Research Article
COMPARISON OF THE BALANCE AND THE AGILITY IN THE STUDENTS 11-14-YEAR-OLD WITH ABNORMALITIES OF THE LOWER EXTREMITY AND NORMAL POSTURE
4012
Views & Citations3012
Likes & Shares
Background: The muscle's strength imbalance often causes Musculoskeletal disorders of incidence. The pattern disorders appear in the dominant and recessive organs and others' body posture. This lack of balance, which affects body alignment, is essential in creating abnormalities. This research aims to study the relationship between deformity lower extremity with some factors of physical fitness.
Methods: In this study, 80 boy students 11-14- years old took part in four groups (each group = 20) Normal Posture, Genu valgum, Genuvarum, and Flat Foot. At first, by measuring the distance between the condyles and Medial malleolus, those with Genuvalgum and Genuvarum were identified, and by Chippaux-Smirak's Index measurement method, those with the arch of Flat Foot identified. A Healthy posture group is also selected from people outside this number. Then, physical fitness variables, including Agility, static balance, and dynamic balance, were measured. ANOVA test was applied to compare the variables of fitness and abnormalities of the lower extremity between groups.
Results: It showed a meaningful and significant difference in the Static Balance (P=0.001), Dynamic Balance (P=0.001), and Agility (P=0.001) of Healthy individual students and patients with abnormalities.
Conclusion: Considering the importance of the relationship between the situation abnormalities and physical performance in people suffering from these abnormalities, the importance of identifying and preventing them with the programs of corrective postures and the promotion of physical fitness is highly emphasized.
Keywords: Balance, Abnormalities, Agility, Flat Foot, GenuValgum, GenuVarum
Abbreviations
CP: Correct Posture; ICP: Incorrect Posture; COG: Center Of Gravity; CSI: Chippaux-Smirak’s Index; BF: Biceps Femoris; RF: Rectus femoris; BMI: Body Mass Index; QDT: Quadriceps' Direction Tendon.
BACKGROUND
One of the most important indexes of general health is having a correct posture (CP), having a proper alignment structure. One of the most important goals of science is human health study. As one of the health and fitness trustees, Physical education and sport science deal with this vital issue through motor activity (Winwood, Keogh, & Harris, 2012). Maintaining the body's natural alignment against internal and external forces can be called musculoskeletal balance. Musculoskeletal disorders often manifest as imbalances in muscle strength. Postural malalignment may result from unilateral muscle superiority, soft tissue asymmetry, and bone contrast. As a result, movements were performed with poor mechanics. In the body, as a closed chain, each joint's position affects the other joints. The CP is the position where the least pressure is applied to the joints. In CP, muscle activity is at its lowest level. Different situations that put pressure on the joints are discussed as Incorrect Posture (ICP). The ICP consumes a great deal of energy (De Nunzio, Zanetti, & Schieppati, 2009). Body maintenance occurs when the center of gravity (COG) of the various body parts, such as the head, trunk, pelvic, and lower extremity, are in a balanced state. Improper body function causes a great deal of energy loss and increase its organic injuries (Zakeri, Baraz, Gheibizadeh, & Saidkhani, 2016).
Deviation from CP is unpleasant and injures muscle performance, and makes one susceptible to musculoskeletal disorders and neurological disorders (Winwood, Keogh, & Harris, 2012). Maintenance of ICP may lead to chronic ICP. Chronic ICP means that the person most often has an ICP when walking, standing, sitting, which is a cause of muscle weakness and is associated with pain and illness. As a result, imbalance manifested as a postural deviation; the body does adjust to the COG. Often such deviations result in injury; for example, the fixed pattern of knee injury may be related to the asymmetry in the pelvic and foot, not just in the form of compensatory actions (Michael & Trevor, 2009). It has been suggested that changes in tibia anatomical alignment are essential potentials in feedback changes in proprioception and muscle performance, affecting their function in performing activities (Mueller, 2005).
The lower extremities' long bones form angles to each other and to the vertical line, which is called “the axis of the alignment lower extremity." The lower extremity is at three degrees of valgus based on the lower extremity's mechanical axis angle, which is standing inside the feet to the pelvic (Delmonico, Harris, Lee, Visser, Nevitt, Kritchevsky, & Health, Aging and Body Composition Study, 2007). The terms varus and valgus were used to express the Genu valgum knee and the Genu varus knee (Aurélio, Ronaldo, João, Rui, Helena, 2010) and termed the drop of the medial longitudinal arch of the flat foot used in lower extremity deviations (Pamela, & Ghinwa, 2003). Since lower extremity abnormalities are involved in balance disorders, they can cause walking, running, jumping, and necessary motor skills (Uden, Scharfbillig, & Causby, 2017) and physical fitness factors during life. Bouchard and Sheffard define physical activity as the skeletal muscles' physical movement because of increased resting energy expenditure. Christerson and Carsperson define performance as a set of traits that people possess or gain physical activity (Aurélio, Ronaldo, João, Rui, Helena, 2010).
Cassio (2011) reported that neuromuscular and biomechanical factors also influence body posture responses. Alignment posture seems to affect body balance control in the COG. Environmental conditions also affect body posture alignment, affecting stability during activities. Malalignment in organs may cause unnecessary movements in other organs to maintain posture. In this condition, there is a disorder in muscle activity. For example, knee stabilizers, which depend on passive structures and quadriceps activity, are more than necessary (Cassio, 2011). (Ho, Lin, Chou, Su, & Lin, 2000) observed a significant relationship between the angle of rotation of the foot to the outside above 16 0 with velocity, walking time, ground reaction, and ankle mechanical strength (Ian, Gavin, 2009). Kirby et al. (1987) showed that foot positioning at different angles influences the balance of the individuals (Kirby, Price, MacLeod, 1987). The prevalence of abnormalities in students has been over 80% in various studies. Given the great importance of students' performance in physical activity and the potential impact of some lower extremity abnormalities, much research has not been conducted in this area. Therefore, this study tests balance and performance in 11-14 -years old students with lower extremity abnormalities and compares them with Healthy posture students.
PATIENTS AND METHODS
Participants
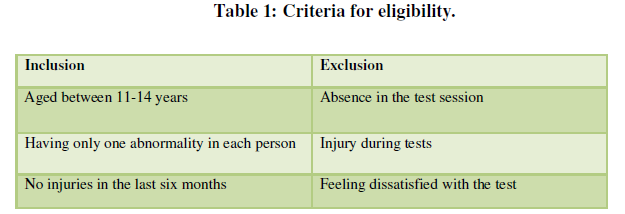
This study's statistical population comprised 11-14-years old boy high school students in Tehran (Iran). The study's statistical sample was purposively selected from the target population, including three randomly chosen schools. Four hundred students in these schools and abnormalities were measured, and students with the desired abnormalities were selected. Finally, 60 subjects were chosen as the primary sample in three groups of Genu valgum knee, Genu varum knee, and flat foot (20 in each group) with abnormalities above average score. Healthy Posture group (n= 20) were the individuals with no abnormalities and selected outside those with abnormalities. Samples with Genu valgum knee abnormalities greater than 4 cm, the Genu varum knee greater than 5 cm, and flat foot over 45% were selected as the study samples. A Static balance was assessed by stork test, dynamic balance by Y balance test, and Agility by 9 * 4 m.
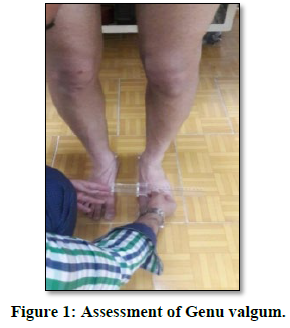
Genu valgum
There are conditions where the knees curved inward while standing. When knees stand together, the legs (medial malleolus) are farther apart. The distance between the medial malleolus of the foot used to measure the genu valgum (Cassio, 2011), in a way, the person standing with no shoes and minimum clothing, their knees and femurs were visible with no muscle contraction. In this way, the knees fully extended and the knees' patella looking forward. Then, the distance between the medial malleolus was measured using a Caliper (if the distance between the two medial malleoli is over 4 cm, the subjects were in the Genu valgum group) (Figure 1) (Shams Abrigh, & Moghaddami, 2020).
GENU VARUM
There are conditions in which the knees are curved outward in the standing position when the medial malleolus are standing together; the knees are farther apart. The distance between the femoral condyle uses to evaluate the Genu varum (Cassio, 2011), whilein that way, the person was standing with no shoes and minimum clothing with visible knees and femurs and without any muscle contraction. In this way, the knees should fully extend, and the medial malleolus should be attached so that the patella is looking forward. Here, the distance between the two condyles measured in the most prominent part with the Caliper in centimeters (if the distance between the two medial condyles is over 5 cm, the individual was in the group of Genu varum knee abnormality) (Figure 2) (Shams Abrigh, & Moghaddami, 2020).

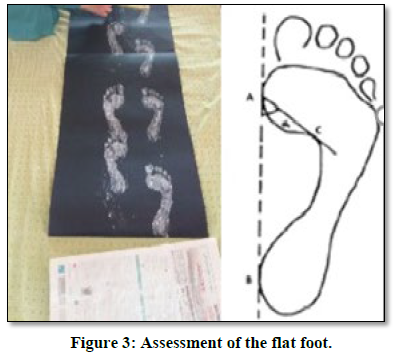
FLAT FOOT
The situation in which the longitudinal arch has fallen or is in full contact with the ground (Chavoshnejad, Ayati, Abbasspour, Karimpur, George, Rémond, & Baniassadi, 2018). Chippaux-Smirak’s Index (CSI) was used to evaluate the flat foot (Flexible). The evaluation method is as follows.
To calculate the CSI, find points A and A' and draw the line AA' (Figure 3).
A: The medial point in the Metatarsal region and
A': The medial point of the Heel.
Then draw line AB (the widest area in the Metatarsal) and line C (the smallest area in the foot arch region) parallel to the line AB. The CSI was then calculated from the smallest arch area ratio to the Metatarsal region's widest arch area.
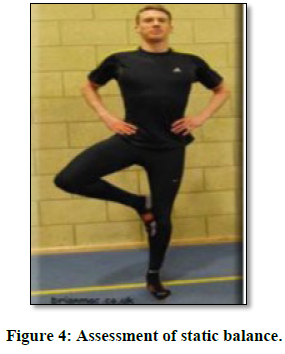
STATIC BALANCE
Stand on one leg test was used to assess static balance. The subject removed those shoes and put to hands-on the iliac crest, then flexed it other foot from the knee and placed his toes on the inside of the other foot knee. The subject then separated from the ground the Heel of the other foot and maintained a balance on one foot. The Stopwatch started when the Heel was lifted off the ground and stopped when one of the following errors occurred: hands raised off the iliac crest; the foot which on the knee separated from the knee, the foot that bears the weight is unbalanced, or the
Heel of the weight-bearing foot contacts the ground (Figure 4) (Armstrong, & Greig, 2018).
DYNAMIC BALANCE
A modified Y balance test was used to assess dynamic balance. The method of performing the test is that the subject was informed about the performance of the test through the researcher's explanations and performed the exercises several times before the first performance. In the first performance, the subjects stood on one foot in the center of the lines' intersection. Simultaneously, standing on one leg, the subject was asked to make achievements with his free foot in the anterior, internal posterior, external posterior have achievements. The test method is that the person stands on his right foot and performs the act of attainment three times in the anterior path and then stands on the left foot and performs attainment three times in the anterior path. Internal and external posterior trajectories were also repeated. The length of a person's foot affects the distance they reach. A normalized test, average access distance divided the length subject's foot multiplied by 100, the dependent variable calculated, and the access distance obtained percentage length foot (Armstrong, & Greig, 2018).
AGILITY
To evaluate the Agility and ability to redirect movement and speed and maintain balance and position perception, (Sivaramakrishnan, Fitzsimons, Kelly, Ludwig, Mutrie, Saunders, & Baker, 2019), a shuttle run test was used. To begin this test, the person stood at the starting line of a distance of 9 meters, with the examiner's command starting the test. In this test, the person ran the distance by touching the finish line with his foot, returning to the starting line and touching the starting line with his foot, repeating the same procedure with the difference in the second iteration, it quickly crossed the starting line. This test's duration is recorded in seconds as an individual record (Sivaramakrishnan, Fitzsimons, Kelly, Ludwig, Mutrie, Saunders, & Baker, 2019).
DATA ANALYSIS
Descriptive and inferential statistics used to analyze the research data. Descriptive statistics used to determine the table's mean and standard deviation. Shapiro-Wilk test was used to assess normal distribution of data, equality of variances tested by Bonferroni post hoc, the ANOVA and Bonferroni post hoc tests to compare subjects in four groups. Statistical analysis performed using SPSS24 software.
RESULT
`The mean and standard deviation of the subject characteristics. Including age, height, weight, and body mass index given in Table 1.
Descriptive information obtained from measuring the anomalies studied is presented in Table 2.
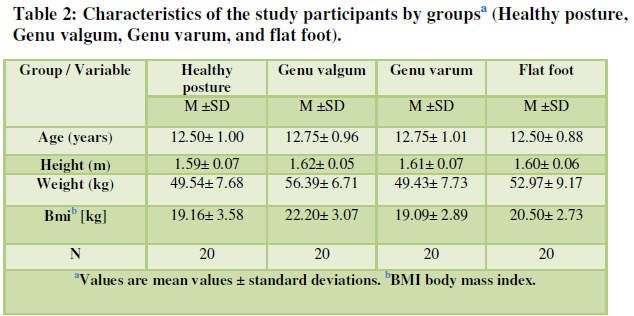
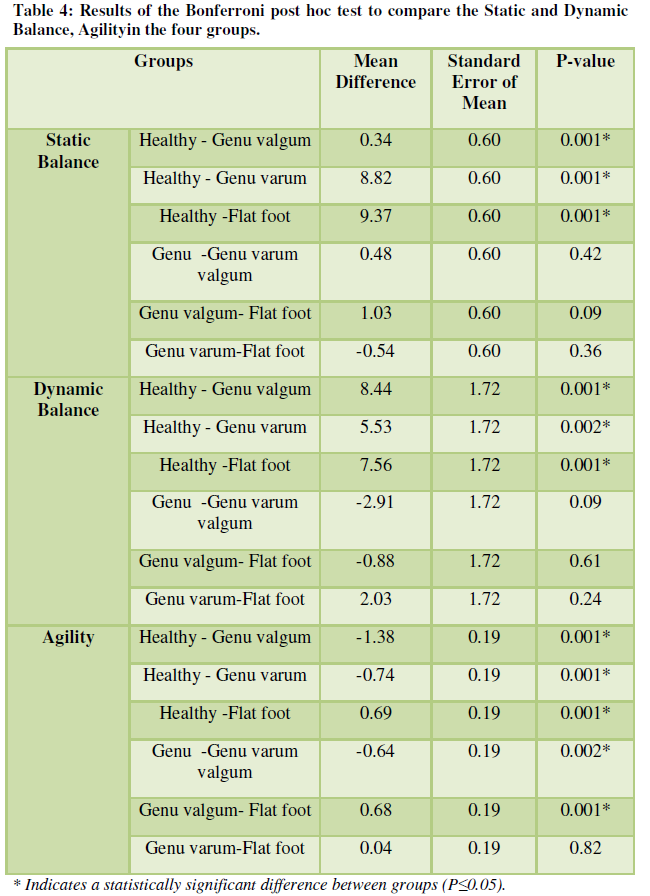
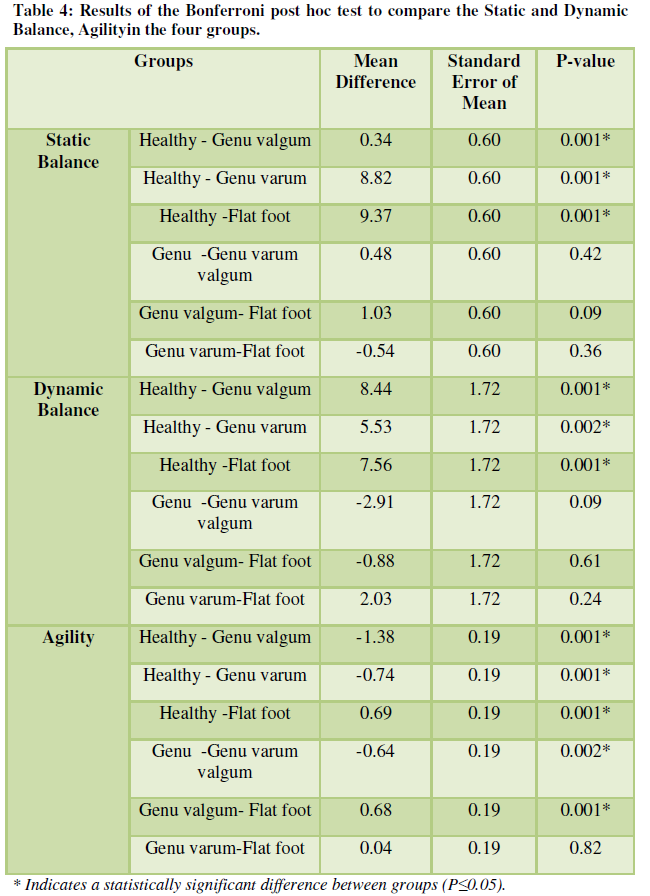
Table 3. Showed the results of the one-way ANOVA test to examine the mean scores of Static and Dynamic Balance, Agility tests in subjects. According to P-value (P≤0.01) between the Static Balance test scores during the trial, that shows a difference in the four groups.
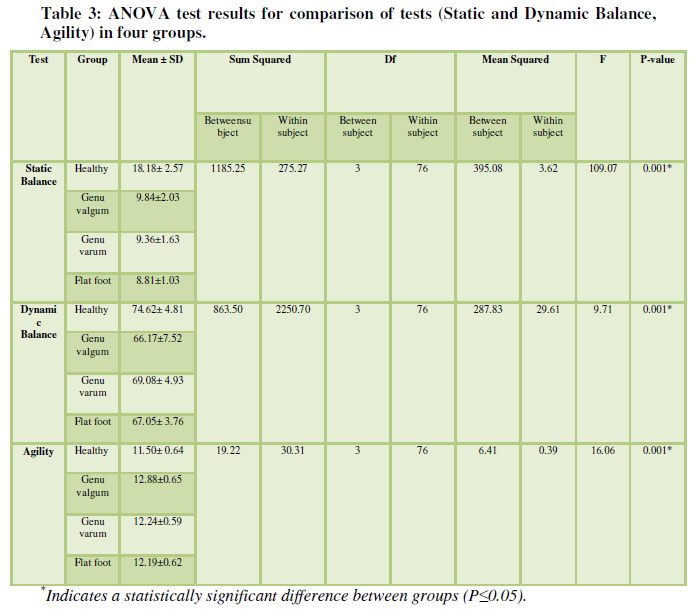
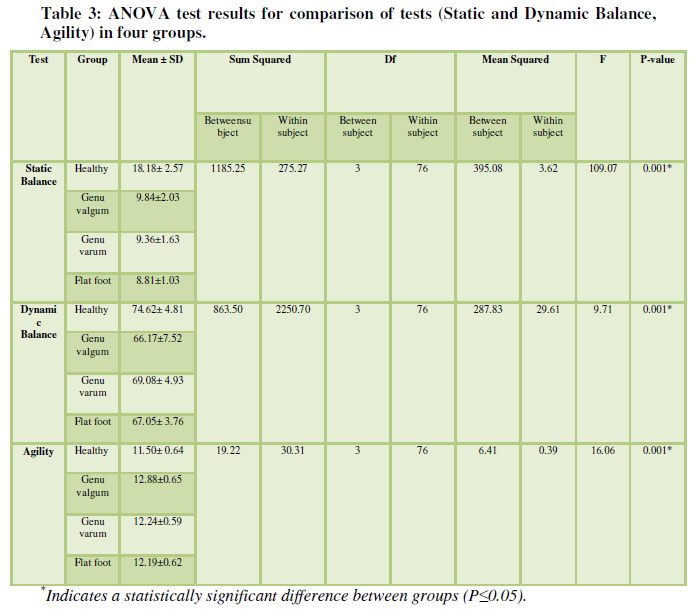
According to the Bonferroni test results in table 4, there was a meaningful difference in the static Balance test between Healthy groups and those with different abnormalities, while the performance of subjects in a Healthy group was better than the other three groups. The dynamic Balance variable also showed a significant difference between the Healthy groups and those with abnormalities, and the Agility of the Healthy group was better than the other three groups. Also, people with Genu valgum knee had the weakest performance in this test.
DISCUSSION AND CONCLUSION
Balance, as one of the controversial concepts of the sensory-motor system, examines the mutual connection and complex interplay between sensory inputs and the motor responses needed to maintain or change postural. The balance control system is a complex mechanism in which the co-ordination of three balance systems (Visual, Auricular and sensory body) plays an important role. The cooperation of these systems together results in postural control and balance. While standing up, the nervous system's central and peripheral components continually perform to maintain body alignment and COG at the level of support. The central nervous system processes the peripheral data within these systems and selects the most appropriate muscle response for postural control and body posture, showing the balance control system (Kumala, Tinduh, & Poerwandari, 2019).
As the disorder of this information leads to disruption of balance, for example, the disruption of visual information that plays an essential role in maintaining body position can impair the body's balance. Based on the coordinated performance of balance control systems, it is logical that people with abnormalities, when close their eyes in static balance tests, have weaker balance than Healthy ones. Since the foot is kept in a closed chain of motion and relies on the integrated feedback of the pelvic, knee, and ankle joint movements, the balance may be impaired by the impairment of mechanical strength and consistency of each joint or structure belonging to the lower extremity. Thus, since the foot forms the lowest part of the chain and provides a relatively small proportion of the support surface to maintain balance, it seems reasonable that even biomechanical changes in the support surface may be possible. It is likely to affect postural control (Ho, Lin, Chou, Su, Lin, 2000).
The foot's arches absorb the impulses and forces coming from the ground, so people with natural arches in the foot stand one foot longer than people with impaired arches, perform a locomotor activity, and get less tired. On the other hand, abnormalities affect the performance in static, dynamic, postural control systems, particularly body movement. Abnormalities may disrupt inputs from proprioception (Kumala, Tinduh, & Poerwandari, 2019). Flat foot may be associated with excessive subtalar pronation (for abnormal compensatory pronation may cause instability and excessive foot joint movement). Therefore, the flat foot may be unstable during weight-bearing and impair postural control (Cobb, Tis, Johnson, & Higbie, 2004).
According to the results, it can be seen that there is a significant difference between Agility in people with different lower extremity abnormalities and those without deformity. People with a deformity in the agility group performed weaker than those without deformity. This finding is in agreement with the results of Ho et al. (2000) and Di Twomey and McIntosh (2012) and disagreement with UNGER et al. (2000), Uden et al. (2017), and Kathleen et al. (2005).
UNGER et al. (2000), in their study of 118 male and female volunteers, concluded that there was no significant correlation between anthropometric measures and an average height of a jump from different leg positions, which is in disagreement with the results. One possible cause of this disagreement may be the age difference and how the Sargent jump is performed (UNGER, & WOODEN, 2000). Kathleen et al. (2005), in their study of people with a Q angle of more or less than the normal amount, concluded that increasing or decreasing this angle did not affect the performance of squat and knee valgus angle is in disagreement with these results. Possible causes of this discrepancy could be the type of subjects (people with a Q angle larger and lesser than usual) and the test (Single Leg Squat) (Kathleen, Pantano, White, Gilchrist, 2005).
The Quadriceps muscle is the primary knee extensor muscle that plays an essential role in leg muscle training, patellar stability, and knee flexion to be affected by the different direction of the knee joint. Electromyographic (EMG) studies have shown that the lower extremity muscles have an inequality pattern of performance when working in people with different knee alignments (such as the Genu valgum and Genu varum knee). A cross-sectional study of the quadriceps muscle in subjects with varying Q angles has shown that transverse areas of the external oblique muscle in people with a low Q angle (Genu varum) were greater than those of people with larger (Genu valgum) Q angle. These findings suggest that the difference in knee alignment may be related to abnormal quadriceps activity and the ratio status between quadriceps muscles. Sogabet et al. (2003) reported that the ratio of internal/external oblique muscle activity in individuals with normal knee alignment was natural (Sogabet, Catherine, Colleen, 2003).
Given lower extremity dysfunction, it is likely that the cause of poor performance in the Genu varum knee during the tests is related to the strength of the hip abductor muscles. Because of these tests, pelvic balance is maintained by these muscles, and since a reduction in the hip's strength muscles can be seen in people with a Genu varum knee. Their ability toperform these activities can reduce with decreased muscle strength (Mechael, 2001).
On the other hand, in vertical jump test, balance and pelvic control are very important, Again, the hip abductor muscles play a critical role in creating balance, and the weakness of these muscles leads to a decrease in balance (Pamela, Ghinwa, 2003). The hamstring and quadriceps muscle contraction also required during tests (Kathleen, Pantano, White, Gilchrist, 2005; Benjamin, 2010). Biomechanical and neuromuscular variables have also been in the vertical jump. Jacobsen et al. Stated that the two-joint muscles are crucial in jumping. The researchers identified that the force produced in the Rectus Femoris (RF) was transmitted from the femur to the knee joint, in contrast with the jump's kinematic analysis, which showed that the hamstring muscle shared the force generated from the knee to the femur (Benjamin, 2010).
As a result, the muscle contraction as opposed to the primary force transducer from the hip to the knee. The vertical jump is an explosive movement that engages the significant hip, knee, and ankle joints. In explosive movements, the force generated by the muscles transmitted to the joints in a short period, which is a vital variable responsible for the proper execution of a vertical jump. Early activity of biceps femoris (BF) muscles for the natural course of change can cause inappropriate vertical jump performance, which can simultaneously alter the motor force in the hip and knee joints during early biceps contraction. Jacobson et al. showed that the force transferred to the hip and knee requires synergy between the RF and BF muscles, which results in the optimal hip and knee extension necessary for a vertical jump to produce the optimal transitional force. Early BF muscle activity was observed before RF muscle activity in poor vertical jump performance, and because of reduced motor force produced in the hip and knee joints, compared to the onset of BR–RF activity in optimal vertical jump performance. Neuromuscular control of the two joint lower extremity muscles' muscles causes activity differences in individuals with different lower extremity alignments.
The early activity of BF causes impairment of performance and reduces motor force in hip and knee joints without optimal force transfer between them. In individuals with Genu varum and Genu valgum knees for a change in the quadriceps' direction tendon (QDT), this muscle decreases in performance, which may be one cause of poor performance in people with abnormalities (Kathleen, Pantano, White, Gilchrist, 2005). The present study results are roughly consistent with the results of Nyland, Smith, Beickman, Armsey, Caborn, 2002. Given the importance of the relationship between postural abnormalities and physical performance in people with these abnormalities, the importance of identifying and preventing physical corrective programs and promoting physical fitness is emphasized.
ACKNOWLEDGMENT
All authors contributed to this article. We thank our fellow citizens from [Tehran, Iran] who provided.
Conflict of interest
The authors have no conflict of interest.
Ethics approval and consent to participate
Ethical permission was given by the Human Ethics Committee at the University of kharazmi (IR.KHARAZMI.REC.1398.069) Iran. Before starting the study, the participant's assent and parent's written informed consent were obtained before starting the study. When the patient was under the age of 16, both parents and the child signed the informed consent.
Consent for publication
Not applicable.
Authors’ contributions
Hadi Mohammadi Nia initiated this study and collected all participants' materials in this study, and with the collaboration, Aisan Fard Mheregan analyzed and interpreted the result.
All authors read and approved the final manuscript.
Funding
No funding was received for performing this study.
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
- Winwood, P.W., Keogh, J.W., & Harris, N.K. (2012). Interrelationships between strength, anthropometrics, and strongman performance in novice strongman athletes. The Journal of Strength & Conditioning Research 26(2), 513-522.
- De Nunzio, A.M, Zanetti, C., Schieppati, M. (2009). Post-effect of forwarding and backward locomotion on body orientation in space during quiet stance. European Journal of Applied Physiology 105, 297-307.
- Zakeri, Y., Baraz, S., Gheibizadeh, M., & Saidkhani, V. (2016). Relationship between backpack weight and prevalence of lordosis, kyphosis, scoliosis and dropped shoulders in elementary students. International journal of pediatrics 4(6), 1859-1866.
- Michael, A.H., Trevor, B. (2009). Effect of tibial realignment surgery on a single standing balance in patients with knee osteoarthritis) clinical biomechanics, 24, 693-696.
- Mueller, M.J., (2005). The ankle and foot complex, Joint Structure and Function, a Comprehensive Analysis, 4th ed, 437-477.
- Delmonico, M.J., Harris, T.B., Lee, J.S., Visser, M., Nevitt, M., Kritchevsky, S.B., & Health, Aging and Body Composition Study. (2007). Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. Journal of the American Geriatrics Society 55(5), 769-774.
- Aurélio, F., Ronaldo, G., João, A., Rui, B., & Helena, M., (2010). The relationship of body mass index, age, and triceps-surae musculotendinous stiffness with the foot arch structure of postmenopausal women. Clinical Biomechanics 25, 588-593.
- Pamela S, Ghinwa H, (2003), Lower Extremity Abnormalities in Children, State University of New York–Downstate Medical Center, Brooklyn, New York, 68, 3.
- Uden, H., Scharfbillig, R., & Causby, R. (2017). The typically developing paediatric foot: How flat should it be? A systematic review. Journal of foot and ankle research 10(1), 1-17.
- Cassio, M. (2011). Misalignment of the knee, Dose it affect human stability. Journal of Bodywork & Movement Therapies 15, 235-241.
- Ian R, Gavin, C. (2009). Evaluation of the limping child. 48, 587-90.
- Kirby, R.L, Price, N.A, MacLeod, D.A, (1987). The influence of foot position on standing balance. Journal of Biomechanics 20(4), 423-427.
- Abrigh, H.S., & Moghaddami, A. (2020). The corrective effect of an NASM based resistance exercise on genu varum deformity in teenage football players. DYSONA-Life Science 1(1), 14-19.
- Chavoshnejad, P., Ayati, M., Abbasspour, A., Karimpur, M., George, D., Rémond, Y., & Baniassadi, M. (2018). Optimization of Taylor spatial frame half-pins diameter for bone deformity correction: Application to femur. Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine 232(7), 673-681.
- Armstrong, R., & Greig, M. (2018). The Functional Movement Screen and modified Star Excursion Balance Test as predictors of T-test agility performance in university rugby union and netball players. Physical Therapy in Sport 31, 15-21.
- Sivaramakrishnan, D., Fitzsimons, C., Kelly, P., Ludwig, K., Mutrie, N., Saunders, D.H., & Baker, G. (2019). The effects of yoga compared to active and inactive controls on physical function and health related quality of life in older adults-systematic review and meta-analysis of randomised controlled trials. International Journal of Behavioral Nutrition and Physical Activity 16(1), 33.
- Kumala, M.S., Tinduh, D., & Poerwandari, D. (2019). Comparison of Lower Extremities Physical Performance on Male Young Adult Athletes with Normal Foot and Flatfoot. Surabaya Physical Medicine and Rehabilitation Journal 1(1), 6-13.
- Ho, C.S., Lin, C.J., Chou, Y.L., Su, F.C., Lin, S.C. (2000). Foot progression angle and ankle joint complex in preschool children. Clinical Biomechanics 15(4): 271-277.
- Cobb, S.C, Tis, L.L, Johnson, B.F., Higbie, E.J. (2004). The effects of forefoot varus on postural stability. Journal of Orthopaedic and Sports Physical Therapy 34, 79-85.
- UNGER, C.L., & WOODEN, M.J. (2000). Effect of foot intrinsic muscle strength training on jump performance. The Journal of Strength & Conditioning Research 14(4), 373-378.
- Kathleen, J., Pantano S.C., White, L., & Gilchrist, J.L., (2005). Differences in peak knee valgus angles between individuals with high and low Q-angles during a single limb squat. Clinical Biomechanics 20, 966-972.
- Sogabet, A., Catherine, M., & Colleen, G., (2003), A Genu Varum Effects on Each Lower Extremity Muscle Activity During Leg Press Exercise. Tairyoku kagaku. Japanese Journal of Physical Fitness and Sports Medicine 52(3), 275-284.
- Mechael, Y. (2001). A review on postural realignment and its muscular and neural component. Archives of Physical Medicine and Rehabilitation 82(2), 205-209.
- Benjamin, J. (2010). Toe walking, flat feet and bow legs, in-toeing and out-toeing. Paediatrics and Child Health 20, 131-136.
- Nyland, J., Smith, S., Beickman, K., Armsey, T., & Caborn, D.N. (2002). Frontal plane knee angle affects dynamic postural control strategy during unilateral stance. Medicine & Science in Sports & Exercise 34(7), 1150-1157.






