4399
Views & Citations3399
Likes & Shares
Purpose: To describe the surgical outcome of a patient that developed a presumed Posner-Schlossmann Syndrome a week after uneventful Small Incision Lenticule Extraction (SMILE)
Methods: Case report.
Results: A 38-year-old man underwent bilateral SMILE for myopic correction. At the 1-week postoperative visit, he complained of blurred vision in OS. Slit lamp exam revealed mild anterior chamber reaction, small inferior iris atrophy, corneal interface opacity and edema, deep anterior chamber with open angle in OS, and IOP was 46 mmHg. Despite clinical treatment with steroids and glaucoma medication, the patient did not achieve a desired IOP and his visual field started to show nerve damage. He underwent a deep non penetrating sclerotomy in OS. The surgery was uneventful and the IOP reduced to 8mmHg and maintained this level.
Conclusions: This is the first case report of presumed Posner-Schlossmann Syndrome after SMILE. The report demonstrates corneal haze and interface edema with corneal thickening.
INTRODUCTION
Posner-Schlossmann Syndrome (PSS) is a disease described by recurrent, unilateral, acute attacks of mild, anterior non-granulomatous uveitis associated to markedly elevated intraocular pressure (IOP) [1].
Small incision lenticule extraction (SMILE) is a current form of femtosecond laser lenticule extraction refractive surgery. However, some complications can occur after surgery. We report a presumed case of PSS after uneventful SMILE, discuss its possible mechanism and describe the treatment and outcome for this condition.
CASE REPORT
A 38-year-old caucasian man with no significant medical or ocular history and a stable refraction underwent bilateral uneventful SMILE. Preoperative manifest refraction was -5.00 sphere in OD and -5.00 sphere in OS, with corrected distance visual acuity (CDVA) of 20/20 in both eyes. Preoperative exams included corneal topography, tomography, slit lamp and fundus exam, all within normal limits. SMILE was performed using VisuMax femtosecond laser (Carl Zeiss Meditec, Jena, Germany). Surgery was uneventful and postoperatively the patient received a combination of antibiotic and steroid drops (Zypred; Allergan, Irvine, CA) four times daily for 1 week.
The patient achieved an uncorrected distance visual acuity (UDVA) of 20/25 in both eyes on the first postoperative day. However, he presented 10 days later with a reduced visual acuity of 20/200 in his left eye. The surgeon restarted the drops (Zypred; Allergan, Irvine, CA) four times daily and, since the patient did not notice any visual improvement, he came to our service for a second opinion.
On presentation at our institute the patient was at his 2 month-postoperative visit. His UDVA was 20/25 in OD and 20/400 in OS. Manifest refraction was OD: +0.50 -0.50 x 95 with CDVA of 20/20; and OS: -2.00 -0.75 x 165 with CDVA of 20/100. At the slit lamp examination, we observed in OS mild anterior chamber reaction, small inferior iris atrophy, corneal interface opacity and edema, deep anterior chamber with open angle (Figure 1A, B). AS-OCT revealed interface opacity and corneal edema with changes in corneal curvature when compared to 1 day postoperative (Figure 1C). The intraocular pressure (IOP) measured with Goldmann applanation tonometer was 12 mmHg in OD and 46 mmHg in OS. Fundus exam, macular Optical Coherence Tomography (OCT) and optic nerve OCT were normal. Gonioscopy confirmed an open angle 360 (Figure 1D).
We started immediately topical prednisolone acetate 1% (Pred Fort; Allergan, Irvine, CA) every 3 h, topical association of timolol and dorzolamide (Cosopt) twice a day and oral acetazolamide (Diamox) four times a day. A thorough clinical examination and laboratory testings were performed in order to rule out any systemic disease that could cause anterior uveitis. IgM and IgG serologies came negative for HSV, CMV. The patient was followed weekly and his IOP decreased to 32 mmHg in OS. After 15 days with no further IOP reduction, we changed his topical medication to association of timolol and brinzolamide (Azorga; Alcon Laboratories, Fort Worth, TX) and introduced topical brimonidine (Alphagan Z, Allergan, Irvine, CA) three times a day, continued with oral acetazolamide and decreased steroids to once a day. Two weeks later his IOP decreased to 25 mmHg and maintained this level for a month.
Since the patient did not achieve a desired IOP with full glaucoma medication and his visual field started to show nerve damage (Figure 2), a surgical approach was indicated. The patient underwent a deep non penetrating sclerotomy in his left eye. The surgery was uneventful and IOP reduced to 8mmHg and maintained this level since then with no need of topical medication. At this time aqueous humor was collected in order to perform PCR for viral infection and it came back negative.
One month after non penetrating sclerotomy, UDVA in OS improved to 20/25, corneal curvature went back to initial postoperative values and corneal interface opacity decreased significantly.
A statement of consent to publish this case was gathered from the patient, as well as consent to publish exams and images.
DISCUSSION
Posner-Schlossman Syndrome (PSS) was first described by Posner and Schlossman in 1948 [2]. The key features for this disease are recurrent episodes of mild cyclitis, typically unilateral, corneal edema with decreased visual acuity, high IOP usually from 40-70 mmHg during the attack, open angles, fine keratic precipitates and mydriasis [3].
The pathophysiology is still not known. Possible etiologies include infections such as Herpes Simplex (HSV), cytomegalovirus (CMV), Helicobacter Pylori, or autoimmune diseases (positive HLA-Bw54 association in some cases) [4-8].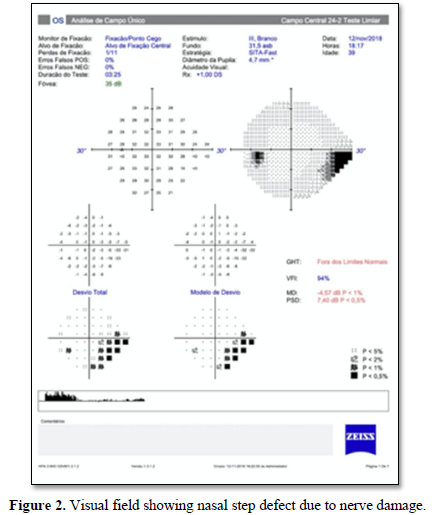
On exam, the patient presents with unilateral mild ocular discomfort and blurred vision. Ocular inflammation usually occurs several days after elevated IOP, which is out of proportion to the amount of anterior chamber inflammation [2]. During the attacks of IOP elevation, the optic nerve can experience significant morphological changes, as well as decreased perfusion due to the acute rise in IOP. The transient changes do not always lead to permanent damage, but optic nerve and visual field damage have been reported after repeated attacks [2].
Wang and coworkers described a case of PSS after LASIK, but in their patient developed uveitis 1 year after surgery. In our case, the patient developed PSS 10 days after surgery, with no previous history of uveitis. One of the hypotheses for the PSS could be the surgical trauma that could lead to inflammation since prostaglandins are believed to play a role in glaucomatocyclitic crises [9].
The patient described in this report had not experienced a glaucomatocyclitic crises prior to surgery and all laboratory tests came back negative (HVS, CMV serologies, as well as tests to rule out other causes of uveitis such as tuberculosis, toxoplasmosis and rheumatological diseases). This was the first and only episode and, despite all efforts to control clinically the IOP, the patient needed surgical therapy. After the procedure, IOP went back to normal values and maintained stable, corneal curvature reduced and visual field improved.
This presumed case of PSS developed after SMILE, despite being rare, is a condition that needs to be considered when patients developed high IOP postoperatively. The inflammation can be so mild as to be unnoticed, so the aetiology of the rise in IOP may not be clear at first presentation.
CONFLICT OF INTERESTS
The authors declare that there is no conflict of interests in anything discussed in this case report.
- Posner A, Schlossman A (1948) Syndrome of unilateral recurrent attacks of glaucoma with cyclitic symptoms. Arch Ophthal 39: 517-535.
- Wang L, Yin G, Wang D, Yu Z (2017) Posner-Schlossman syndrome: A 10-year review of clinical experience. Ann Eye Sci 2.
- Choi CY, Kim MS, Kim JM, Park SH, Park KH, et al. (2010) Association between Helicobacter pylori infection and Posner-Schlossman syndrome. Eye 24: 64-69.
- Takusagawa HL, Liu Y, Wiggs JL (2011) Infectious theories of Posner-Schlossman syndrome. Int Ophthalmol Clin 51: 105-115.
- Yamamoto S, Pavan-Langston D, Tada R, Yamamoto R, Kinoshita S (1995) Possible role of herpes simplex virus in the origin of Posner-Schlossman syndrome. Am J Ophthalmol 119: 796-798.
- Bloch-Michel E, Dussaix E, Cerqueti P, Patarin D (1987) Possible role of cytomegalovirus infection in the etiology of the Posner-Schlossmann syndrome. Int Ophthalmol 11: 95-96.
- Teoh SB, Thean L, Koay E (2005) Cytomegalovirus in aetiology of Posner-Schlossman syndrome: Evidence from quantitative polymerase chain reaction. Eye (Lond) 19: 1338-1440.
- Markomichelakis NN, Canakis C, Zafirakis P, Marakis T, Mallias I (2002) Cytomegalovirus as a cause of anterior uveitis with sectoral iris atrophy. Ophthalmology 109: 879-882.
- Wang X, Lim EWL, Lim L, Wei RH (2017) Posner-Schlossmann syndrome induced laser in situ keratomileusis keratoectasia - A case report. Int J Ophthalmol 10: 1617-1619.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Spine Diseases
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)




