1280
Views & Citations280
Likes & Shares
CASE REPORT
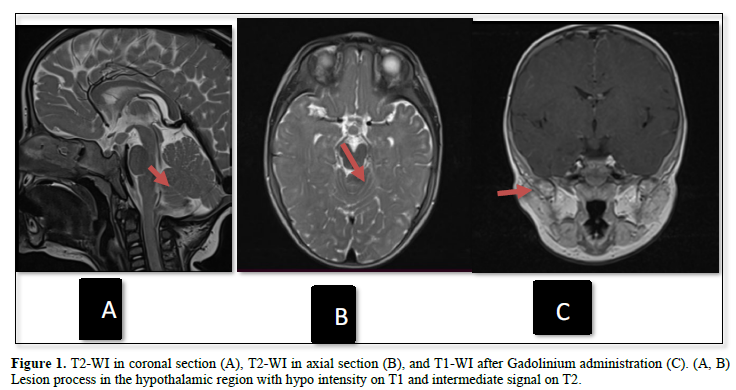
This is an 11-month-old female infant from a consanguineous marriage, with no significant medical history. Symptoms began one month ago with the occurrence of uterine bleeding. Clinical examination revealed signs of estrogenization with the development of pubertal characteristics. Laboratory tests showed elevated levels of LH and estradiol. An MRI of the hypothalamic-pituitary region was performed, revealing a suprasellar mass located posterior to the tuber cinereum and in contact with the mammillary bodies. The mass was roughly oval, well-defined, with regular contours, isointense on T1-weighted images, intermediate signal on T2-weighted images, without restriction on diffusion sequences, and not enhanced after gadolinium injection, consistent with a hypothalamic hamartoma (Figure 1).
DISCUSSION
Hypothalamic hamartomas (HH) are rare congenital malformations that consist of a mixture of neurons and glial cells [1]. With an estimated prevalence of approximately 1 in 100,000 live births. These lesions are more frequently diagnosed in girls than in boys, although the reasons for this sex predisposition are not yet well understood [2]. These benign lesions, which are typically located near the hypothalamus, can lead to notable clinical manifestations, including central precocious puberty, gelastic seizures, and cognitive impairment in some cases [1,3]. Central precocious puberty (CPP), a hallmark of HH, is marked by the early activation of the hypothalamic-pituitary-gonadal (HPG) axis, resulting in premature development of secondary sexual characteristics. The association between HH and CPP is particularly concerning due to the lesion's capacity to induce the early release of gonadotropin-releasing hormone (GnRH), which accelerates pubertal development [4].
The diagnosis of HH is primarily made through neuroimaging, with magnetic resonance imaging (MRI) as the gold standard for identifying the typical features and location of these lesions [5]. Treatment often involves the use of GnRH agonists to manage early puberty, with surgical intervention considered in cases of neurological complications or uncontrolled seizures [6].
Precocious puberty, defined as the development of secondary sexual characteristics before the age of 8 in girls and before 9 in boys, represents a significant clinical challenge. It is crucial to use neuroimaging to identify any underlying organic causes, even if they are rare. Hypothalamic hamartomas (HH) are a potential cause of central precocious puberty, and their identification requires a thorough understanding of imaging characteristics and associated symptoms [2].
Hypothalamic hamartomas are rare and benign congenital anomalies composed of neurons and glial cells, primarily located in the tuber cinereum or mammillary bodies. These heterotopic lesions typically present with a combination of symptoms: precocious puberty, gelastic seizures (involuntary laughter), dacrystic seizures (involuntary crying), and occasionally intellectual deterioration [7]. Magnetic resonance imaging (MRI) is the diagnostic tool of choice for these lesions. Hypothalamic hamartomas generally show iso-intensity on T1-weighted images, slight hyperintensity on T2 and FLAIR sequences, and typically no enhancement after gadolinium injection, which is an important distinguishing feature [8].
Treatment of hypothalamic hamartomas primarily involves a medical approach. LH-RH agonists are used to manage precocious puberty, while anti-epileptic drugs are administered if seizures are present. Surgery is considered mainly in cases of progressive neurological deficits, hydrocephalus, or frequent epileptic seizures resistant to medical treatment. Regular follow-up, generally every 6 months after diagnosis, is crucial to assess disease progression and adjust treatment as necessary [9-10].
It is also essential to differentiate hypothalamic hamartomas from other brain pathologies that may present with similar symptoms. Hypothalamic gliomas, particularly pilocytic gliomas, should be considered in the differential diagnosis. These tumors may show iso-intensity on T1-weighted images and moderate hyperintensity on T2-weighted images, but they are distinguished by significant contrast enhancement after gadolinium injection, which is rare in hamartomas. Gliomas may also exhibit signs of tumor growth and invasion of surrounding structures [8].
Vascular malformations, such as arteriovenous malformations (AVMs), are another pathology to consider. AVMs in the hypothalamic region typically present with well-defined vascular architecture and marked contrast enhancement on MRI and MR angiography. They may also be associated with signs of hemorrhage or calcifications, which helps distinguish them from hypothalamic hamartomas, which generally do not show these features [10-11]. Venous malformations often present with diffuse contrast enhancement and a "honeycomb" appearance. Signs of hemorrhage or marked vascular anomalies observed on MRI assist in differentiating them from hypothalamic hamartomas [11].
Finally, Dandy-Walker malformation is a congenital condition to consider in the differential diagnosis. This malformation is characterized by abnormalities in the cerebellar region and may be associated with signs in the hypothalamic region. MRI reveals abnormalities in the cerebellar structure and a cyst of the fourth ventricle, which helps differentiate this malformation from hypothalamic hamartomas, which are specifically located in the tuber cinereum [12].
By considering these specific imaging characteristics and associated clinical signs, it is possible to differentiate hypothalamic hamartomas from other brain pathologies, ensuring accurate diagnosis and appropriate treatment.
CONCLUSION
Hypothalamic hamartomas, although rare, require precise identification via MRI due to their distinctive imaging characteristics. It is essential to differentiate them from other brain pathologies such as gliomas and vascular malformations for appropriate treatment. Management generally involves LH-RH agonists and anti-epileptic medications, with surgery considered in severe cases. Regular follow-up is crucial to adjust treatment based on disease progression.
- Regis J, Lagmari M, Carron R, Hayashi M, McGonigal A, et al. (2007) Safety and efficacy of Gamma Knife radiosurgery in hypothalamic hamartomas with severe epilepsies: A prospective trial in 48 patients and review of the literature. Epilepsia 2: 60-71.
- Hirayama K, Tada K, Tominari S (2011) Hypothalamic Hamartoma: Clinical Features, Diagnosis, and Management. Child's Nervous System 27: 1185-1190.
- Benyakhlef S, Messaoudi N, Rouf S (2020) Hypothalamic hamartoma revealed by precocious puberty: Case report. CHU Mohammed VI, Faculty of Medicine and Pharmacy, University Mohammed Premier, Oujda, Morocco.
- Mounach J, Abilkassem R, Zerhouni A, Satté A, Bourazza A, et al. (2010) Puberté précoce liée à un hamartome hypothalamique. Service de Neurologie et Neurophysiologie. Clinique de l’hôpital militaire.
- Wilfong AA, Curry DJ (2013) Hypothalamic hamartomas: optimal approach to clinical evaluation and diagnosis. Epilepsia 9: 109-114.
- Ilvesmäki V, Savinainen A (2020) Neuroimaging in Hypothalamic Hamartoma-Induced Precocious Puberty. Pediatric Radiology.
- Verrotti A, Manco R, De Palma M (2015) Hypothalamic Hamartomas and Central Precocious Puberty: A Review of Clinical Presentation and Treatment. Epilepsy Behav 52(Pt A): 292-298.
- Choi JH, Hwang HS (2019) MRI of Hypothalamic Hamartomas: A Review of Imaging Features and Differential Diagnosis. J Magn Reson Imaging 50(3): 721-731.
- Reni M, Vecht CJ (2012) Management of Hypothalamic Hamartomas: Clinical Experience and Treatment Guidelines. Neuro Oncol 14(5): 658-669.
- Rosenberg R, Engel J Jr. (2020) Imaging and Management of Hypothalamic Tumors: Insights and Challenges. Epilepsy Res 166: 106443.
- Thomas SR, Becker D (2021) Vascular Malformations in the Hypothalamic Region: Diagnostic Imaging and Clinical Implications. Neuroradiology 63(8): 1241-1252.
- Kothari S, Gupta P (2018) Dandy-Walker Malformation: Radiologic Features and Differential Diagnosis. J Pediatr Neurosci 13(2): 150-156.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- BioMed Research Journal (ISSN:2578-8892)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)






