Research Article
Operation Theatre Time Utilization in SMHS Hospital, a Tertiary Level Teaching Hospital in Kashmir Valley
5113
Views & Citations4113
Likes & Shares
Operation theatres are an important but limited resource in any hospital. This is especially true in a setting like ours where the number of hospitals providing surgical services is even as such less as compared with the large population. This puts tremendous strain on Operation Theaters as a resource. Operation theater time utilization is an important indicator of the use of this limited resource. With long waiting lists it become imperative to evaluate available operation theater resources and study ways to maximize their usage.
INTRODUCTION
The concept of cost effectiveness and optional utilization of resources is becoming increasingly important in health care management. Although hospitals have traditionally been the major consumers of health care resources, they have not been a focus of health policy and research in developing countries [1].
On an average 50-80 % of the public health resources in terms of money as well as trained personnel are used in hospitals [1]. It has been observed that a considerable portion of these resources are wasted because of the technical and management inefficiency in the hospitals.
Operation theatres are the pride of any good hospital and account for considerable expenditure of hospital budget and human resources. A theatre complex typically consumes 9-10% of the hospital budget [2]. Thus, operation theatres require maximum utilization of resources to ensure optimum cost-benefit [3]. The efficient use of operation theatre time is also important to clear waiting lists [4]. It has been observed that Operation theatres are usually under-utilized and lie idle most of the time and many patients who are scheduled for operation get postponed. This assumes even greater importance in a developing country like ours where even as such waiting lists tend to be long because comparatively fewer hospitals are available to cater to large population groups.
Analysis of the time spent on various activities in the operation theatres thus becomes imperative as it can lead to an improvement in the utilization of operation theaters.
This study was carried out at SMHS Hospital Srinagar which is a 750 bedded teaching hospital associated with the Government Medical College Srinagar, Kashmir. The aim of this study was to find out the extent of under- utilization of time in the operation theatres and suggest measures to decrease the unproductive time in the theatres. To this end the time spent in performing the various surgical procedures as well as the time spent in the supportive services and in preparation of the operation theatres was calculated.
AIMS AND OBJECTIVES
To study the actual time spent in performing the various surgical procedures and the time spent in support services associated with the surgery and in preparation of the operation theatres.
- To determine the extent of under-utilization of time in
the operation theatres and suggest measures to decrease the unproductive time spent in the theatres.
MATERIAL AND METHODS
A prospective yearlong study was conducted in the operation theatres of SMHS Hospital Srinagar. There are four operation theatre suites in the hospital, two for general surgery and one each for ENT and Ophthalmology. In addition, there is an Emergency / Trauma theatre suite which was not included in our study because it was based on elective surgeries only.
To streamline the study a random sampling of the operation days and operation lists was done selecting a total of 75 operation days/ operation lists each from general Surgery, ENT and Ophthalmology theatres.
A proforma was developed, pre-tested and standardized to record the following observations in all the operation theatres.
- Time at which the operation theatre is ready for the first case.
- Time of receiving the first patient in the operation theatre.
- Time of induction by the anesthetist.
- Time of the commencement of surgery.
- Time at the completion of surgery.
- Time when the first patient leaves the theatre.
- Time involved between the first patient’s leaving and the second patient’s entrance (Turnover period).
- Time at which operating room is ready for the next patient.
- Time at which surgery starts
- Time spent on actual surgery (preparing the part to closure of wound) was noted. Time spent on supportive services (time which is spent on laying out sterile trolley, sponges and also time spent on anaesthetizing the patient) was recorded.
- Time spent on making room ready (time spent in cleaning the room, disposing off used linen, removing tissues sponges etc.) both at the start of the day and between cases was also recorded.
- Time not spent on any of the above activities, i.e., idle time was also recorded.
RESULTS
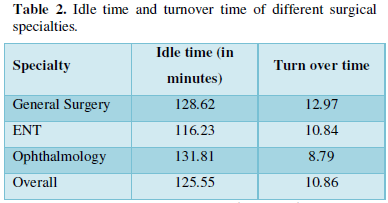
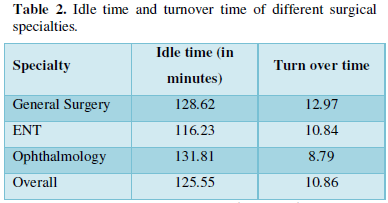
The data obtained has been analyzed and summarized in the form of Tables 1 & 2.
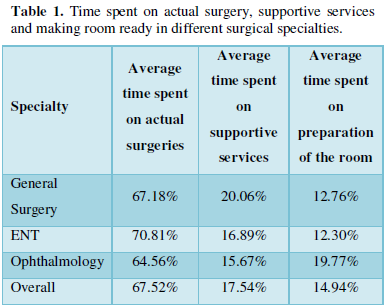
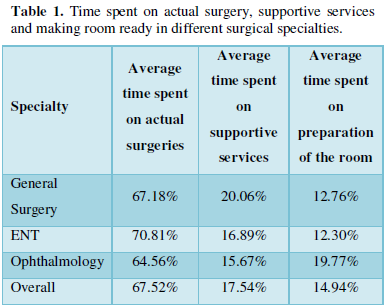
Time spent on actual surgery includes time duration from preparing the part to be operated till closure of the wound.
Time spent on supportive services includes the time spent on anaesthetizing the patient, laying out the instrument trolley and sponges etc.
Time spent on making the room ready includes the time spent in cleaning the room, disposing off the used linen, removing used sponges and tissues etc.
Idle time includes the time not spent on any of the surgery related activity; i.e., unproductive time.
Turnover time includes the time gap between the exit of one patient and the entrance of another.
Analysis of variance showed that the difference in the time spent on actual surgery between different surgical specialties is statistically significant (P< 0.05).
Analysis of variance showed that the time spent on actual surgery in different specialties is statistically significant (P< 0.05).
The difference in making the operation theatres ready in the different surgical specialties was found to be significant on the basis of analysis of the variance recorded as P< 0.05.
The difference in the idle time between the different surgical specialties was not statistically significant (P> 0.05).
DISCUSSION
We found that the time spent on actual surgery in various specialties averaged around 67.52% (varying between 64.56% to 70.81%; average time spent on supportive services was 17.54% (varying between 15.67% to 20.06% whereas on an average 14.94% of the time was spent in getting the theatre ready for surgery (ranging between 12.30% to 19.77%). A similar study elsewhere has shown that about 54% of the theatre time was spent in performing the surgical procedures whereas the time spent on supportive services was 31% and the time spent in preparing the theatres was 15% [5].
A study conducted in the Orthopedic theatres of Central Middle-Sex Hospital, London showed that 60% of elective list time was used for operating, 21% for turnover and no useful activity occurred during the remaining 19% of theatre times [4]. Of the general surgery session time in the same hospital 49% was found to be used for performing operations [4].
We found during our study that considerable variations were observed in the percentage of time spent on actual surgery, supportive services and on making room ready for surgery in different surgical specialties. Statistically this difference was found to be significant (p<.05). This statistically significant difference can be attributed to the type of the surgeries performed as case lengths vary in the General Surgery, ENT and Ophthalmology theatres.
Productivity in an operation theatre has been defined as surgical time divided by the total work hours of the operation room staff [6]. This productivity factor is normally reduced in the case of operations that take only a short time to perform, since the time interval between operations is usually not reduced correspondingly [6]. In a survey conducted in the unit for outpatient surgery at the Norwegian Akershus Central hospital, it was found that 4.6 operations were performed daily in 206 days in 1993, with a productivity factor of 42% and an operating theatre utilization of 66% (Operating theatre time spent on specific patients/total operating theatre time) [6]. The mean interval from the time the surgeons finished one operation until they could start the next was 33 min (confidence interval 32-34) with a mean operating time of 44 min (42-46) [6].
The mean idle time in our study was 125.55 min/day. There was no statistically significant variation in the idle time of different surgical specialties (p>.05), which indicates that this unproductive time has nothing to do with the type of the surgery being performed. The causes of this idle time need to be identified and corrected as they cannot be attributed to the surgical procedures themselves. In another study conducted in the surgical unit of a large teaching hospital idle time of 105 min on an average has been recorded [7]. Researchers have found operating room utilization rates to be low overall, ranging between 40 and 60%, in widely varying settings in Chicago [8], Columbia [9] and United States Department of veteran affairs [8]. In another study utilization was found to be ranging from 44% to 113% [7]. Audit of surgical theatre utilization at Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India which was done prospectively over a period of 12 months with respect to the starting and closing of the operation theatre, interval between surgical procedures and cancellation of surgical procedures showed that theatre was functional for 279 days during the year of the study, and 1773 cases were operated (6.3 cases/day) [3]. The total operating time utilization was 91.5%. The major reasons for cancellation of a total of 310 cases were lack of operating time (65.2%), emergency surgery during the elective cases (13.9%) and preoperative lack of fitness (11.3%). 2 Among all the lists, 43.6% started late and 63.6% of lists finished well before the scheduled closing time [3]. Absence of monitoring equipment and non-availability of additional qualified anesthetists necessitated induction of anesthesia in the main operating room and accounted for 11% of the total operating time [3]. An audit of the usage of operating theatre in Eastern General Hospital Edinburgh found that twenty five percent of theatre sessions were not allocated for use, twenty three percent of general surgical lists were cancelled and of the lists which did take place, a further twenty three percent of theatre time was not utilized [10]. A report by the National audit office UK showed only 50% to 60% of weekday operating time was being used [10]. This report was examined by the committee of public accounts and much of the blame for underutilization of operation theatres was attributed to poor working practices among surgeons [10]. A study at Central Middlesex Hospital London showed only 9/151 (6%) of lists started within 5 min of the scheduled time [4]. Of unnecessary delays contributing to this, 63% involved anesthetic staff and 24% theatre staff. Surgeons were implicated in 10% of start delays [4]. There were less start delays if senior anesthetic staff were present [4]. In a study patients seen at assessment clinics within two months before admission had a significantly higher operation rate than those admitted from a routine waiting list. Patients on long waiting lists for surgery need to be reassessed before admission to avoid wasting theatre opportunities by cancellation of cases [11].
Turn-over time of 10.86 min was recorded on an average in our study. In studies conducted in other hospitals room turnaround time was almost uniformly 36 min [12]. In our study it was seen that most of the time is wasted at the start of the day and at the end rather than between cases. Shorter turnaround times may also sometimes indicate compromise on the cleanliness of the theatre. In one study turnaround times were quicker if a consultant surgeon was present [4].
CONCLUSIONS
It was found during our study that even with certain existing lacunae and constraints the OT time utilization is optimum as per the available literature. However, in spite of this optimum utilization, long waiting lists in every surgical discipline are a reality leading to dissatisfaction and discontentment among patients as well as doctors. In spite of the various parameters falling within accepted norms and comparing favorably with other studies we concluded that there always exists room for further improvement.
It was observed that the causes of idle time were mainly unplanned scheduling of operations, delayed starts and cancellation of cases. It is possible to increase effective use of theatre time if delays in starting lists are minimized and a proper scheduling of surgical lists is done. We also concluded that a more detailed assessment of the patients to be operated should be undertaken by the anesthetists well before the date of scheduled surgery, as well as a more thorough work-up of the patients done by the admitting units ruling out any cause that might lead to cancellation of cases at the eleventh hour.
It is also recommended that the induction as well as recovery of the patient should be done in a separate anesthesia room instead of the operating room which would reduce the time spent on supportive services. This should be weighed against the need for two qualified anesthetists to alternate between cases and proper monitoring equipment being available in the anesthesia induction/recovery room. The laying out of sterile trolleys should similarly be done in a separate lay-up room instead of the operating room which would again reduce the time spent on supportive services. The time spent on making the operation theatres ready, both at the start of day and in between cases, can also be reduced but this should in no way compromise aseptic precautions National Health Services Management Board has pointed out that full utilization of operation theaters would involve the recruitment of considerable numbers of staff, the provision of substantial numbers of extra beds as well as a substantial amount of extra funding [13].
- Tabish SA (1998) Towards development of professional management in Indian hospital. J Manag Med 12(2): 109-119.
- WHO (1966) MaCaulay, HMC and Davies LL. Hospital planning and Administration.
- Vinukondaiah K, Ananthakrishnan N, Ravishankar M (2000) Audit of operation theatre utilization in general surgery. Natl Med J India 13(3): 118-121.
- Ricketts D, Hartley J, Patterson M, Harries W, Hitchin D (1994) An orthopedic theatre timing survey. Ann R Coll Surg Engl 76(3): 200-204.
- Sakharkar BM (1998) Operation theatre Suite; In Principles of Hospital Administration and Planning. 1st Jaypee Bros, New Delhi. Vol: 14, pp: 197-207.
- Hoel TM, Steen PA (1996) Utilization of a unit of ambulatory surgery. Tidsskr Nor Laegeforen 116(3): 376-378.
- Sinha R.K (1987) A study to assess staffing requirement of doctors in surgical unit of a large hospital. Tehesis for M.H.A, AIIMS.
- McQuarrie DG (1981) Limits to efficient operating room scheduling: Lessons from computer? Use models. Arch Surg 116: 1065-1071.
- Gil AV, Galarza MT, Guerrero R, deVeleez GP, Peterson OL, et al. (1983) Surgeons and operating rooms: underutilized resources. Am J Public Health 73: 1361-1365.
- Haiart DC, Paul AB, Griffiths JM (1990) An Audit of the usage of operating theatre time in a peripheral teaching surgical unit. Postgrad Med J; 66(780): 612-615.
- Mangan JL, Walsh C, Kernohan WG, Murphy JS, Mollan RA, et al. (1992) Total Joint replacement: Implication of cancelled operations for hospital costs and waiting list management. Qual Health Care 1(1): 34-37.
- Mazzei WJ (1994) Operating room start times and turn over times in a university hospital. J Clin Anaesth 1994: 405-408.
- National Centre for Health Statistics (1999) Health, United States, 1999 with health and aging chart book (DHSS Publication No. PHS99-1232). Hyattsville, MD: National Centre for Health Statistics.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Genomic Medicine and Pharmacogenomics (ISSN:2474-4670)
- Journal of Womens Health and Safety Research (ISSN:2577-1388)
- Journal of Astronomy and Space Research
- Advances in Nanomedicine and Nanotechnology Research (ISSN: 2688-5476)
- Journal of Veterinary and Marine Sciences (ISSN: 2689-7830)
- Journal of Genetics and Cell Biology (ISSN:2639-3360)
- Food and Nutrition-Current Research (ISSN:2638-1095)


