Research Article
Use of Three Point Index as A Predictor of Outcome in Pediatric Forearm Fractures: A Prospective Study
3287
Views & Citations2287
Likes & Shares
Pediatric diaphyseal both bone forearm fractures are the third most common fracture in the pediatric population and account for 13-40% of all pediatric fractures. There are many modalities of definitive treatment vis a vis conservative casting and operative management in form of intramedullary flexible nails or plating. While conservative management has the risk of redisplacement of fractures, operative management has the risk of incision scar formation, infection and requirement of second surgery for removal of implants which are inherent to any surgical form of treatment. Pediatric population has the potential of remodeling and conservative management is still the gold standard treatment in management of these fractures if correctly applied. We conservatively managed the cases of pediatric both bone forearm fractures and evaluated the three-point index (TPI) in the skiagram and found a sensitivity of 85% and specificity of 90 percent in predicting redisplacement in cases wherein TPI was more than 0.8. Our study concluded with a recommendation of usage of TPI in all cases pertaining to these fractures in pediatric population.
Keywords: Pediatric diaphyseal, Intamedullary flexible nails, Skiagram, Pediatric population
Abbreviations
TPI: Three point index
INTRODUCTION
Pediatric diaphyseal fractures of the radius and ulna, commonly referred to as both bone forearm fractures, are the third most common fracture in the pediatric population and account for 13-40% of all pediatric fractures [1,2]. Ulna is relatively straight whereas radius has a bow and rotates over ulna during supination and pronation. Much of the growth occurs at the lower end of both bones of forearm.
Most forearm injuries are the result of indirect trauma. A fall on an outstretched hand coupled with a rotational component to produce fracture is common. The goal of forearm fracture treatment is to restore appropriate length, alignment, and rotation to allow normal function after completion of remodeling and healing [3].
Fracture severity falls along a continuum from plastic deformity to significant displacement. Historically, the majority of these fractures have been treated with non-operative management relying on closed reduction and casting. Recently, however, there has been a trend towards increased surgical management of these fractures in an effort to improve clinical outcomes [4].
NON-SURGICAL MANAGEMENT
Normal function is often achieved with closed reduction and casting. Because of children’s ability to remodel, especially if more than two years of growth is left, some amount of angulation and translation is acceptable. Most authors concur with the recommendations from Noonan and Price with angulation of 10-15° and malrotation of 30° [5].
Conservative methods still play a major role in treatment and 85% of these patients achieve satisfactory results with these methods [6,7]. Loss of fracture reduction is the most commonly reported complication of manipulated distal forearm fractures and, up to one third of cases will demonstrate late displacement [8]. Maintaining acceptable reduction inside the cast is difficult in some cases and re-displacement may occur. Exact and repeated radiological checks are necessary because early identification will prompt additional treatment, which will prevent further complications [8,9].
Although the remodeling potential of these fractures is well recognized, up to 30% of these fractures exhibit significant redisplacement requiring further treatment. In order to avoid the morbidity of re-manipulation, a number of radiological indices that have been developed to differentiate between the well and poorly applied plaster casts and to assess the quality of molding, in order to predict fracture redisplacement in plaster casts [10].
RATIONALE BEHIND THE TPI
The TPI was originally designed according to the basic principles of cast treatment: Three-point fixation and reduction accuracy in terms of the contact area of the fragments in the fracture site (Figure 1) [11].
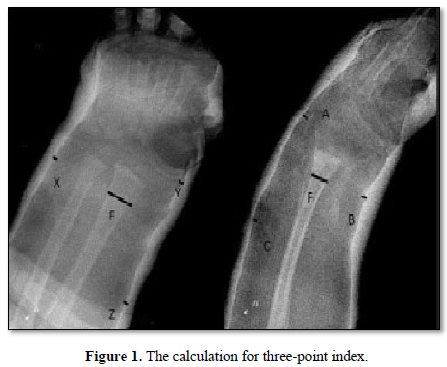
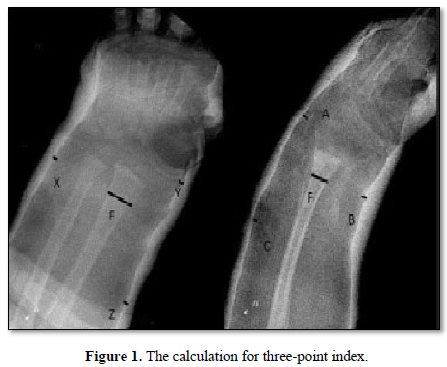
The critical gaps were selected on the basis of the most important points in the cast that maintain the reduction against the common displacement forces. On an AP radiograph, ‘Y’ should be the narrowest radial-side gap between the cast and the skin around the radiocarpal joint or at the level of the scaphoid bone; ‘X’ should be the narrowest ulna-side gap between the cast and the skin within 1 cm of the fracture line; and ‘Z’ should be the narrowest radial-side gap about 3-5 cm proximal to the fracture site [7].
On a lateral view, ‘A’ should be the narrowest dorsal-side gap between the cast and the skin around the radio-carpal joint or the proximal carpal row; ‘B’ should be the narrowest volar-side gap between the cast and the skin within 1 cm of the fracture line; and ‘C’ should be the narrowest dorsal-side gap about 3-5 cm proximal to the fracture site [7].
Dividing the sums by the contact length of the fracture fragments in each plane provides proportionality for the index, which prevents measurement errors due to magnification of the plain radiographs [7].
METHODOLOGY
90 cases of pediatric diaphyseal fractures were included in the study in the age group of 3-10 years with a single level of fracture. Comminuted fractures segmental fractures, compound injuries, injuries which are contraindications to conservative management like evidence of compartment syndrome etc. were excluded from the study.
The reduction of the fracture was done under sedation/Short GA under the guidance of image intensifier and reduction was achieved using traction, manipulation of fragments, maintenance of interosseous space etc and standard above elbow cast was applied with elbow in 90° flexion and supinated position in proximal third fractures and pronated position in distal fractures . We generally used POP casts in these cases as better molding could be achieved via the same as compared to a fiberglass.
Post reduction Skiagram was done and TPI was calculated. Serial skiagrams were done at the end of first week first month and 2nd month just prior to cast removal and protected weight bearing and physiotherapy started thereafter.
Failure of reduction was defined as >15° angulation in AP or Lateral radiographs or displacement of fracture fragments leading to less than 25% contact between fracture ends.
RESULTS
Out of the 90 cases which were included in the study only 13 cases had a loss of reduction and were treated operatively with open reduction/closed reduction and intramedullary physis sparing elastic nails. We generally do not do plating for these fractures at our institute.
Out of those 13 cases 4 cases had displacement of one bone only and in 9 cases both the bones were displaced. The mean three-point index in the displaced group was 1.04 and in the non-displaced group was 0.68. The sensitivity in predicting displacement was 84.61% and specificity in non-displaced cases was 90%.
The Odds ratio was 48.12. The Positive predictive value in predicting displacement was 58% while negative predictive value in predicting non displacement was 97%, implying the usefulness of this index in predicting non displacement of fracture.
There was no difference in outcome due to age or sex of the patient, experience of the surgeon, initial displacement.
DISCUSSION
Out of the total 90 patients analyzed in the study, 13 patients had significant redisplacement and required remanipualtion. This rate of redisplacement was comparable to previous studies on the subject [6,7].
No significant association was seen between age, sex, or side of injury with redisplacement as has been seen in previous studies [6,7].
Initial angulation or prereduction angulation has been reported as a risk factor by Mazzini et al. [11]. However, for current series, no difference was seen between the patients with acceptably reduced fractures and significantly redisplaced fractures as also seen previously [6,7]. Angulation only suggests bending of bones without complete disruption of periosteum. Due to this intact periosteal sleeve, intrinsic stability of fracture is maintained. Hence, there is less chance of redisplacement.
The mean TPI in patients with redisplaced fractures was 1.04 while for acceptably reduced fractures it was 0.68. This difference was statistically significant. When its validity was assessed as a predictor of redisplacement with a cutoff of 0.8, it proved to be a significant predictor. The sensitivity (85%) and specificity (90%) of TPI makes it a useful predictor of redisplacement in these fractures which is also supported the findings of Alemdaroğlu et al. [7]. TPI is a sensitive predictor of redisplacement in these fracture cases although its use is somewhat restricted by complex calculations needed.
The present study had limitations of single-center recruitment, use of non-synthetic padding which may have thickness variations, with no comparisons between synthetic and non-synthetic padding material, cast material (POP vs. fiberglass), type of anesthesia used (conscious sedation vs. GA). The strengths of the study were this being a prospective study including both diaphyseal and metaphyseal fractures with well-defined inclusion and exclusion criteria, acceptability of reduction, redisplacement and indications of remanipulation.
CONCLUSION
We conclude that conservative management by closed reduction and cast well molded is still the management of choice in closed pediatric forearm fractures. TPI should be routinely used as a predictor for assessment of redisplacement in these cases.
- Cheng JC, Ng BK, Ying SY, Lam PK (1999) A 10-year study of the changes in the pattern and treatment of 6,493 fractures. J Pediatr Orthop 19: 344-350.
- Jones K, Weiner DS (1999) The management of forearm fractures in children: a plea for conservatism. J Pediatr Orthop 19: 811-815.
- Pace JL (2016) Paediatric, adolescent forearm fractures: Current controversies and treatment recommendations. J Am Acad Orthop Surg 24: 780-788.
- Flynn JM, Jones KJ, Garner MR, Goebel J (2010) Eleven years’ experience in the operative management of pediatric forearm fractures. J Pediatr Orthop 30: 313-319.
- Noonan KJ, Price CT (1998) Forearm and distal radius fractures in children. J Am Acad Orthop Surg 6: 146-156.
- Hove LM, Brudvik C (2008) Displaced pediatric fractures of the distal radius. Arch Orthop Trauma Surg 128: 55-60.
- Alemdaroglu KB, Iltar S, Çimen O, Uysal M (2008) Risk factors in redisplacement of distal radial fractures in children. J Bone Joint Surg 90: 1224-1230.
- Bae DS (2008) Pediatric distal radius and forearm fractures. J Hand Surg 33A: 1911-1923.
- Reichmann W (1978) Distal radial fracture in childhood. Handchirurgie 10: 179-181.
- Bhatia M, Housden P (2006) Redisplacement of paediatric forearm fractures: Role of plaster moulding and padding. Injury Int J Care Injured 37: 259-268.
- Mazzini JP, Beck N, Brewer J, Baldwin K, Sankar W, et al. (2012) Distal metaphyseal radius fractures in children following closed reduction and casting: Can loss of reduction be predicted? Int Orthop 36: 1435-1440.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Spine Diseases
- Journal of Alcoholism Clinical Research
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)



