Research Article
A Prospective Study to Evaluate Histopathological Detection of Helicobacter Pylori in Perforated Peptic Ulcer Cases
4693
Views & Citations3693
Likes & Shares
Background: Although the role of Helicobacter pylori (H. pylori) is well known in peptic ulcer disease (PUD) etiology, its role in perforated peptic ulcer (PPU) is not well established. This study aimed to evaluate the role of H. pylori infection in patients with PPU and to find its prevalence in patients with PUD.
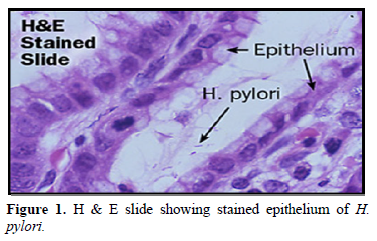
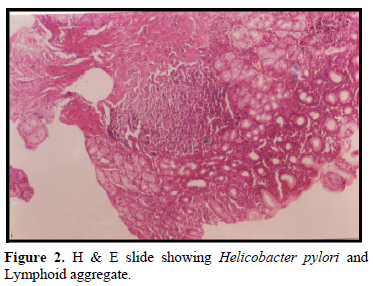
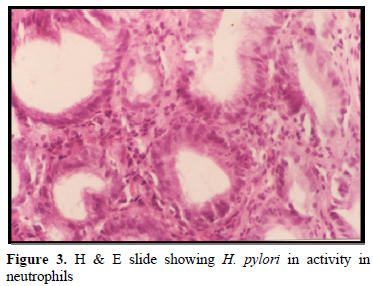
Methodology: This study was conducted on 50 cases of perforated gastric or duodenal ulcer managed by simple closure and omentopexy in the Department of Surgery. Patients having some other associated pathology like tuberculosis, pancreatitis, ileal or colonic perforation were excluded. Similarly, Patients having peptic perforation due to some trauma or penetrating injury of abdomen or due to some corrosive poisonings were also excluded. Patients who had received anti H. pylori regimen, preoperatively or post operatively were also excluded. Intraoperatively, perforation margins were taken for histopathology and perforation was closed with 3’0’ mersilk suture and an omental patch was stitched over it. Post operatively all patients were put on appropriate antibiotics. On follow up, patients were put on H2 blocker: Ranitidine and endoscopic biopsy after one month was done from the gastric antrum which was examined for presence of H. pylori. The biopsy material was examined with hematoxylin and eosin staining for presence of H. pylori.
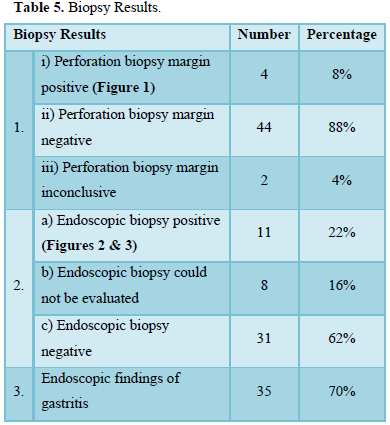
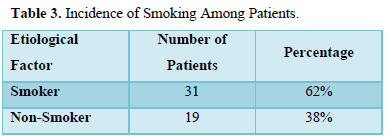
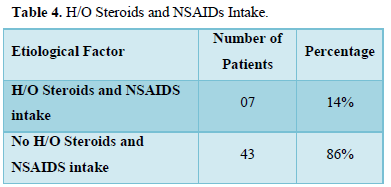
Results: In 88% of patients the perforation margin stained negative for H. pylori and 62% of the antral biopsies in the post operative were negative for H. pylori. Thus, indicating the low prevalence of H. pylori in peptic ulcer perforation cases. Also, history of smoking/alcoholism was positive in 38% cases. History of drugs (non-steroidal anti-inflammatory and steroids) was positive in 14% of cases. This study suggested that peptic ulcer perforation has multiple causes and associated factors.
Conclusion: H. pylori infection was not significantly associated with PPU. Some other factors like alcohol intake and tobacco were also involved in perforation. We can conclude that H. pylori infection is not a risk factor for PPU.
Categories: Gastroenterology, General Surgery, Infectious Disease
Keywords: Helicobacter pylori, Peptic ulcer, Smoking, NSAID, Alcohol
INTRODUCTION
Helicobacter pylori have been associated with gastric and duodenal ulcers in most of the studies and data but its role in complications like peptic ulcer perforation needs to be evaluated. It is important to know the role of H. pylori in peptic ulcer perforation to plan the surgical procedure for peptic ulcer perforation patients. In patients with peptic ulcer perforation with H. pylori infection, simple closure of perforation with omental patch may suffice followed by H. pylori eradication therapy in the postoperative period. In patients with increased acid production where H. pylori has not been detected, other acid reducing surgeries need to be done during the closure of perforation with omentum patch overlay, to prevent the recurrence of perforation of ulcers.
Peptic ulcer is defined as defects in gastrointestinal mucosa extending through the mucosa into the sub-mucosa and deeper into muscularis mucosa that persists as a function of acid peptic activity in gastric juice [1]. In the past it appeared that ulcers were caused by acid and that if acid could be suppressed the ulcer would heal even though they tend to reoccur. Serological studies from different regions show that exposure to H. pylori infection occurs early in life; by the end of 2nd decade over 80% of the population has IgG antibodies to H pylori [2]. Most studies report prevalence of H. pylori as approximately 70% - 90% in patients with duodenal ulcer [3]. The male to female ratio now varies between 1.9:1 to 2.9:1 which is significantly lower compared to a ratio of 5:1, 20 years ago [4].
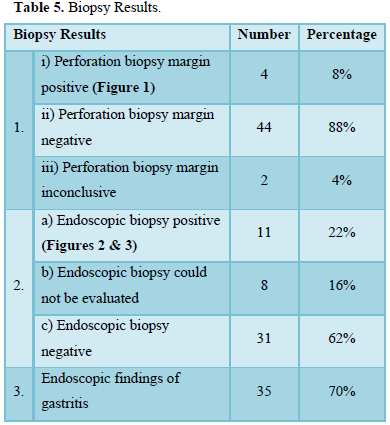
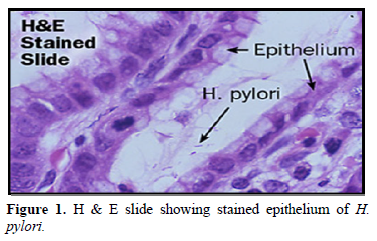
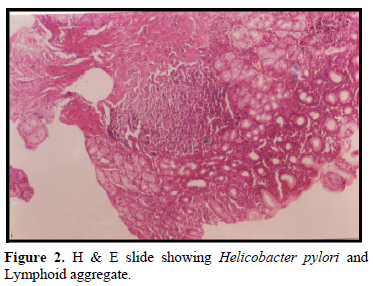
- pylori is intensely antigenic and secretes number of enzymes & chemicals including urease, catalase, mucinase, lipase, phosphates A, hemolysin and alkaline phosphatase, some of which reduce the viscosity of mucus. The production of catalase protects the bacterium against the toxic effects of reactive oxygen metabolites formed in neutrophils. H. pylori incidence is extremely high in first few years of life approaching 10% per annum. The prevalence may rise to over 80% in young adults, whereas in the Prevalence in India is approximately 80%-90% in patients with duodenal ulcer. H. pylori is present in 60-70% of patients with non-ulcer dyspepsia [5]. H. pylori can be stained by various staining processes, such as Warthin starry silver stain, Giemsa stain, hematoxylin - eosin, acridine orange, greenish or brown- Hopps staining.
OBJECTIVES OF STUDY
- Histopathological evaluation of pylori in Perforated peptic ulcer cases (Primary).
- To study demographic profile of Perforated peptic ulcer cases (Secondary).
- Prevalence of pylori in perforated peptic ulcer cases.
MATERIALS AND METHODS
A period-based study was conducted for a period of two years on 50 cases of perforated gastric or duodenal ulcer managed by simple closure and omentopexy [6] in the Department of Surgery.
Type of study: Prospective Study
Exclusion Criteria
- Patients having some other associated pathology like tuberculosis, pancreatitis, ileal or colonic perforation.
- Patients having peptic perforation due to some trauma or penetrating injury of abdomen or due to some corrosive poisonings were also excluded.
- Patients who had received anti pylori regimen, preoperatively or post operatively.
Sample Size: It was a two-year study and 50 cases of perforated peptic ulcer were operated in this two-year period.
Method
- After the presumptive clinical diagnosis of peptic ulcer perforation, patients were resuscitated and taken up for surgery.
- All patients were given IV fluids, metrogyI and third generation cephalosporins.
- Intra-operatively, perforation margins were taken for histopathology and perforation was closed with 3’0’ mersilk suture and an omental patch was stitched over it.
- Post operatively all patients were put on appropriate antibiotics.
- On follow up, patients were put on H-2 blockers.
- Endoscopic biopsy was done after one month from the gastric antrum for presence of pylori.
- The biopsy material was examined with haematoxylin and eosin staining for presence of pylori.
OBSERVATIONS AND RESULTS
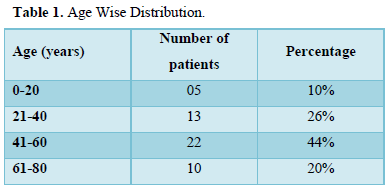
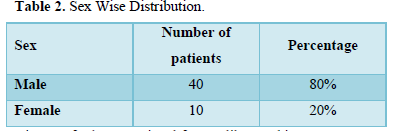
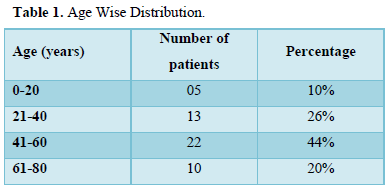
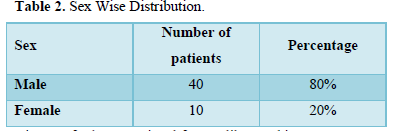
Various observations and results are described as following (Tables 1 & 2)
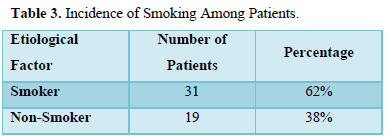
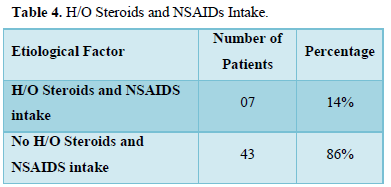
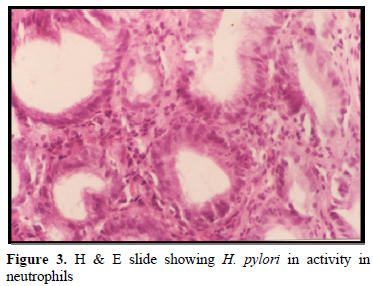
History of other associated factors like smoking was present in 62% patients which is significant (Table 3) and history of Steroids/NSAID intake was present in 14% case (Tables 4 & 5).
DISCUSSION
The older age of presentation, the increased association with non-steroidal anti-inflammatory drugs, associated increased debility, and resulting higher mortality in the elderly are causing a rethink in the management protocol. Years ago, discussions were on the role of early definitive surgery in peptic ulcer perforation, whereas nowadays most of the studies are on the role of anti H. pylori treatment and minimally invasive surgery. A deliberative approach, where in not all patients require surgery, is detailed and there may be an increasing role for laparoscopic perforation sealing techniques in the remainder.
Perforation is the commonest complication of duodenal ulcer. H. pylori is found in 95% patients with duodenal ulcer. However, there is paucity of reports on the prevalence of H. pylori infection in patients with duodenal ulcer perforation. We therefore studied the incidence of H. pylori infection in patients with duodenal ulcer perforation, undergoing laparotomy with repair.
In the present study of 50 consecutive patients of duodenal ulcer perforation who presented in our emergency, the data collected is as follows.
About 44% of the patients were in the age group of 41 to 60 year followed by 36% in less than 40 years and only 20% of patents were in age group of more than 60 years. Majority of the patients were males with a male-female ratio of 4:1.
In 8% of the patient’s positive history of smoking and alcoholism was elicited. About 64% of the patients presented within 48 h from the onset of pain and remaining 36% after 48 h.
32% of the patients had positive history of peptic ulcer symptoms in the form of either burning sensation in epigastrium dyspepsia, flatulence or post prandial fullness. History of intake of non-steroidal anti-inflammatory drugs and steroids was found to be positive in only 14% of patients.
About 20% of the patients had positive history of hypertension/ diabetes mellitus/ ischemic heart disease/ chronic medical illness. All the patients underwent the laparotomy with simple closure of perforation with omental patch only [6].
In majority of patients the per operative biopsy of the perforation margin was found to be negative for H. Pylori staining (88%). In only 8% of the patients, biopsy was positive and remained 4% of the patients had inconclusive report. 62% of the antral biopsies in the post operate period were negative for H. pylori only 22% of the patients stained positive for H. pylori and the remaining 16% of the patients were lost to follow up.
In [7], studied 80 patients of perforated peptic ulcer with mean age of 52 years and concluded that H. pylori was not associated with acute perforated duodenal ulcer. He had used the ferium Anti H. pylori IgG antibody titer and C-14 Urea Breath test at 4 to 10 weeks post operatively to evaluate for the positivity of H. pylori whereas in this present study we used H & E staining of the biopsy and visualization of H. pylori under microscope as the criteria for the positivity of H. pylori.
In [8] studied in 29 patients using C-13 Urea breath test at 8th day and after 6 weeks and found high incidence of H. pylori infection and associated high rate of duodenal ulcer persistence thus concluding the role of H. pylori to be positive in peptic ulcer perforation and suggested that anti H. pylori therapy be given to all patients of peptic ulcer perforation. In our study, we used different diagnostic criteria i.e., perforation margin biopsy and endoscopic biopsy after one month for assessing the H. pylori status which showed that 88% of patients were negative for H. pylori.
In [9] did a similar study in 36 patients of perforated peptic ulcer. He took endoscopic biopsies and concluded perforated ulcer patients were a heterogenous group with a recurrent ulcer disease mainly in patients with H. pylori. In our study, gastritis on endoscopic examination in post operative period persisted in 70% of patients irrespective of H. pylori positivity (22% patients) suggesting role of other factors to be taken into consideration in cases of peptic ulcer perforation.
In [3] took intra-operative antral biopsies in 73 patients via a gastroscope and noted younger age group being H. pylori positive with male preponderance, had less NSAID consumption and more prolonged dyspepsia. He concluded that H. Pylori played an important role and endoscopic biopsy from the antral region was more sensitive in detecting H. Pylori positive cases than the perforation margin.
In [5] also did a similar study in perforated duodenal ulcer, complicated duodenal ulcer patients and non-ulcer dyspepsia patients. He took antral biopsies and noted that none of the perforated duodenal ulcer patient tested positive for H. pylori though all fifteen patients with perforated duodenal ulcer had histological gastritis arising in post operative period. The results were almost similar to our study with H. pylori positive in only 22% of patients. This shows the geographic similarity of the low prevalence of H. pylori in this Northern region of India being less common as cause for H. pylori perforation.
In [10] published on the role of H. pylori in perforated duodenal ulcer. Earlier reports on the association between H. pylori and perforated duodenal ulcer in the nineties suggested that the prevalence of H. pylori was high in patients with perforated duodenal ulcer.
With the association of H. pylori infection with perforated duodenal ulcer postulated by many studies, attention was focused on the effect of eradication of the organism on the ulcer recurrence following simple closure of perforated duodenal ulcer. In an earlier study from our institute on a prospective group of 202 patients and a retrospective group of 60 patients who had undergone simple closure of perforated duodenal ulcer it was found that at every interval of follow-up H. pylori infection rate was significantly higher in patients who had recurrent or residual ulcer. suggested that an immediate and appropriate H. pylori eradication therapy for perforated duodenal ulcers reduces the relapse rates after simple closure. In a recent study on 150 patients with perforated duodenal ulcer following simple closure included on a prospective basis, we found that presence of recurrent ulcer was 18.6% in the eradicated patients when compared to 70% in non-eradicated patients suggesting that H. pylori eradication reduces risk of ulcer recurrence after simple closure.
In a recent systematic review and meta-analysis on H. pylori eradication therapy after simple closure of perforated duodenal ulcer, the pooled incidence of 1-year ulcer recurrence in the H. pylori eradication group was 5.2% (95% confidence interval (CI) of 0.7 and 9.7), when compared with that of the control group (35.2%) with 95% CI of 0.25 to 0.45. The pooled relative risk was 0.15 with 95% CI of 0.06 to 0.37. The authors concluded that H. pylori eradication after simple closure of duodenal ulcer perforation gives better results than antisecretory non-eradication therapy for prevention of ulcer recurrence and hence should be recommended for all infected patients.
From all the previously mentioned data it appears that H. pylori infection does play an important role in perforated duodenal ulcer and eradication is recommended in all infected patients following simple closure to prevent ulcer relapse.
In [11] conducted a study to determine the prevalence of H. pylori in patients with DUP patients as compared to normal healthy volunteers (NHV). Eighty-six consecutives’ patients with DUP and 30 NHV were included in the study. The NHV, drawn from the Surgery outpatient, were subjected to upper gastrointestinal (UGI) endoscopy and multiple gastric mucosal biopsies. Gastric mucosal biopsies among patients with DUP were obtained during laparotomy by passing a biopsy forcep through the perforation site. Biopsy specimens were put in urea broth for the rapid urease test (RUT), brucella broth (used as a transport medium) for culture and 10% formalin for histopathology. The results were analyzed as the percentage of positive cases. The mean (+/-SD) age of patients with DUP (39.4+/-15.5 years) and of the NHV (36.0+/-13.9 years) were comparable (p= 0.290). Sixty-one (70.9%) patients with DUP had used NSAIDs prior to perforation. Only 7 patients with DUP (8.14%) had a past history of symptoms of duodenal ulcer and had been treated for it. A positive history of smoking, alcoholism and tobacco use was present in 68 (78.9%), 59 (68.6%) and 41(47.7%) patients with DUP, respectively. No culture was positive. Histology was positive for H. pylori in 29 patients with DUP and in 2 (6.7%) NHV. RUT was positive for H. pylori in 43(50%) patients with DUP and 5 NHV (16.7%). The present study documented a markedly higher association of H. pylori infection with perforated duodenal ulcer.
In [12] shows that the prevalence of H. pylori infection among patients presenting with a PPU was 12.5%. Among them, 87.5% had a perforation in the pre-pyloric region and12.5% were in the first part of the duodenum. The prevalence of H. pylori infection among patients with PUD was 31.3%. This was based on the rapid urease test and histopathological examination. The results were statistically significant with a p-value of 0.026 when H. pylori was considered as an exposure factor, and with an odds ratio (OR) of 0.31; we found that H. pylori infection was not significantly associated with PPU. This is similar to the study done by Gisbert [13] in which the prevalence of H. pylori infection in PPU was significantly less with an infection rate of 47% [13]. They found that chronic recurrent PUD and PPU have different pathogenesis based on the fact that there is a low prevalence of H. pylori infection in patients presenting with PPU. It also suggests that other pathogenic factors might also play a role in PPU. Also, another study done by Gisbert [13] found that all their 15 patients with PPU were negative for H. pylori. But in contrast to our study, most other studies showed a significant association of H. pylori infection with PPU. The discrepancy in the infection rates found in the literature may be attributed in part to the different populations studied. In the present study, 45.8% of patients in group I were smokers, among which 13.63% tested positive for H. pylori. In group II, only 16.66% were smokers of which only one patient was tested positive for H. pylori infection. Alcohol intake is another attributable risk factor for PPU. In the present study, 56.3% of PPU patients had a history of alcohol intake and among them, two were tested positive for H. pylori. In PUD patients, 25% had a history of alcohol consumption of which five were found to be positive for H. pylori. The results were statistically significant (p: 0.002) when alcohol intake and smoking were considered as risk factors for PPU. Based on the OR (3.85 and 4.23, respectively), it was found that both alcohol intake and smoking were risk factors for PPU. This was similar to a study done by Ugochukwu which showed that smoking and alcohol consumption were significantly associated with perforation in young men from developing countries. Previous studies that show a significant association between H. pylori infection and PPU are listed below (Table 5) [8,9,12,14]. Study Year Prevalence of H. pylori infection in PPU, % Association Ugochukwu 2013 65-70 Significant Dogra 2014 92 Significant John B 2017 47 Significant Sebastian 2001 83.3 Significant.
The main problem with biopsy for H. pylori was potential sampling error which may occur due to the patchy distribution of H. pylori in the gastric mucosa. This makes endoscopy dependent tests relatively insensitive especially in the presence of scanty infection. The predictive value of diagnostic tests for H. pylori could be improved by taking more than one biopsy sample or by using more than one endoscopy dependent test at the sometime. Diagnosis of the presence of H. pylori by histology tends to be inaccurate especially in the presence of scanty infection. Despite the low diagnostic sensitivity of the test, histology was available for investigating the histopathologic process involved in infection with H. pylori. The patients detected as H. pylori positive from the gastric antrum endoscopic biopsy were more i.e., 11 than the perforation margin biopsy i.e., 4 suggesting that H. pylori is not related to the local changes in the perforated gut leading on to perforation. It is not surprising that that acid reduction surgery has been successful in decreasing the recurrence ulcer rate in patients with perforated duodenal ulcer. Eradication of H. pylori from stomach is associated with remission of ulcer disease warranting reconsideration of surgical treatment protocols using ulcer definitive surgery [14]. There is now a tendency towards minimalistic approach like simple closure of perforation by laparoscopy rather than by laparotomy. We have shown in the present study, that perforated peptic ulcer was not associated with H. pylori and has multiple risk factors and causations. Confirmation of fact that recurrence of ulcer disease was not related to the type of surgery performed rather related to H. pylori; needs a randomized trial, to compare the ulcer recurrence rates after simple closure versus eradication of H. pylori with acid reduction surgery [14].
CONCLUSION
We concluded that H. pylori was not detected in patients with peptic ulcer perforation in our belt. Role of smoking/alcoholism cannot be undermined as shown in above study (62% positive cases). History of drugs (non-steroidal anti-inflammatory and steroids) intake was found positive in 14% of cases. This study clearly suggests that there are multiple causes and other important associated factors to be taken into consideration in cases of peptic ulcer perforation in our belt. Laparotomic/Laparoscopic simple closure of the perforation with omental patch should be done in perforated duodenal/pyloric/gastric ulcer. In patients positive for H. pylori; eradication.
- Shwartz, Stanley WA, Denis E, John MD (1999) Principles of Surgery. 7th ed USA McGraw Hill, Chapter 24, Stomach 1191.
- Graham DY, Adam E, Reddy GT, Agarwal JP, Agarwal R, et al. (1991) Seroepidemiology of Helicobacter pylori infection in India. Comparison of developing and developed countries. Dig Dis Sci 36: 1084-1088.
- Ng EK, Chung SC, Sung JJ, Lam YH, Lee DW, et al. (1996) High prevalence of pylori infection in duodenal ulcer perforations not caused by NSAIDs. Br J Surg 83: 1779-1781.
- Matsukara N, Onda M, Tokonaga A, Kato S, Yoshiyuki T, et al. (1997) Role of pylori in perforation of peptic ulcer: An age and gender matched case control study. J Clin Gastroentrol 25 1: S235-S239.
- Chowdhary SK, Bhasin DK, Panigrahi D, Malik AK, Kataria RN, et al. (1998) pylori infection in patients with perforated duodenal ulcer. Trop Gastroenterol 19: 19-21.
- Rintoul RF, Macintyre IMC, Johnstone JMS (2014) Farquharsons Textbook of Operative Surgery. 10th ed Edinburgh: Churchill livingstone. Chapter 17 Stomach and duodenum. pp: 387-390.
- Reinbach DH, Cruickshank G, Acute, McColl KE (1993) Acute perforated ulcer is not associated with pylori infection. Gut 34: 1344-1347.
- Sebastian M, Chandran VP, EL Elashaal YI, Sim AJ (1995) pylori infection in perforated ulcer disease. Br J Surg 82: 360-362.
- Debongnie JC, Wibin E, Timmermans M, Mairesse J, Dekoninck X, et al. (1995) Are perforated gastroduodenal ulcers related to pylori infection. Acta Gastroenterol 58: 208-212.
- Kate V, Ananthakrishnan N, Tovey FI (2013) Is Helicobacter pylori Infection the Primary Cause of Duodenal Ulceration or a Secondary Factor? A Review of the Evidence. Gastroenterol Res Pract pp: 1-8.
- Kumar S, Mittal GS, Gupta S, Kaur I, Aggarwal S, et al. (2004) Prevalence of Helicobacter pylori in patients with perforated duodenal ulcer. Trop Gastroenterol 25: 121-124.
- Thirupathaiah K, Jayapal L, Amaranathan A (2020) The Association Between Helicobacter Pylori and Perforated Gastroduodenal Ulcer. Cureus 12: e7406.
- Gisbert JP, Legido J, Garcia-Sans, Pajares JM (2004) Helicobacter pylori and perforated peptic ulcer prevalence of the information and role of non-steroidal anti-inflammatory drugs. Dig Liver Dis 36: 116-120.
- Souza FO, Dalcin SR, Dalcin RP, Abaid CA, Almeida PM, et al. (2009) Ten years comparative study after surgical treatment of perforated peptic ulcer according to ulcer relapse between pylori positive, after eradication and negative patients. ABCD Arq Bras Cir Dig 22: 15-18.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)





