CT Scan control showed a perfectly patent bypass (Figure 8).

DISCUSSION
Takayasu arteritis is a chronic idiopathic inflammatory disease which mostly affects the aorta and its main branches. The median age at presentation is 30 years, ranging from 4 to 63 years [4]. The main histological changes are granulomatous vasculitis of the medium and the large arteries. Stenotic lesions are more common; however, mixed lesions and aneurysmal dilations may also be seen [5]. Female patients with Takayasu arteritis have more frequent involvement of the thoracic aorta and its branches, where as involvement of the abdominal aorta and its branches is more common in males.
Ethnicity implication is also well described, according to Hata et al. [6], the aorticarch and its branches are mostly affected in Japanese patients, however in Indian patients, the abdominal aorta is mostly affected part [4]. Aortic involvement is found in 50-76% of the patients [7], it can be seen from the ascendant aorta to below the iliac bifurcation.
Therapy is based on glucocorticoids, but once arterial stenosis is formed, angioplasty or bypass grafts are the two available therapeutic options [5]. Renovascular hypertension is the main indication for interventional or surgical repair [5].
Endovascular repair is an attractive option [8-10]. Despite there have been many reports of successful endovascular repair procedures, reports of long-term outcomes and event-free survival are sparse. In fact, Destruction of the elastic fibers inside the vascular wall could explain the poor vessels response to endovascular repair in Takayasu arteritis patients [11]. In addition, because of the concomitant aortic branch involvement, the aortic anatomy become hostile and not suitable for endovascular repair. The well-developed collateral circulation and the extent of diseased aortic segment places the paraplegia risk as high. Considering the relatively young age of the patients, long-term durability is not certain in case of endovascular repair and becomes an essential determinant for selecting the type of treatment. Moreover, TEVAR should be carefully performed and reserved for patients with a high anesthetic and operative risk [12].
Also, surgical management of coarctation-like aortic stenosis is well reported in the literature [9,12-17]. In fact, surgical management is considered the best choice. It is recommended that open repair should not be performed during the active phase [12] and proper preparation before surgery is necessary by administrating corticosteroids, and eventually immune suppressive agents and antihypertensive drugs in order to return ESR to normal to reduce the operation risk [18] Taketani et al. [14] reported in their study about 33 patients with Takayasu arteritis that overall and event-free survival rates at 20 years were 62.3% and 58.4%. Field et al [10] also concluded that surgery was considered safe with excellent long-term results; Moreover, patients with active disease were at risk for reintervention [12].
As for high blood pressure after surgical repair, Cohen et al [19], reported that 96% of patients were normotensive or had easily controllable hypertension postoperatively [14], like in our case, the blood pressure levels decreased in the same way of the need of antihypertensive drugs.
CONCLUSION
Descending thoracic aortic stenosis secondary to Takayasu’s disease remains a rare event. Renovascular hypertension is the main indication for aortic repair. Surgical repair is safe and considered the best choice of treatment. However, surgery is not recommended during the active phase and therapy with corticosteroids, eventually immune suppressive agents and antihypertensive drugs are strongly advised before repair.
- Sugawara Y, Sueda T, Orihashi K, Okada K (2002) Surgical treatment of atypical aortic coarctation associated with occlusion of all arch vessels in Takayasu’s disease. Eur J Cardiothorac Surg 22: 836-838.
- Jmaa Hela B, Saif El Hak H, Oussama D, Faten F, Sayda M, et al. (2017) Isolated Aortic Aneurysm with Aortic Valve Regurgitation in Takayasu Disease. J Clin Exp Cardiol [Internet].
- Che W, Xiong H, Jiang X, Dong H, Zou Y, et al. (2018) Stenting for middle aortic syndrome caused by Takayasu arteritis-immediate and long-term outcomes. Catheter Cardiovasc Interv 15 févr 91: 623-631.
- Johnston SL, Lock RJ, Gompels MM (2002) Takayasu arteritis: a review. J Clin Pathol l 55: 481-486.
- Ashwal AJ, Murugaiyan R, Padmakumar R, Reddy R, Rao S, et al. (2016) A rare and uncommon association: A case of Takayasu arteritis presenting as typical coarctation of aorta in a pediatric patient. J Indian Coll Cardiol 6: 38-40.
- Hata A, Noda M, Moriwaki R, Numano F (1996) Angiographic findings of Takayasu arteritis: New classification. Int J Cardiol août 54: S155-S163.
- Chung JW, Kim H-C, Choi YH, Kim SJ, Lee W, et al. (2007) Patterns of aortic involvement in Takayasu arteritis and its clinical implications: Evaluation with spiral computed tomography angiography. J Vasc Surg 45: 906-914
- Carr JA (2006) The Results of Catheter-Based Therapy Compared With Surgical Repair of Adult Aortic Coarctation. J Am Coll Cardiol 47: 1101-1107
- Perera AH, Youngstein T, Gibbs RGJ, Jackson JE, Wolfe JH, et al. (2014) Optimizing the outcome of vascular intervention for Takayasu arteritis: Outcome of vascular intervention for Takayasu arteritis. Br J Surg 101: 43-50
- Macdonald S, Thomas SM, Cleveland TJ, Gaines PA (2003) Angioplasty or Stenting in Adult Coarctation of the Aorta? A Retrospective Single Center Analysis Over a Decade. Cardiovasc Intervent Radiol 26: 357-364
- Mwipatayi BP, Jeffery PC, Beningfield SJ, Matley PJ, Naidoo NG, et al. (2005) TAKAYASU ARTERITIS: CLINICAL FEATURES AND MANAGEMENT: REPORT OF 272 CASES. ANZ J Surg mars 75: 110-117
- Kim SM, Jung IM, Han A, Min SI, Lee T, et al. (2015) Surgical treatment of middle aortic syndrome with takayasu arteritis or midaortic dysplastic syndrome. Eur J Vasc Endovasc Surg 50: 206-212
- Fields CE, Bower TC, Cooper LT, Hoskin T, Noel AA, et al. (2006) Takayasu’s arteritis: Operative results and influence of disease activity. J Vasc Surg 43: 64-71
- Taketani T, Miyata T, Morota T, Takamoto S (2005) Surgical treatment of atypical aortic coarctation complicating Takayasu’s arteritis-experience with 33 cases over 44 years. J Vasc Surg 41: 597-601
- Ham SW, Subramanyan RK, Rowe VL, Weaver FA (2010) RR12 Disease progression following initial surgical intervention for takayasu’s arteritis. J Vasc Surg 51: 92S
- Miyata T, Sato O, Koyama H, Shigematsu H, Tada Y, et al. (2003) Long-term survival after surgical treatment of patients with takayasu’s arteritis. Circulation 108: 1474-1480
- Saadoun D, Lambert M, Mirault T, Resche-Rigon M, Koskas F, et al. (2012) Retrospective analysis of surgery versus endovascular intervention in takayasu arteritis: A multicenter experience. Circulation 125: 813-819
- Bao (2013) Arteritis mimicking aortic coarctation and review of the literature. J Med Cases [Internet]
- Cohen JR, Birnbaum E (1988) Coarctation of the abdominal aorta. J Vasc Surg 8: 160-164
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- International Journal of AIDS (ISSN: 2644-3023)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Renal Transplantation Science (ISSN:2640-0847)










